Abstract
Purpose
We assessed the uptake of fertility preservation (FP), recovery of ovarian function (OFR) after chemotherapy, live birth after breast cancer, and breast cancer outcomes in women with early-stage breast cancer.
Methods
Women aged below 41 years and referred to our center for FP counseling between 2008 and 2015 were included. Data on patient and tumor characteristics, ovarian function, cryopreservation (embryo/oocyte) and transfer, live birth, and disease-free survival were collected. Kaplan–Meier analyses were performed for time-to-event analyses including competing risk analyses, and patients with versus without FP were compared using the logrank test.
Results
Of 118 counseled women with a median age of 31 years (range 19–40), 34 (29%) chose FP. Women who chose FP had less often children, more often a male partner and more often favorable tumor characteristics. The 5-year OFR rate was 92% for the total group of counseled patients. In total, 26 women gave birth. The 5-year live birth rate was 27% for the total group of counseled patients. Only three women applied for transfer of their cryopreserved embryo(s), in two combined with preimplantation genetic diagnosis (PGD) because of BRCA1-mutation carrier ship. The 5-year disease-free survival rate was 91% versus 88%, for patients with versus without FP (P = 0.42).
Conclusions
Remarkably, most women achieved OFR, probably related to the young age at diagnosis. Most pregnancies occurred spontaneously, two of three women applied for embryo transfer because of the opportunity to apply for PGD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most commonly diagnosed malignancy in women, with approximately 12% of the women affected being younger than 40 years of age [1]. In these patients, (neo)adjuvant chemotherapy is frequently recommended, as younger age is an independent risk factor for an unfavorable outcome [2]. In patients at a reproductive age, chemotherapy may lead to premature ovarian insufficiency and subsequently to impaired fertility [3, 4]. With the currently used chemotherapy regimens the risk of permanent chemotherapy-induced ovarian function failure is on average 20% in patients below 40 years of age [3,4,5].
Considering the trend towards postponing the age of becoming pregnant, the number of women without children at diagnosis of breast cancer is increasing [6]. Moreover, at breast cancer diagnosis, it is generally recommended to postpone pregnancy for 2 years to allow resumption of adequate ovarian function and because of the relatively high risk of recurrence in this period [7].
Infertility following cancer treatment has a recognized negative impact on quality of life [8]. The prospect of loss of fertility has been reported to influence the choice of and adherence to a prescribed systemic treatment in over a quarter of cases [9,10,11,12]. International guidelines recommend that oncologists address the possibility of future infertility with patients with newly diagnosed cancer in their reproductive years [7, 13, 14]. Despite these guidelines, the likelihood of discussions regarding fertility preservation, among others, is influenced by unfamiliarity with fertility preservation processes, risks, and outcomes [15]. Patients should be referred as early as possible to specialists who can offer fertility preservation (FP). Initiation of a program with information about cancer treatment-related fertility issues and FP options has shown to significantly improve patient satisfaction [16, 17]. In our university hospital in the Southeast of the Netherlands, a FP program has been offered since 2008. The current study aimed to evaluate the uptake of FP in patients referred for counseling at breast cancer diagnosis and to assess fertility, live birth after breast cancer, and breast cancer outcome during follow-up.
Methods
Patients and study design
We performed a prospective cohort study in patients who visited the Maastricht University Medical Centre for counseling on FP in the years 2008–2015. Premenopausal patients aged under 41 years with stage I–III invasive breast cancer with an indication for adjuvant or neoadjuvant systemic treatment who were potentially interested in FP were referred. Patients were offered the option of embryo and/or oocyte cryopreservation. None of the patients received prophylactic GnRH analogs during chemotherapy. Our controlled ovarian stimulation protocol is according to the protocol described by Oktay et al. and von Wolff et al. [18, 19] According to the Netherlands Central Committee on Research Involving Human Subjects guidelines, this observational study is not subject to the Act on Medical Research Involving Human Subjects.
Data collection
For each patient, the following characteristics were collected: date of first visit, age, gene mutation status and date, (male) partner at time of diagnosis, age and number of children at diagnosis if applicable, known infertility before treatment, primary tumor characteristics, type of local breast cancer treatment, chemotherapy, human epidermal growth factor receptor 2 (HER2)-targeted therapy and endocrine therapy if applicable, choice of FP procedure, number of oocytes retrieved, and number of embryos and oocytes frozen. During follow-up, we collected data on OFR, date of live birth, date of last update, first local, regional or distant breast cancer recurrence or the occurrence of a contralateral breast cancer, and survival status. Data collection from the medical files was last updated in 2018, therefore the follow-up duration was at least 2 years.
