Abstract
Age-related lobular involution (LI) is a physiological process in which the terminal duct lobular units of the breast regress as a woman ages. Analyses of breast biopsies from women with benign breast disease (BBD) have found that extent of LI is negatively associated with subsequent breast cancer development. Here we assess the natural course of LI within individual women, and the impact of progressive LI on breast cancer risk. The Mayo Clinic BBD cohort consists of 13,455 women with BBD from 1967 to 2001. The BBD cohort includes 1115 women who had multiple benign biopsies, 106 of whom had developed breast cancer. Within this multiple biopsy cohort, the progression of the LI process was examined by age at initial biopsy and time between biopsies. The relationship between LI progression and breast cancer risk was assessed using standardized incidence ratios and by Cox proportional hazards analysis. Women who had multiple biopsies were younger age and had a slightly higher family history of breast cancer as compared with the overall BBD cohort. Extent of LI at subsequent biopsy was greater with increasing time between biopsies and for women age 55 + at initial biopsy. Among women with multiple biopsies, there was a significant association of higher breast cancer risk among those with involution stasis (lack of progression, HR 1.63) as compared with those with involution progression, p = 0.036. The multiple biopsy BBD cohort allows for a longitudinal study of the natural progression of LI. The majority of women in the multiple biopsy cohort showed progression of LI status between benign biopsies, and extent of progression was highest for women who were in the perimenopausal age range at initial biopsy. Progression of LI status between initial and subsequent biopsy was associated with decreased breast cancer risk.
Similar content being viewed by others
Introduction
Age-related lobular involution (LI) is a physiological process in which the epithelial tissue of the breast gradually regresses, corresponding with elimination of the need for milk production beyond the child-bearing years. Analysis of the Mayo Clinic cohort of more than 13,000 women who had a breast biopsy with benign findings and were thus diagnosed with benign breast disease (BBD) showed that the timing of LI centers around the perimenopausal years but varies considerably among women [1–3], with complete LI in 8.5 % of women <40 years of age [1, 3], while more than half of women over 50 with BBD have not completed the process of LI [1, 4, 5]. Investigation of LI in a sample of breast tissues from normal donors demonstrated reductions in acini counts per terminal duct lobular unit (TDLU) starting in the 3rd decade of life and slowing of this process in the 6th decade [6].
The Mayo BBD Cohort includes 13,455 women, ages 18–85 at biopsy, who had a breast biopsy with benign findings at Mayo Clinic 1967–2001, and of whom 1273 have subsequently developed breast cancer [7]. In the Mayo BBD Cohort, LI extent at initial biopsy was categorized qualitatively as none (0 % lobules involuted), partial (1–74 % involuted) or complete (≥75 % involuted), and progressive degrees of LI were found to be associated with a significantly reduced risk of breast cancer [1]. These results were subsequently confirmed in an analysis of patient samples from the Nurses’ Health Study, which found that smaller lobular size was associated with decreased cancer risk [8]. While an association between progressive LI and reduced breast cancer risk is consistent with the understanding that breast lobules are the anatomic substructure that gives rise to breast cancer [9], these findings were particularly robust in that progressive degrees of LI were associated with reduced cancer risk even in subsets of women at high-risk due to epithelial proliferation. Thus, even for women with atypical hyperplasia (atypia), a high-risk subset (overall relative risk [RR] = 4 for cancer development), patients with no LI in the background lobules had substantially higher risk of subsequent breast cancer than those who had completed involution (RR = 7.79 vs. 1.49, respectively), and for postmenopausal women in particular, evidence of no or partial LI was associated with a 3-fold increased breast cancer risk as compared to women in which the LI process had been completed.
Previous studies of LI status have involved evaluations of cohorts at single time points, and identification of the relationship between progressive stages of LI and breast cancer risk was limited by an inability to distinguish between women who had undergone LI at some point in the past and women who may never have developed extensive lobular structures. We have now identified from the Mayo BBD cohort a group of 1115 women who had multiple, sequential benign biopsies, with time between biopsies from 60 days to more than 15 years. Within this multiple biopsy cohort, we have assessed for the first time the relationship between age and LI progression over time within individual women, and have evaluated how active LI progression versus LI stasis is linked with subsequent breast cancer incidence.
