Abstract
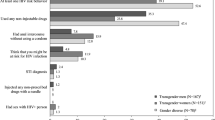
The aim of this study is to investigate HIV-related healthcare needs and access barriers for Brazilian transgender and gender diverse people. Data were collected from gender identity clinics and the questionnaire was also made available on the Internet. Out of the 543 participants—62.1% (n = 337) transgender women, 28.7 (n = 156) transgender men and 9.2% (n = 50) gender diverse people, 63.7% had been tested at least once in their lives. The prevalence of self-reported HIV-positive status among transgender women was 16.5%, of which 92.0% reported having a physician with whom they regularly consulted about HIV, whereas none of the transgender men or gender diverse people reported HIV-positive status. In addition, 8.2% of transgender men and 12.5% of gender diverse people did not know their serological status. Finally, 71.0% of the participants were unfamiliar with post-exposure prophylaxis. The study discusses the need for adequate behavior-oriented HIV health policies and training of healthcare professionals regarding the needs of Brazilian transgender and gender diverse people.
Similar content being viewed by others
References
Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infec Dis. 2013;13(3):214–22. https://doi.org/10.1016/S1473-3099(12)70315-8.
Poteat T, Wirtz AL, Radix A, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385(9964):274–86. https://doi.org/10.1016/S0140-6736(14)60833-3.
Costa AB, Fontanari AMV, Jacinto MM, et al. Population-based HIV prevalence and associated factors in male-to-female transsexuals from southern Brazil. Arch Sex Behav. 2015;44(2):521–4. https://doi.org/10.1007/s10508-014-0386-z.
Grinsztejn B, Jalil EM, Monteiro L, et al. Unveiling of HIV dynamics among transgender women: a respondent-driven sampling study in Rio de Janeiro, Brazil. Lancet HIV. 2017;4(4):169–76. https://doi.org/10.1016/s2352-3018(17)30015-2.
Bauer GR, Travers R, Scanlon K, Coleman TA. High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: a province-wide respondent-driven sampling survey. BMC Public Health. 2012;12(1):1–12. https://doi.org/10.1186/1471-2458-12-292.
Herbst JH, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. https://doi.org/10.1007/s10461-007-9299-3.
Reisner SL, Murchison GR. A global research synthesis of HIV and STI biobehavioural risks in female-to-male transgender adults. Glob Public Health. 2016;11(7–8):866–87. https://doi.org/10.1080/17441692.2015.1134613.
Scheim IA, Jackson R, James L, Sharp Dopler T, Pyne J, Bauer GR. Barriers to well-being for aboriginal gender-diverse people: results from the Trans PULSE Project in Ontario, Canada. Ethn Inequal Health Soc Care. 2013;6(4):108–20. https://doi.org/10.1108/EIHSC-08-2013-0010.
Costa AB, Peroni RO, Camargo ES, Pasley A, Nardi HC. Prejudice toward gender and sexual diversity in a Brazilian Public University: prevalence, awareness, and the effects of education. Sex Res Social Policy. 2015;12(4):261–72. https://doi.org/10.1007/s13178-015-0191-z.
Cerqueira-Santos E, Calvetti PU, Rocha K, Moura A, Barbosa L, Herme J. Percepção de Usuários Gays, Lésbicas, Bissexuais e Transgêneros, Transexuais e Travestis do Sistema Único de Saúde [Perception of gay, lesbian, bisexual and transgender, transsexual and travesti users about Brazilian unified health system]. Interam J Psychol. 2010;44(2):235–45. https://doi.org/10.1007/s10508-014-0386-z.
Balzer C, Hutta JS, Adrián T, Hyndal P. Transrespect versus transphobia worldwide: a comparative review of the human-rights situation of gender-variant/trans people. Berlin: Transgender Europe (TGEU); 2012.
Costa AB, Rosa FHT, Pase PF, Fontanari AMV, Catelan RF, Mueller A, et al. Healthcare needs of and access barriers for Brazilian transgender and gender diverse people. J Immigr Minor Health. 2016. https://doi.org/10.1007/s10903-016-0527-7.
Andrinopoulos K, Hembling J, Guardado ME, Maria Hernandez F, Nieto AI, Melendez G. Evidence of the negative effect of sexual minority stigma on HIV testing among MSM and transgender women in San Salvador, El Salvador. AIDS Behav. 2015;19(1):60–71. https://doi.org/10.1007/s10461-014-0813-0.
Bao A, Colby DJ, Trang T, et al. Correlates of HIV testing among transgender women in Ho Chi Minh, Vietnam. AIDS Behav. 2016;20(Suppl 3):371–8. https://doi.org/10.1007/s10461-016-1574-8.
Pal K, Ngin C, Tuot S, et al. Acceptability study on HIV self-testing among transgender women, men who have sex with men, and female entertainment workers in Cambodia: a qualitative analysis. PLoS ONE. 2016;11(11):e0166129. https://doi.org/10.1371/journal.pone.0166129.