Study objectives
We aimed to assess the uptake of FP in young women with early-stage breast cancer referred for counseling to the Maastricht University Medical Centre from 10 affiliated centers in the Southeast of the Netherlands in the years 2008–2015, and to assess the OFR-rate after end of chemotherapy, the live birth rate, and the disease-free survival rate since the date of counseling.
Definitions
Premenopausal status at counseling was based on a history of regular menstruation. In patients using oral contraceptives, we presumed a premenopausal status based on a regular menstrual cycle before oral contraceptive use and the young age at counseling [20]. Furthermore, before the start of hyperstimulation, we performed a vaginal ultrasound to count the antral follicles and measured Anti-Mullerian Hormone to predict the ovarian reserve. Uptake of FP was defined by the number of women who underwent FP as numerator and the number of counseled women as denominator. Premenopausal status after chemotherapy (OFR) was based on menstrual cycles and/or premenopausal lab values. History and FSH/17-ß-estradiol assessments were locally performed at the end of chemotherapy and 3-monthly thereafter. Time to OFR was defined as the interval from the end of chemotherapy to the date of premenopausal status confirmation (set at 0.1 months if present at the end of chemotherapy). Hence, OFR is a composite endpoint consisting of both recovery and maintenance of ovarian function during chemotherapy, as one may consider it equally relevant from a patient perspective when estimating on forehand the risk of infertility. The rate of live birth was defined as the percentage of women that gave birth to one or more babies excluding still birth and miscarriage. The time to live birth was defined as the interval from the date of counseling to the first live birth. The mode by which the pregnancy leading to live birth was achieved was categorized as either spontaneous, by use of earlier cryopreserved embryos or oocytes, or by fertility treatments. The period of disease-free survival was defined as the interval from the date of counseling to ipsilateral invasive breast tumor recurrence, regional breast cancer recurrence, distant recurrence, contralateral breast cancer, second primary non-breast invasive cancer, or death attributable to any cause, whichever occurred first [21].
Statistical analysis
Baseline characteristics of the FP group and the non-FP group were compared using independent samples Student t tests for normally distributed continuous variables, the Mann–Whitney-U test for skewed continuous variables, and the chi-square test for categorical variables. Kaplan–Meier analyses were performed for OFR (one minus Kaplan–Meier estimator) and disease-free survival, for disease-free survival comparing the FP group and the non-FP group by using the logrank test. Cumulative incidence of live birth was determined using competing risk analyses. For the endpoint of OFR, patients were censored at the date of ovariectomy, start of gonadotropin-releasing hormone treatment in the absence of OFR, recurrent disease or last follow-up. In patients with OFR for whom the exact date of OFR was not known (n = 13), we assumed the group median as time to OFR to prevent exclusion of these patients and an underestimation of the OFR-rate. For the endpoint of live birth rate, patients were censored at the end of follow-up. The occurrence of a disease-free survival event and ovariectomy, both hindering the observation of live birth, were therefore considered as competing risks. All statistical analyses were performed with SPSS 22.0 and STATA 14.1. A P value of < 0.05 was considered statistically significant.
Results
Patient characteristics
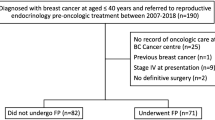
In the period 2008–2015, 125 women with the diagnosis of early breast cancer were referred for FP counseling. After excluding seven patients because of several reasons, 118 patients were analyzed in this study (Fig. 1).
Patient, tumor, and treatment characteristics are shown in Table 1. The median age of the counseled women was 31 years (range 19–40). At diagnosis, 75% of patients had a male partner and 31% had one or more children. Of all patients, 84% were analyzed for germline mutations. In 19% of patients, a germline mutation was present, corresponding with 23% of tested patients. The median tumor size was 22 mm (range 7–100) with slightly more than half of the patients having lymph node-negative disease. Almost two-third of the patients had a grade III tumor. The hormone receptor status was positive in 53% and the HER2 status was positive in 25%. The median follow-up in the FP group was 52 months (95% confidence interval (CI) 48–58), the median follow-up in the non-FP group was 51 months (95% CI 42–63).
Uptake of fertility preservation
Thirty-four (29%) women underwent FP before the start of chemotherapy. Patients who underwent FP had less often children (85% versus 63%, P = 0.03), more often a male partner (88% versus 70%, P = 0.06), and more often smaller tumors (19 mm versus 25 mm, P = 0.04) compared with those who did not undergo FP (Table 1).