Methods
Study population
The Mayo BBD Cohort has been described previously [10, 11] and currently comprises 13,455 women ages 18–85 who underwent benign breast biopsies between 1967 and 2001 at Mayo Clinic (Rochester, MN). Demographic clinical features and risk factors were identified from medical records and questionnaires [10, 11]. Evaluation of patient records identified 1115 women who had undergone at least one additional benign biopsy more than 60 days after the initial biopsy (multiple biopsy cohort).
Demographic and clinical characteristics were collected using study questionnaires and comprehensive medical record review. Family history of breast cancer was categorized as strong, weak, or negative. A strong family history was defined as the patient having (1) at least one first-degree relative with breast cancer diagnosed before age 50 years or (2) two relatives with breast cancer at any age, with at least one being a first-degree relative. Blood relatives from either the mother’s or father’s side were included. Members adopted into the family, or members from any potential spouse were not included. Patients with family history of breast cancer who did not meet the above criteria were categorized as having a weak family history.
Breast cancer events were ascertained from study questionnaires, tumor registry, and review of medical records. With a median of 21.9 years of follow-up for the multiple biopsy cohort, 106 women have been diagnosed with breast cancer. The study protocol, including patient contact and follow-up methods, was approved by the Mayo Clinic Institutional Review Board with methods previously described [1].
Histologic examination
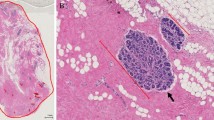
The study breast pathologist (DWV) performed histologic review of archived H&E slides from the subsequent benign biopsies, and histologic features were recorded. Biopsy findings were classified by the most extreme degree of hyperplasia as nonproliferative, proliferative disease without atypia, or atypical hyperplasia, as previously reported [7]. LI status was previously assessed in the initial biopsy for the entire cohort according to a three-level categorization: non-involuted, 0 %; partial involution, 1–75 %; complete involution, 75–100 % [1]. The LI status of the initial and subsequent biopsies for the patients in the multiple biopsy cohort were assessed using a four-level metric to provide increased resolution of LI status: 0–25 % involuted, 26–50 %, 51–74 %, and 75–100 %.
Statistical methods
Data were summarized using means and standard deviations for continuous variables and percentages and frequencies for categorical variables. Occurrence of subsequent biopsy was compared across levels of categorical variables (age of BBD, breast cancer status, overall impression, involution, family history of breast cancer, number of children) using Pearson Chi-squared tests for significance. Kruskal–Wallis tests were used for continuous covariates (duration of follow-up). Age-adjusted comparisons were also performed using logistic regression.
To determine if women with multiple benign biopsies were representative of the overall BBD cohort, associations were examined between previously published risk factors and later breast cancer [12]. Results from subsetting to women with multiple benign biopsies were compared to results from the overall BBD cohort. The duration of follow-up was calculated as the number of days from first biopsy of the benign lesion to the date of the diagnosis of breast cancer, death, prophylactic mastectomy, reduction mammoplasty, LCIS, or last contact. Internal comparisons were performed using hazard ratio (HR) estimates using a conventional Cox proportional hazards regression analysis. External comparisons were performed using relative risk (RR) estimates from standardized incidence ratios (SIRS). SIRS are an external comparison of the number of observed breast cancers versus the number expected using age-year specific incidence rates of breast cancer from the Iowa Surveillance, Epidemiology, and End Results (SEER) registry, and were calculated using methods in previous publications [13].
Associations between LI progression at second biopsy and features at index biopsy were assessed using logistic regression. Time between biopsies, age at index biopsy, and involution at index were included as predictors. Women with LI >75 % at index were not included in this comparison due to their inability to progress. Each variable was initially examined univariately in separate logistic regression models. After this, we fit one overall multivariate logistic model that included all variables to assess the independent effects on LI progression.
