Abstract
Purpose
Alongside the modern trend of delaying childbirth, the high incidence of breast cancer among young women is causing significant pregnancy-related problems in Korea. We estimated the incidence of childbirth for young Korean breast cancer survivors compared with women who did not have breast cancer using a nationally representative dataset.
Methods
Using a database from the National Health Insurance Service in South Korea, we analyzed 109,680 women who were between 20 and 40 years old between 2007 and 2013. They were prospectively followed, and childbirth events were recorded until December 31, 2015. We compared childbirth rates and characteristics between the breast cancer survivors and the noncancer controls.
Results
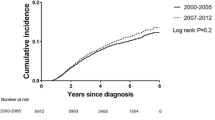
Compared to 10,164 childbirths among 91,400 women without breast cancer (incidence rate: 22.3/1000), 855 childbirths occurred among 18,280 breast cancer survivors (incidence rate: 9.4/1000); the adjusted hazard ratio (HR) for childbirth was 0.41 (95% CI 0.38–0.44). Chemotherapy, endocrine therapy, and target therapy were associated with the decreasing childbirths among survivors, with corresponding adjusted HRs of 0.61 (0.53–0.70), 0.44 (0.38–0.51), and 0.62 (0.45–0.86), respectively. Breast cancer survivors had a lower probability of full-term delivery and a higher frequency of preterm labor than controls, with corresponding adjusted ORs of 0.78 (0.68–0.90) and 1.33 (1.06–1.65), respectively.
Conclusions
We showed that a history of breast cancer has a negative effect on childbirth among young premenopausal women in Korea. Breast cancer survivors should be aware that they have a higher risk for preterm labor and are less likely to have a full-term delivery than women without a history of breast cancer.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the NHIS but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the NHIS.
References
Oh CM, Won YJ, Jung KW et al (2016) The Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat 48(2):436–450
GLOBOCAN 2012. Estimated cancer incidence, mortality and prevalence worldwide in 2012. International Agency for Research on Cancer, Lyon. http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed 1 Sept 2016
Jemal A, Siegel R, Ward E et al (2007) Cancer statistics, 2007. CA Cancer J Clin 57:43–66
Kim Z, Min SY, Yoon CS et al (2015) The basic facts of Korean breast cancer in 2012: results from a nationwide survey and breast cancer registry database. J Breast Cancer 18(2):103–111
Del Mastro L, Venturini M, Sertoli MR, Rosso R (1997) Amenorrhea induced by adjuvant chemotherapy in early breast cancer patients: prognostic role and clinical implications. Breast Cancer Res Treat 43:183–190
Partridge A, Gelber S, Gelber RD et al (2007) Age of menopause among women who remain premenopausal following treatment for early breast cancer: long-term results from International Breast Cancer Study Group Trials V and VI. Eur J Cancer 43:1646–1653
Shandley LM, Spencer JB, Fothergill A et al (2017) Impact of tamoxifen therapy on fertility in breast cancer survivors. Fertil Steril 107:243–252
Partridge AH, Gelber S, Peppercorn J et al (2004) Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol 22:4174–4183
Pagani O, Partridge A, Korde L et al (2011) Pregnancy after breast cancer: if you wish, ma’am. Breast Cancer Res Treat 129:309–317
OECD Family Database. SF2.3: age of mothers at childbirth and age-specific fertility. http://www.oecd.org/els/family/database.htm
Seong SC, Kim YY, Khang YH et al (2017) Data resource profile: the national health information database of the national health insurance service in South Korea. Int J Epidemiol 46:799–800
Song SO, Jung CH, Song YD et al (2014) Background and data configuration process of a nationwide population-based study using the Korean National Health Insurance System. Diabetes Metab J 38:395–403
Malamos NA, Stathopoulos GP, Keramopoulos A, Papadiamantis J, Vassilaros S (1996) Pregnancy and offspring after the appearance of breast cancer. Oncology 53:471–475
Emens LA, Davidson NE (2003) Adjuvant hormonal therapy for premenopausal women with breast cancer. Clin Cancer Res 9:486s–494s
Dalberg K, Eriksson J, Holmberg L (2006) Birth outcome in women with previously treated breast cancer-a population-based cohort study from Sweden. PLoS Med. 3(9):e336
Black KZ, Nichols HB, Eng E, Rowley DL (2017) Prevalence of preterm, low birthweight, and small for gestational age delivery after breast cancer diagnosis: a population-based study. Breast Cancer Res 19(1):11
Langagergaard V, Gislum M, Skriver MV et al (2006) Birth outcome in women with breast cancer. Br J Cancer 94(1):142–146
Ives A, Saunders C, Bulsara M, Semmens J (2007) Pregnancy after breast cancer: population based study. BMJ 334(7586):194
Nichols HB, Schoemaker MJ, Cai J et al (2019) Breast cancer risk after recent childbirth: a pooled analysis of 15 prospective studies. Ann Intern Med 170:22–30
Averette HE, Mirhashemi R, Moffat FL (1999) Pregnancy after breast carcinoma: the ultimate medical challenge. Cancer 85(11):2301–2304
Upponi SS, Ahmad F, Whitaker IS, Purushotham AD (2003) Pregnancy after breast cancer. Eur J Cancer 39(6):736–741
Kim JS, Kang EJ, Woo OH et al (2013) The relationship between preeclampsia, pregnancy-induced hypertension and maternal risk of breast cancer: a meta-analysis. Acta Oncol 52(8):1643–1648
Sun M, Fan Y, Hou Y et al (2018) Preeclampsia and maternal risk of breast cancer: a meta-analysis of cohort studies. J Matern Fetal Neonatal Med 31:2484–2491
Acknowledgements
This work was supported by the Korean Breast Cancer Society and the Study of Multi-disciplinARy Teamwork for breast cancer survivorSHIP (SMARTSHIP). This study enrolled patients from the National Health Information Database (NHIS-2017-4-011), which was provided and is maintained by the National Health Insurance Service (NHIS). The authors would like to thank the National Health Insurance Service for cooperation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The authors declare that the present study complies with the current laws of Korea, and this study was approved by the Institutional Review Board of Catholic Kwandong University International St. Mary’s Hospital (IS16RCMI0053).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, H.M., Kim, B.W., Park, S. et al. Childbirth in young Korean women with previously treated breast cancer: The SMARTSHIP study. Breast Cancer Res Treat 176, 419–427 (2019). https://doi.org/10.1007/s10549-019-05244-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05244-6