In 33 of the 34 (97%) patients who pursued FP, embryos or oocytes could be cryopreserved. In one patient only one oocyte was obtained, which could not be fertilized. In 25 patients embryos were frozen and in seven oocytes. One patient chose to preserve both embryos and oocytes. Per patient a median of four embryos (range 1–17) and seven oocytes (range 2–13) were cryopreserved. In three patients, two cycles of oocyte retrieval were necessary, the other patients underwent one cycle.
Ovarian function
In all but four patients menses was stopped during chemotherapy. Median time to OFR was 9 months (range 0–83 months). The 2-year OFR-rate was 68% (95% CI 59–77%). The 5-year OFR rate was 92% for the total group of counseled patients (Fig. 2).
Live birth
Live birth occurred in 26 women. All pregnancies occurred at least 2 years after the diagnosis of breast cancer. The 5-year live birth rate was 27% (95% CI 17–38%, Fig. 3). Of the 26 women giving live birth, eleven had estrogen receptor-positive disease.
Ten women in the FP group gave birth to twelve babies. Eleven babies were healthy, one had a congenital anomaly (M. Hirschsprung).
Only three women applied for transfer of cryopreserved embryos. Two of these women asked for PGD of the frozen embryos because they had a germline mutation in the BRCA1 gene, although both had OFR. Both women became pregnant after transfer of an embryo without the BRCA1 mutation. One other woman did not conceive after thawing of 10 and transfer of 8 embryos. Also, her attempts to achieve a spontaneous pregnancy were not successful. Another patient was supported by intrauterine insemination (IUI) to become pregnant. The other nine pregnancies in this group were spontaneous pregnancies.
Sixteen women in the non-FP group gave birth to twenty healthy babies. All but one pregnancy in this group were spontaneous. One woman conceived via IVF after breast cancer treatment. One woman did not become pregnant despite OFR and the use of IVF and IUI.
Disease-free survival
Disease events were detected in fifteen patients. The 5-year disease-free survival rate was 85%. In the FP group, two patients developed distant metastases, of whom one is deceased, one patient had a loco-regional recurrence. In the non-FP group (n = 84), twelve women developed distant metastases, of whom four were deceased. For women in the FP group, the 5-year disease-free survival rate was 85% and for women in the non-FP group, the rate was 84% (logrank P = 0.42, Fig. 4).
Discussion
Twenty-nine percent of 118 young women with early breast cancer diagnosis elected FP after counseling. Predictive factors for choosing FP were childlessness at the time of diagnosis, having a male partner and smaller tumors. After a median follow-up of 52 months, only three of 34 couples used their frozen embryos in an attempt to achieve live birth. Interestingly, all three had OFR, and two of these used the embryos for PGD because of a BRCA1-mutation carriership. Also, in the total group, the 5-year OFR was more than 90%. Twenty-six mothers gave birth to thirty-two babies. The 5-year live birth rate was 27%.
Before initiating systemic treatment for breast cancer at a young age, the option of FP by cryopreservation of embryos of oocytes should be considered [13]. In our study, 29% of referred women underwent FP. Of note, we only counseled women who were potentially interested in FP. Other studies reported FP rates varying from 9 to 58%, with the lower rates seen in studies in unselected young women [9, 12, 22,23,24,25,26]. Based on the Dutch Cancer Registry database, we estimate that approximately 20% of women < 41 years and 35% of women < 35 years diagnosed with breast cancer wished referral for counseling. Remarkably, many patients in our study stated at the start of counseling that they tended not to opt for FP, even though they were not yet fully informed. However, counseling on the possible benefits and harms of chemotherapy including impact on fertility and the option of FP are important for the patient to make a well-informed decision before the initiation of chemotherapy in order to prevent regrets afterwards [17].
To date, the available data on the transfer of cryopreserved oocytes or embryos after breast cancer therapy are limited [18, 25, 27,28,29]. Embryo or oocyte transfer rates of 6—25% are reported [18, 25, 27,28,29]. In our study, only three women returned for embryo transfer, with a relatively high rate of spontaneous pregnancies. In the earlier reported studies, there is no information on OFR rates. Our current and former studies have shown high OFR rates in women < 40 years [30]. A quarter of patients had OFR between 2 and 5 years after counseling. When live birth is strived for too soon, the ovarian function may yet not have had time to recover.