Comparisons of breast cancer risk at second biopsy were performed using multiple methods. Internal comparisons were made using Cox proportional hazards regression. Duration of follow-up was calculated in the same fashion as above with date of second biopsy as the starting time point. Time was modeled as a function of age using start and stop methods rather than time on study [14]. Like in the logistic analyses, women with LI >75 % at index were not included in either comparison due to their inability to progress. Covariates examined included LI at index biopsy, overall impression at index biopsy, and change in involution from index to second biopsy. Each variable was examined univariately in separate Cox models. An overall multivariate Cox model including all variables was used to assess independent effects on risk of breast cancer. External comparisons of breast cancer risk at second biopsy were performed using SIRS. LI at second biopsy, change in involution, and histologic impression at second biopsy were examined. All statistical tests were 2 sided and conducted using SAS statistical software (SAS institute Inc., Cary, NC). A p value <0.05 was determined significant.
Results
LI progression and breast cancer risk in multiple biopsy cohort
Of the 13,455 patients in the Mayo BBD cohort, 1115 were found to have had multiple, sequential benign biopsies (Supplemental Table 1). Comparison of baseline patient characteristics between the multiple biopsy BBD cohort and the rest of the BBD cohort revealed that the multiple biopsy cohort is significantly younger (p < 0.001) and was followed longer (median 20.7 years follow-up for multiple biopsy cohort as compared to 15.4 years for the rest of the BBD cohort, p < 0.001). Women in the multiple biopsy cohort were significantly more likely to show proliferative disease without atypia at the initial biopsy (PDWA; p = 0.014 univariate, p < 0.001 when adjusted for patient age at initial biopsy) and had a stronger family history of breast cancer (p < 0.001) than the remainder of the cohort. LI status was assessed for the initial and subsequent biopsies using a four-level metric to provide increased resolution of LI status: 0–25 % involuted, 26–50, 51–74, and 75–100 % (Fig. 1). Comparison of the LI status for the multiple biopsy group showed significantly lower levels of involution as compared to the rest of the BBD cohort, even when adjusted for patient age (p < 0.001). Of the women in the multiple biopsy cohort, 106 subsequently developed breast cancer (cases), while 1009 remained cancer-free (controls); this relative proportion of cases vs. controls showed no significant difference as compared to the rest of the BBD cohort (age-adjusted p = 0.876).
Breast cancer risk (observed versus expected) was assessed through standardized incidence ratios (SIRs) for the overall BBD cohort and the multiple biopsy BBD cohort (Supplemental Table 2). In the entire BBD cohort, categories of LI status at initial biopsy, overall histologic impression, and age at initial biopsy were all significantly associated with later breast cancer risk. By contrast, LI status and age initial biopsy and were not significantly associated with later breast cancer risk in the multiple biopsy cohort, possibly due in part to the younger age of the multiple biopsy cohort as well as the increased follow-up time for women in this cohort, since women in this group did not have breast cancer between biopsies, which shifts their risk profile.
Hazard ratios (HRs) for breast cancer risk in the overall cohort and in the multiple biopsy cohort were calculated via Cox regression, which allows for adjustment of other covariates including time from first biopsy to second biopsy and histologic impression (Supplemental Table 3). These results showed a strong and progressive reduction of risk by LI status for the overall BBD cohort, while no significant HR differences were seen for categorical LI in the multiple biopsy BBD cohort when assessed at initial biopsy, possibly due in part to the smaller sample size.
Rate of LI progression by patient age in the multiple biopsy cohort
Women were assigned to the category LI progression when the subsequent biopsy was assessed as having a greater extent of LI as compared to the initial biopsy (0–25 % at initial biopsy to 26–100, 25–50 % to 51–100, or 51–74 % at initial biopsy to 75–100 %; N = 507); women showing complete involution at initial biopsy (N = 281) were excluded from consideration for LI progression. Patients were assigned to the category LI stasis when the subsequent biopsy was assessed as having the same or decreased degree of LI status (75–100 to 0–100 %, 26–74 to 0–74 %, and 0–25 to 0–25 %; N = 327; Table 1).