Though FP in breast cancer patients is feasible and safe, the individual risk estimation of premature ovarian insufficiency should be part of the counseling procedure. Previously, we reported that with the currently used chemotherapy schedules, age is still the most important factor predicting OFR after chemotherapy [30, 31]. Petrek et al. showed that in women younger than 35 years of age, the long-term (more than 3 years after diagnosis) incidence of amenorrhea was similar to that of women who had not received chemotherapy (nearly 10%) [32]. In our current study, in patients < 30 years, at least 93% had OFR. Given these data, very young women may decide not to undergo a FP procedure. However, after completion of prolonged adjuvant endocrine therapy, irrespective of prior use of chemotherapy, natural aging may have caused loss of ovarian reserve and thus infertility, despite the presence of OFR. Although interruption of adjuvant endocrine therapy is used in daily practice, its safety is still under investigation in the POSITIVE trial (ClinicalTrials.gov Identifier: NCT02308085) [33]. For patients with BRCA 1/2-gene mutations, another argument for embryo or oocyte cryopreservation can be the option of PGD and the possibly shorter reproductive life span in these patients [34,35,36,37].
Luteinizing hormone releasing hormone analogs (LHRHa) are being used in premenopausal women to protect the ovarian function during chemotherapy [38,39,40]. Of note, the primary aim of the studies was to reduce the occurrence of premature menopause instead of improving live birth rates. As a result, the included population may not be appropriate to address the live birth rate. The added value of LHRHa in terms of live birth rate in younger women could thus be less than assumed from these studies. The POEMS trial is the only randomized controlled trial that reported pregnancies as preplanned endpoint and also reported live births. The live birth rate was 7% [38, 39]. A meta-analysis showed a 6% pregnancy rate in women undergoing chemotherapy alone [40]. The live birth rates were not reported. These rates are significantly lower as compared to the 5-year live birth rate in our study (27%), whereas none of the patients in our cohort received prophylactic LHRHa use. A possible explanation is the lower median age of the women in our study (31 years) as compared with the median age in the meta-analysis (39 years) [32, 41].
FP after diagnosis of breast cancer is considered a safe option [24, 42]. Even in women with estrogen receptor-positive breast tumors, small retrospective studies have shown no detrimental effect of FP with the estrogen-positive tumor in situ [28, 42,43,44,45]. Stimulation protocols that add letrozole or tamoxifen have been successfully implemented and keep serum estradiol close to physiologic levels during the cycle [43, 46, 47]. Live birth after breast cancer, even in endocrine sensitive tumors, is currently considered safe [48,49,50,51]. In our study, fifteen women had recurrent disease, five of them within 2 years after diagnosis. None of these patients had given live birth after the diagnosis of breast cancer.
Apart from the relative short follow-up time, a limitation of our study is that we do not have data for actual and persistent desire to have children during follow-up. Women may have tried to conceive as soon as the ovarian function recovered, or they might regret the choice of not having cryopreserved embryos of oocytes. Since pregnancy attempts were not prospectively registered, it could be that during follow-up, their responsible oncologist paid no active attention to it. Moreover, we did not collect information on the maintenance of their relationship. Hence, we are not sure whether the previous choice to cryopreserve embryos instead of oocytes may have been a barrier for some to achieve a pregnancy. However, the observation that a substantial number of patients gave live birth to one or more children is reassuring.
In conclusion, in our cross-sectional study, nearly one-third of the counseled women chose to undergo a procedure for FP. About a quarter of women gave birth within 5 years after counseling, in nearly all spontaneously. Only three women used their frozen embryos to achieve a live birth: two applied for PGD of their cryopreserved embryos because of a BRCA1 mutation, resulting in the birth of two healthy children. The third woman did not become pregnant after transfer of embryos. More research in this field is required, as fulfillment of the desire to have children is clearly related to the quality of life.
References
Fidler MM, Gupta S, Soerjomataram I, Ferlay J, Steliarova-Foucher E, Bray F (2017) Cancer incidence and mortality among young adults aged 20–39 years worldwide in 2012: a population-based study. Lancet Oncol 18(12):1579–1589. https://doi.org/10.1016/s1470-2045(17)30677-0
Partridge AH, Hughes ME, Warner ET, Ottesen RA, Wong YN, Edge SB, Theriault RL, Blayney DW, Niland JC, Winer EP, Weeks JC, Tamimi RM (2016) Subtype-dependent relationship between young age at diagnosis and breast cancer survival. J Clin Oncol 34(27):3308–3314. https://doi.org/10.1200/jco.2015.65.8013
Zhao J, Liu J, Chen K, Li S, Wang Y, Yang Y, Deng H, Jia W, Rao N, Liu Q, Su F (2014) What lies behind chemotherapy-induced amenorrhea for breast cancer patients: a meta-analysis. Breast Cancer Res Treat 145(1):113–128. https://doi.org/10.1007/s10549-014-2914-x
Zavos A, Valachis A (2016) Risk of chemotherapy-induced amenorrhea in patients with breast cancer: a systematic review and meta-analysis. Acta Oncol 55(6):664–670. https://doi.org/10.3109/0284186x.2016.1155738
Ter Welle-Butalid MEE, Vriens I, Derhaag JGJ, Leter EME, de Die-Smulders CEC, Smidt MM, van Golde R, Tjan-Heijnen V (2019) Counseling young women with early breast cancer on fertility preservation. J Assist Reprod Genet 36(12):2593–2604. https://doi.org/10.1007/s10815-019-01615-6
Mathews TJ, Hamilton BE (2016) Mean age of mothers is on the rise: United States, 2000–2014. NCHS data brief 232:1–8
Peccatori FA, Azim HA Jr, Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V, Pentheroudakis G (2013) Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24(Suppl 6):vi160–vi170. https://doi.org/10.1093/annonc/mdt199
Howard-Anderson J, Ganz PA, Bower JE, Stanton AL (2012) Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst 104(5):386–405. https://doi.org/10.1093/jnci/djr541
Ruddy KJ, Gelber SI, Tamimi RM, Ginsburg ES, Schapira L, Come SE, Borges VF, Meyer ME, Partridge AH (2014) Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J Clin Oncol 32(11):1151–1156. https://doi.org/10.1200/jco.2013.52.8877
Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, Rosenberg R, Przypyszny M, Rein A, Winer EP (2004) Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol 22(20):4174–4183. https://doi.org/10.1200/JCO.2004.01.159
Llarena NC, Estevez SL, Tucker SL, Jeruss JS (2015) Impact of fertility concerns on tamoxifen initiation and persistence. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djv202
Ruggeri M, Pagan E, Bagnardi V, Bianco N, Gallerani E, Buser K, Giordano M, Gianni L, Rabaglio M, Freschi A, Cretella E, Clerico M, Farolfi A, Simoncini E, Ciccarese M, Rauch D, Ramello M, Glaus A, Berardi R, Pellanda AF, Ribi K, Gelber S, Partridge AH, Goldhirsch A, Pagani O (2019) Fertility concerns, preservation strategies and quality of life in young women with breast cancer: Baseline results from an ongoing prospective cohort study in selected European Centers. Breast 47:85–92. https://doi.org/10.1016/j.breast.2019.07.001
Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, Wallace WH, Wang ET, Loren AW (2018) Fertility preservation in patients with cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. https://doi.org/10.1200/jco.2018.78.1914
Paluch-Shimon S, Pagani O, Partridge AH, Abulkhair O, Cardoso MJ, Dent RA, Gelmon K, Gentilini O, Harbeck N, Margulies A, Meirow D, Pruneri G, Senkus E, Spanic T, Sutliff M, Travado L, Peccatori F, Cardoso F (2017) ESO-ESMO 3rd international consensus guidelines for breast cancer in young women (BCY3). Breast 35:203–217. https://doi.org/10.1016/j.breast.2017.07.017
Covelli A, Facey M, Kennedy E, Brezden-Masley C, Gupta AA, Greenblatt E, Baxter NN (2019) Clinicians' perspectives on barriers to discussing infertility and fertility preservation with young women with cancer. JAMA Netw Open 2(11):e1914511. https://doi.org/10.1001/jamanetworkopen.2019.14511
Kelvin JF, Thom B, Benedict C, Carter J, Corcoran S, Dickler MN, Goodman KA, Margolies A, Matasar MJ, Noy A, Goldfarb SB (2016) Cancer and fertility program improves patient satisfaction with information received. J Clin Oncol 34(15):1780–1786. https://doi.org/10.1200/JCO.2015.64.5168
Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, Melisko ME, Cedars MI, Rosen MP (2012) Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer 118(6):1710–1717. https://doi.org/10.1002/cncr.26459
Oktay K, Turan V, Bedoschi G, Pacheco FS, Moy F (2015) Fertility preservation success subsequent to concurrent aromatase inhibitor treatment and ovarian stimulation in women with breast cancer. J Clin Oncol 33(22):2424–2429. https://doi.org/10.1200/JCO.2014.59.3723
von Wolff M, Thaler CJ, Frambach T, Zeeb C, Lawrenz B, Popovici RM, Strowitzki T (2009) Ovarian stimulation to cryopreserve fertilized oocytes in cancer patients can be started in the luteal phase. Fertil Steril 92(4):1360–1365. https://doi.org/10.1016/j.fertnstert.2008.08.011
Webber L, Davies M, Anderson R, Bartlett J, Braat D, Cartwright B, Cifkova R, de Muinck K-S, Hogervorst E, Janse F, Liao L, Vlaisavljevic V, Zillikens C, Vermeulen N (2016) ESHRE Guideline: management of women with premature ovarian insufficiency. Hum Reprod 31(5):926–937. https://doi.org/10.1093/humrep/dew027
Hudis CA, Barlow WE, Costantino JP, Gray RJ, Pritchard KI, Chapman JA, Sparano JA, Hunsberger S, Enos RA, Gelber RD, Zujewski JA (2007) Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol 25(15):2127–2132. https://doi.org/10.1200/JCO.2006.10.3523
Kim J, Oktay K, Gracia C, Lee S, Morse C, Mersereau JE (2012) Which patients pursue fertility preservation treatments? A multicenter analysis of the predictors of fertility preservation in women with breast cancer. Fertil Steril 97(3):671–676. https://doi.org/10.1016/j.fertnstert.2011.12.008
Hill KA, Nadler T, Mandel R, Burlein-Hall S, Librach C, Glass K, Warner E (2012) Experience of young women diagnosed with breast cancer who undergo fertility preservation consultation. Clin Breast Cancer 12(2):127–132. https://doi.org/10.1016/j.clbc.2012.01.002
Moravek MB, Confino R, Smith KN, Kazer RR, Klock SC, Lawson AK, Gradishar WJ, Pavone ME (2018) Long-term outcomes in cancer patients who did or did not pursue fertility preservation. Fertil Steril 109(2):349–355. https://doi.org/10.1016/j.fertnstert.2017.10.029
Takahashi Y, Shien T, Sakamoto A, Tsuyumu Y, Yoshioka R, Uno M, Hatono M, Kochi M, Kawada K, Tsukioki T, Iwamoto T, Ikeda H, Taira N, Matsuoka J, Nakatsuka M, Doihara H (2018) Current multidisciplinary approach to fertility preservation for breast cancer patients. Acta Med Okayama 72(2):137–142. https://doi.org/10.18926/amo/55854
Lambertini M, Fontana V, Massarotti C, Poggio F, Dellepiane C, Iacono G, Abate A, Miglietta L, Ferreccio C, Pescio MC, Conte B, Blondeaux E, Bighin C, D'Alonzo A, Vaglica M, Zanardi E, Boccardo F, Ballestrero A, Anserini P, Del Mastro L (2018) Prospective study to optimize care and improve knowledge on ovarian function and/or fertility preservation in young breast cancer patients: Results of the pilot phase of the PREgnancy and FERtility (PREFER) study. Breast 41:51–56. https://doi.org/10.1016/j.breast.2018.06.012
Hashimoto T, Nakamura Y, Obata R, Doshida M, Toya M, Takeuchi T, Kyono K (2017) Effects of fertility preservation in patients with breast cancer: a retrospective two-centers study. Reprod Med Biol 16(4):374–379. https://doi.org/10.1002/rmb2.12054
Chien AJ, Chambers J, McAuley F, Kaplan T, Letourneau J, Hwang J, Kim MO, Melisko ME, Rugo HS, Esserman LJ, Rosen MP (2017) Fertility preservation with ovarian stimulation and time to treatment in women with stage II-III breast cancer receiving neoadjuvant therapy. Breast Cancer Res Treat 165(1):151–159. https://doi.org/10.1007/s10549-017-4288-3
Diaz-Garcia C, Domingo J, Garcia-Velasco JA, Herraiz S, Mirabet V, Iniesta I, Cobo A, Remohi J, Pellicer A (2018) Oocyte vitrification versus ovarian cortex transplantation in fertility preservation for adult women undergoing gonadotoxic treatments: a prospective cohort study. Fertil Steril 109(3):478–485.e472. https://doi.org/10.1016/j.fertnstert.2017.11.018
Vriens IJ, De Bie AJ, Aarts MJ, de Boer M, van Hellemond IE, Roijen JH, van Golde RJ, Voogd AC, Tjan-Heijnen VC (2017) The correlation of age with chemotherapy-induced ovarian function failure in breast cancer patients. Oncotarget 8(7):11372–11379. https://doi.org/10.18632/oncotarget.14532