The relative proportion of patients showing LI progression increased with longer time between biopsies, although this effect was most significant for women who had initial biopsies at ages <45 and 45–55, as women who had initial biopsy greater than age 55 were largely completely involuted at their initial biopsy (Supplemental Table 4). Calculation of adjusted odds ratios for LI progression (Table 2) revealed a significantly higher incidence of LI progression when time between biopsies was greater than 2 years, with generally increasing LI progression rates at longer time points (as compared with patients having time between biopsies <2 years, adjusted for age at BBD and LI status at initial biopsy). Evaluation by age at initial biopsy showed greatest incidence of LI progression from non-involuted or partially involuted states for patients >55 years (as compared with patients with initial biopsy at ages <45 years, adjusted for time between biopsy and LI status at initial biopsy), and reducing likelihood of LI progression with greater extent of LI at initial biopsy (adjusted for time between biopsy and age at initial biopsy). Use of hormone replacement therapy (HRT) was available for 85 % of the patients in the multiple biopsy cohort, but no information was available for whether HRT was used prior to first biopsy, between biopsies, or after the subsequent biopsy. HRT usage was not found to be significantly associated with involution progression (p = 0.482, Table 2).
Effect of LI progression or stasis on breast cancer risk
HRs were also calculated to examine the effect of LI progression vs. LI stasis (Table 1) on breast cancer risk following the subsequent biopsy (Table 3). For these analyses, follow-up was defined as time from second biopsy to breast cancer event or censorship. These results showed that LI stasis patients had a significant increase in breast cancer risk as compared with LI progression patients after accounting for LI at the index biopsy and all other variables listed in the table (HR 1.63 [95 % CI 1.03–2.57], p = 0.036). We also performed a similar analysis in which follow-up time was stratified on time since first biopsy (<10 years vs. 10 + years), and found similar results, with a slightly weaker (though still significant) association with involution progression (HR 1.64 [95 % CI 1.02–2.64), p = 0.041; Supplemental Table 5).
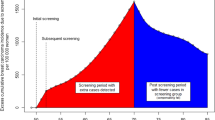
We also evaluated SIRs, which allow for comparison with an outside group, in the multiple biopsy group based on time from subsequent biopsy to later breast cancer (Table 4). These analyses revealed a higher overall SIR for the multiple biopsy BBD patients (1.93 [95 % CI 1.53–2.39], as compared to 1.65 [95 % CI 1.56–1.74] for the overall BBD cohort and 1.35 [95 % CI 1.11–1.64] for the multiple biopsy BBD cohort at initial biopsy, Supplemental Table 2). SIRs for LI status at subsequent biopsy were also larger for no LI (2.94 [95 % CI 1.61–4.93], as compared to 2.08 [95 % CI 1.83–2.36] for patients with no LI in the overall BBD cohort and 1.41 [95 % CI 0.93–2.06] for patients from the multiple biopsy BBD cohort with no LI at initial biopsy, Supplemental Table 2). Strikingly, SIRs at subsequent biopsy for patients with LI stasis were increased as compared with patients with LI progression (Table 4; LI progression, 1.59 [95 % CI 1.13–2.17] versus LI stasis, 2.44 [95 % CI 1.76–3.28], p = 0.054). Thus, at time of subsequent biopsy, when the association between LI status and breast cancer risk is much closer to that of the overall BBD cohort, ongoing LI is associated with a marginally significant decrease in breast cancer risk as compared to stalled LI.
Discussion
In this study, we define a cohort of 1115 women from within the larger Mayo BBD cohort who had multiple, sequential benign biopsies at the Mayo Clinic. We find that there are differences between the women in the multiple biopsy cohort as compared with the overall BBD cohort, in that they are significantly younger and more likely to have a family history of breast cancer, although the age-adjusted incidence of breast cancer in the multiple biopsy cohort was essentially the same. Evaluation of change of LI status between initial and subsequent biopsy provided the expected finding that progressive LI was more common with increasing time between biopsies (Supplemental Table 4) and in peri- and post-menopausal women (Table 2). Previous studies of LI and breast cancer risk have consistently found that increased LI status is associated with decreased breast cancer risk [8, 15–20], but these studies only examined women at single points in time. This is the first study to examine individual women at multiple time points. We also found that LI status was strongly associated with breast cancer risk when assessed at subsequent biopsy (Table 4), though this relationship was weaker when assessed at initial biopsy (Supplemental Table 2). This difference is likely a consequence of the increased follow-up time for women in the multiple biopsy cohort, since by definition, women in this group did not have breast cancer between biopsies, which necessarily shifted their risk profile.