van Hellemond IEG, Vriens IJH, Peer PGM, Swinkels ACP, Smorenburg CH, Seynaeve CM, van der Sangen MJC, Kroep JR, de Graaf H, Honkoop AH, Erdkamp FLG, van den Berkmortel F, Kitzen J, de Boer M, de Roos WK, Linn SC, Imholz ALT, Tjan-Heijnen VCG (2017) Ovarian Function Recovery During Anastrozole in Breast Cancer Patients With Chemotherapy-Induced Ovarian Function Failure. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djx074
Petrek JA, Naughton MJ, Case LD, Paskett ED, Naftalis EZ, Singletary SE, Sukumvanich P (2006) Incidence, time course, and determinants of menstrual bleeding after breast cancer treatment: a prospective study. J Clin Oncol 24(7):1045–1051. https://doi.org/10.1200/JCO.2005.03.3969
Pagani O, Ruggeri M, Manunta S, Saunders C, Peccatori F, Cardoso F, Kaufman B, Paluch-Shimon S, Gewefel H, Gallerani E, Abulkhair OM, Pistilli B, Warner E, Saloustros E, Perey L, Zaman K, Rabaglio M, Gelber S, Gelber RD, Goldhirsch A, Korde L, Azim HA Jr, Partridge AH (2015) Pregnancy after breast cancer: are young patients willing to participate in clinical studies? Breast 24(3):201–207. https://doi.org/10.1016/j.breast.2015.01.005
Oktay K, Kim JY, Barad D, Babayev SN (2010) Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J Clin Oncol 28(2):240–244. https://doi.org/10.1200/jco.2009.24.2057
Derks-Smeets IAP, van Tilborg TC, van Montfoort A, Smits L, Torrance HL, Meijer-Hoogeveen M, Broekmans F, Dreesen J, Paulussen ADC, Tjan-Heijnen VCG, Homminga I, van den Berg MMJ, Ausems M, de Rycke M, de Die-Smulders CEM, Verpoest W, van Golde R (2017) BRCA1 mutation carriers have a lower number of mature oocytes after ovarian stimulation for IVF/PGD. J Assist Reprod Genet 34(11):1475–1482. https://doi.org/10.1007/s10815-017-1014-3
Turan V, Bedoschi G, Emirdar V, Moy F, Oktay K (2018) Ovarian stimulation in patients with cancer: impact of letrozole and BRCA mutations on fertility preservation cycle outcomes. Reprod Sci 25(1):26–32. https://doi.org/10.1177/1933719117728800
Lambertini M, Goldrat O, Ferreira AR, Dechene J, Azim HA Jr, Desir J, Delbaere A, t’Kint de Roodenbeke MD, de Azambuja E, Ignatiadis M, Demeestere I (2018) Reproductive potential and performance of fertility preservation strategies in BRCA-mutated breast cancer patients. Ann Oncol 29(1):237–243. https://doi.org/10.1093/annonc/mdx639
Moore HC, Unger JM, Phillips KA, Boyle F, Hitre E, Porter D, Francis PA, Goldstein LJ, Gomez HL, Vallejos CS, Partridge AH, Dakhil SR, Garcia AA, Gralow J, Lombard JM, Forbes JF, Martino S, Barlow WE, Fabian CJ, Minasian L, Meyskens FL Jr, Gelber RD, Hortobagyi GN, Albain KS, Investigators PS (2015) Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med 372(10):923–932. https://doi.org/10.1056/NEJMoa1413204
Moore HCF, Unger JM, Phillips KA, Boyle F, Hitre E, Moseley A, Porter DJ, Francis PA, Goldstein LJ, Gomez HL, Vallejos CS, Partridge AH, Dakhil SR, Garcia AA, Gralow JR, Lombard JM, Forbes JF, Martino S, Barlow WE, Fabian CJ, Minasian LM, Meyskens FL, Gelber RD, Hortobagyi GN, Albain KS (2019) Final analysis of the prevention of early menopause study (POEMS)/SWOG Intergroup S0230. J Natl Cancer Inst 111(2):210–213. https://doi.org/10.1093/jnci/djy185
Lambertini M, Moore HCF, Leonard RCF, Loibl S, Munster P, Bruzzone M, Boni L, Unger JM, Anderson RA, Mehta K, Minton S, Poggio F, Albain KS, Adamson DJA, Gerber B, Cripps A, Bertelli G, Seiler S, Ceppi M, Partridge AH, Del Mastro L (2018) Gonadotropin-releasing hormone agonists during chemotherapy for preservation of ovarian function and fertility in premenopausal patients with early breast cancer: a systematic review and meta-analysis of individual patient-level data. J Clin Oncol. https://doi.org/10.1200/jco.2018.78.0858
Walshe JM, Denduluri N, Swain SM (2006) Amenorrhea in premenopausal women after adjuvant chemotherapy for breast cancer. J Clin Oncol 24(36):5769–5779. https://doi.org/10.1200/jco.2006.07.2793
Rodriguez-Wallberg KA, Eloranta S, Krawiec K, Lissmats A, Bergh J, Liljegren A (2018) Safety of fertility preservation in breast cancer patients in a register-based matched cohort study. Breast Cancer Res Treat 167(3):761–769. https://doi.org/10.1007/s10549-017-4555-3