Nearly three-quarters of breast cancer cases are diagnosed at age 50 or higher [21], and considerable research effort has been directed to understanding how the process of aging is linked to breast cancer development. Of note, the greatest increase in rate of breast cancer occurs during the peri- and early postmenopausal years [22], where we also find greatest evidence for ongoing progression of the LI process (Table 2). Our previous investigations with the BBD cohort have revealed that breast cancer risk is concentrated in the 40 % of postmenopausal women for whom the process of LI is delayed [1], and our findings presented here reveal that women in the multiple biopsy BBD group who do not have LI progression between initial and subsequent biopsies are at significantly increased risk as compared with women who do show LI progression (Table 4). Further investigations as to the information present at a histological or molecular level in the benign breast biopsies of the women in the multiple biopsy BBD cohort could reveal mediators driving the process of LI. By extension, these mediators could further provide insight into why LI is delayed in many postmenopausal women and why these women are at increased risk for development of breast cancer.
This is the first investigation of LI changes across time in individual women, and the first demonstration that stalled LI is a significant predictor of increased breast cancer risk. Strengths of the study include centralized pathological review for all BBD patients and for the initial and subsequent biopsies in the multiple biopsy cohort, as well as the large size of the multiple biopsy cohort and the ability to compare with the entire BBD cohort. Weaknesses include the significant differences in average age between the multiple biopsy cohort as compared with the overall BBD cohort, as well as the limited power of our statistical comparisons. In conclusion, this study revealed that progressive LI status has a protective mechanism for breast cancer development, and might be utilized as a risk marker in breast cancer risk assessment models. Further longitudinal studies involving BBD cohorts are encouraged to evaluate the progression of LI and breast cancer development.
References
Milanese TR, Hartmann LC, Sellers TA, Frost MH, Vierkant RA, Maloney SD, Pankratz VS, Degnim AC, Vachon CM, Reynolds CA, Thompson RA, Melton LJ 3rd, Goode EL, Visscher DW (2006) Age-related lobular involution and risk of breast cancer. J Natl Cancer Inst 98(22):1600–1607
Hutson SW, Cowen PN, Bird CC (1985) Morphometric studies of age related changes in normal human breast and their significance for evolution of mammary cancer. J Clin Pathol 38(3):281–287
Geschickter C (1945) Diseases of the breast. J.B. Lipincott Co, Philadelphia
Henson DE, Tarone RE (1993) On the possible role of involution in the natural history of breast cancer. Cancer 71(6 Suppl):2154–2156
Henson DE, Tarone RE (1994) Involution and the etiology of breast cancer. Cancer 74(1 Suppl):424–429
Figueroa JD, Pfeiffer RM, Patel DA, Linville L, Brinton LA, Gierach GL, Yang XR, Papathomas D, Visscher D, Mies C, Degnim AC, Anderson WF, Hewitt S, Khodr ZG, Clare SE, Storniolo AM, Sherman ME (2014) Terminal duct lobular unit involution of the normal breast: implications for breast cancer etiology. J Natl Cancer Inst 106(10):286. doi:10.1093/jnci/dju286
Hartmann LC, Sellers TA, Frost MH, Lingle WL, Degnim AC, Ghosh K, Vierkant RA, Maloney SD, Pankratz VS, Hillman DW, Suman VJ, Johnson J, Blake C, Tlsty T, Vachon CM, Melton LJ 3rd, Visscher DW (2005) Benign breast disease and the risk of breast cancer. N Engl J Med 353(3):229–237
Baer HJ, Collins LC, Connolly JL, Colditz GA, Schnitt SJ, Tamimi RM (2009) Lobule type and subsequent breast cancer risk: results from the Nurses’ Health Studies. Cancer 115(7):1404–1411. doi:10.1002/cncr.24167