Letourneau JM, Wald K, Sinha N, Juarez-Hernandez F, Harris E, Cedars MI, McCulloch CE, Dolezal M, Chien AJ, Rosen MP (2019) Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 43 months after fertility-preservation consultation. Cancer. https://doi.org/10.1002/cncr.32546
Letourneau JM, Sinha N, Wald K, Harris E, Quinn M, Imbar T, Mok-Lin E, Chien AJ, Rosen M (2017) Random start ovarian stimulation for fertility preservation appears unlikely to delay initiation of neoadjuvant chemotherapy for breast cancer. Hum Reprod 32(10):2123–2129. https://doi.org/10.1093/humrep/dex276
Kim J, Turan V, Oktay K (2016) Long-term safety of letrozole and gonadotropin stimulation for fertility preservation in women with breast cancer. J Clin Endocrinol Metab 101(4):1364–1371. https://doi.org/10.1210/jc.2015-3878
Azim AA, Costantini-Ferrando M, Oktay K (2008) Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol 26(16):2630–2635. https://doi.org/10.1200/jco.2007.14.8700
Meirow D, Raanani H, Maman E, Paluch-Shimon S, Shapira M, Cohen Y, Kuchuk I, Hourvitz A, Levron J, Mozer-Mendel M, Brengauz M, Biderman H, Manela D, Catane R, Dor J, Orvieto R, Kaufman B (2014) Tamoxifen co-administration during controlled ovarian hyperstimulation for in vitro fertilization in breast cancer patients increases the safety of fertility-preservation treatment strategies. Fertil Steril 102(2):488–495.e483. https://doi.org/10.1016/j.fertnstert.2014.05.017
Hartman EK, Eslick GD (2016) The prognosis of women diagnosed with breast cancer before, during and after pregnancy: a meta-analysis. Breast Cancer Res Treat 160(2):347–360. https://doi.org/10.1007/s10549-016-3989-3
Iqbal J, Amir E, Rochon PA, Giannakeas V, Sun P, Narod SA (2017) Association of the timing of pregnancy with survival in women with breast cancer. JAMA Oncol 3(5):659–665. https://doi.org/10.1001/jamaoncol.2017.0248
Lambertini M, Kroman N, Ameye L, Cordoba O, Pinto A, Benedetti G, Jensen MB, Gelber S, Del Grande M, Ignatiadis M, de Azambuja E, Paesmans M, Peccatori FA, Azim HA Jr (2018) Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst 110(4):426–429. https://doi.org/10.1093/jnci/djx206
Lambertini M, Martel S, Campbell C, Guillaume S, Hilbers FS, Schuehly U, Korde L, Azim HA Jr, Di Cosimo S, Tenglin RC, Huober J, Baselga J, Moreno-Aspitia A, Piccart-Gebhart M, Gelber RD, de Azambuja E, Ignatiadis M (2019) Pregnancies during and after trastuzumab and/or lapatinib in patients with human epidermal growth factor receptor 2-positive early breast cancer: analysis from the NeoALTTO (BIG 1–06) and ALTTO (BIG 2–06) trials. Cancer 125(2):307–316. https://doi.org/10.1002/cncr.31784
Acknowledgements
We thank R. Tjan and R. Vleugels for their assistance in data management and J. Roijen for her participation in patient care.
Funding
This work was supported by a grant from Pink Ribbon Netherlands (Grant Number 2008.C42, recipient V.C.G. Tjan-Heijnen); and the Department of Medical Oncology, Maastricht University Medical Centre, Maastricht, the Netherlands.
Author information
Authors and Affiliations
Contributions
The funders had no role in the design of the study; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of interest
Vivianne C.G. Tjan-Heijnen received research grants from AstraZeneca, Novartis, Pfizer, Roche, Eisai, and E. Lily. Honorarium or other (financial) fees: Roche, Novartis, and E. Lily. The remaining authors have no disclosures.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
According to the Netherlands Central Committee on Research Involving Human Subjects guidelines, this observational study is not subject to the Act on Medical Research Involving Human Subjects and therefore informed consent is not obtained for patients included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vriens, I.J.H., ter Welle-Butalid, E.M., de Boer, M. et al. Preserving fertility in young women undergoing chemotherapy for early breast cancer; the Maastricht experience. Breast Cancer Res Treat 181, 77–86 (2020). https://doi.org/10.1007/s10549-020-05598-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05598-2