Wellings SR, Jensen HM, Marcum RG (1975) An atlas of subgross pathology of the human breast with special reference to possible precancerous lesions. J Natl Cancer Inst 55(2):231–273
Hartmann LC, Sellers TA, Frost MH, Lingle WL, Degnim AC, Ghosh K, Vierkant RA, Maloney SD, Pankratz VS, Hillman DW, Suman VJ, Johnson J, Blake C, Tlsty T, Vachon CM, Melton LJ 3rd, Visscher DW (2005) Benign breast disease and the risk of breast cancer. N Engl J Med 353(3):229–237. doi:10.1056/NEJMoa044383
Milanese TR, Hartmann LC, Sellers TA, Frost MH, Vierkant RA, Maloney SD, Pankratz VS, Degnim AC, Vachon CM, Reynolds CA, Thompson RA, Melton LJ 3rd, Goode EL, Visscher DW (2006) Age-related lobular involution and risk of breast cancer. J Natl Cancer Inst 98(22):1600–1607. doi:10.1093/jnci/djj439
Pankratz VS, Degnim AC, Frank RD, Frost MH, Visscher DW, Vierkant RA, Hieken TJ, Ghosh K, Tarabishy Y, Vachon CM, Radisky DC, Hartmann LC (2015) Model for individualized prediction of breast cancer risk after a benign breast biopsy. J Clin Oncol 33(8):923–929. doi:10.1200/JCO.2014.55.4865
Said SM, Visscher DW, Nassar A, Frank RD, Vierkant RA, Frost MH, Ghosh K, Radisky DC, Hartmann LC, Degnim AC (2015) Flat epithelial atypia and risk of breast cancer: A Mayo cohort study. Cancer 121(10):1548–1555. doi:10.1002/cncr.29243
Korn EL, Graubard BI, Midthune D (1997) Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 145(1):72–80
McKian KP, Reynolds CA, Visscher DW, Nassar A, Radisky DC, Vierkant RA, Degnim AC, Boughey JC, Ghosh K, Anderson SS, Minot D, Caudill JL, Vachon CM, Frost MH, Pankratz VS, Hartmann LC (2009) Novel breast tissue feature strongly associated with risk of breast cancer. J Clin Oncol 27(35):5893–5898
Radisky DC, Hartmann LC (2009) Mammary involution and breast cancer risk: transgenic models and clinical studies. J Mammary Gland Biol Neoplasia 14(2):181–191
Henson DE, Tarone RE, Nsouli H (2006) Lobular involution: the physiological prevention of breast cancer. J Natl Cancer Inst 98(22):1589–1590
Ghosh K, Hartmann LC, Reynolds C, Visscher DW, Brandt KR, Vierkant RA, Scott CG, Radisky DC, Sellers TA, Pankratz VS, Vachon CM (2010) Association between mammographic density and age-related lobular involution of the breast. J Clin Oncol 28(13):2207–2212. doi:10.1200/JCO.2009.23.4120
Ghosh K, Vachon CM, Pankratz VS, Vierkant RA, Anderson SS, Brandt KR, Visscher DW, Reynolds C, Frost MH, Hartmann LC (2010) Independent association of lobular involution and mammographic breast density with breast cancer risk. J Natl Cancer Inst 102(22):1716–1723. doi:10.1093/jnci/djq414
Cichon MA, Degnim AC, Visscher DW, Radisky DC (2010) Microenvironmental influences that drive progression from benign breast disease to invasive breast cancer. J Mammary Gland Biol Neoplasia 15(4):389–397. doi:10.1007/s10911-010-9195-8
DeSantis C, Ma J, Bryan L, Jemal A (2013) Breast cancer statistics. CA Cancer J Clin 64(1):52–62. doi:10.3322/caac.21203
Benz CC (2008) Impact of aging on the biology of breast cancer. Crit Rev Oncol Hematol 66(1):65–74. doi:10.1016/j.critrevonc.2007.09.001
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Financial support
This study was supported by the National Cancer Institute (CA187112 to ACD); Bankhead-Coley Foundation (5BC02 to DCR and AN); Mayo Clinic Breast Cancer-Specialized Program of Research Excellence (SPORE CA116201 to DWV, DCR, AN, and LCH).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Radisky, D.C., Visscher, D.W., Frank, R.D. et al. Natural history of age-related lobular involution and impact on breast cancer risk. Breast Cancer Res Treat 155, 423–430 (2016). https://doi.org/10.1007/s10549-016-3691-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3691-5