Lippman SA, Moran L, Sevelius J, et al. Acceptability and feasibility of HIV self-testing among transgender women in San Francisco: a mixed methods pilot study. AIDS Behav. 2016;20(4):928–38. https://doi.org/10.1007/s10461-015-1236-2.
Frye V, Wilton L, Hirshfied S, et al. “Just because it’s out there, people aren’t going to use it”: HIV self-testing among young, black MSM, and transgender women. AIDS Patient Care STDS. 2015;29(11):617–24. https://doi.org/10.1089/apc.2015.0100.
Logie CH, Lacombe-Duncan A, Brien N, et al. Barriers and facilitators to HIV testing among young men who have sex with men and transgender women in Kingston, Jamaica: a qualitative study. J Int AIDS Soc. 2017;20(1):1–9. https://doi.org/10.7448/IAS.20.1.21385.
Woodford MR, Chakrapani V, Newman PA, Shunmugam M. Barriers and facilitators to voluntary HIV testing uptake among communities at high risk of HIV exposure in Chennai, India. Glob Public Health. 2015. https://doi.org/10.1080/17441692.2015.1057757.
Wirtz AL, Clouse E, Veronese V, et al. New HIV testing technologies in the context of a concentrated epidemic and evolving HIV prevention: qualitative research on HIV self-testing among men who have sex with men and transgender women in Yangon, Myanmar. PLoS ONE. 2017;20(1):1–9. https://doi.org/10.7448/IAS.20.1.21796.
Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24. https://doi.org/10.1016/S0277-9536(02)00304-0.
Boerma JT, Weir SS. Integrating demographic and epidemiological approaches to research on HIV/AIDS: the proximate-determinants framework. J Infect Dis. 2005;191(Supp 1):S61–7. https://doi.org/10.1086/425282.
Lewis ND. Is the social–ecological framework useful in understanding infectious diseases? The case of HIV/AIDS. EcoHealth. 2005;2(4):343–8.
TransPULSE. Provincial survey. 2012. http://transpulseproject.ca/wp-content/uploads/2012/05/Trans-PULSE-survey-information-only-copy-2012.pdf.
Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, Austin SB. Monitoring the health of transgender and other gender minority populations: validity of natal sex and gender identity survey items in a U.S. national cohort of young adults. BMC Public Health. 2014;14(1):1224. https://doi.org/10.1186/1471-2458-14-1224.
Carvalho M, Carrara S. Em direito a um futuro trans?: contribuição para a história do movimento de travestis e transexuais no Brasil [Towards a trans future? Contributions to a history of the travesti and transsexual movement in Brazil]. Sex Salud Soc. 2013;14:319–51. https://doi.org/10.1590/s1984-64872013000200015.
Barbosa C. “Doidas e putas”: usos das categorias travesti e transexual [“Freaks and whores”: uses of travesti and transsexual categories]. Sex Salud Soc. 2013;14(2):352–79. https://doi.org/10.1590/s1984-64872013000200016.
Socías ME, Marshall BD, Arístegui I, et al. Factors associated with healthcare avoidance among transgender women in Argentina. Int J Equity Health. 2014;13(1):1–12. https://doi.org/10.1186/s12939-014-0081-7.
Pinheiro Junior FM, Kendall C, Martins TA, et al. Risk factors associated with resistance to HIV testing among transwomen in Brazil. AIDS Care. 2016;28(1):92–7. https://doi.org/10.1080/09540121.2015.1066751.
Pascom ARP, Arruda MR, Simão MBG. Pesquisa de conhecimentos, atitudes e práticas na população brasileira de 15 a 64 anos 2008 [Research on knowledge, attitudes and practices in the Brazilian population from 15 to 64 years-old 2008]. Ministério da Saúde, Brasília, Brazil; 2011.
Sousa PJD, Ferreira LOC, Sá JBD. Estudo descritivo da homofobia e vulnerabilidade ao HIV/Aids das travestis da Região Metropolitana do Recife, Brasil [Descriptive study of homophobia and vulnerability to HIV/Aids of the transvestites in the Metropolitan Region of Recife, Brazil]. Cien Saude Colet. 2013;18(8):2239–51. https://doi.org/10.1590/S1413-81232013000800008.
Martins TA, Kerr LRF, Macena RH, et al. Travestis, an unexplored population at risk of HIV in a large metropolis of northeast Brazil: a respondent-driven sampling survey. AIDS Care. 2013;25(5):606–12. https://doi.org/10.1080/09540121.2012.726342.
Brazilian Ministry of Health. Boletim epidemiológico AIDS e DST [Epidemiological data on AIDS and IST]. Ministério da Saúde, Brasília, Brazil; 2012.
World Health Organization. Post-exposure prophylaxis to prevent HIV infection. Geneva: WHO; 2014. http://www.who.int/hiv/topics/prophylaxis/info/en/.
Silva AS, Barboza R. Exclusão social e consciência política: luta e militância de transgêneros no ENTLAIDS [Social exclusion and political awareness: transgender struggle and activism in ENTLAIDS]. Cadernos CERU. 2009;20:257–76.
Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19(2):69–79. https://doi.org/10.1093/heapol/czh009.
Weinhardt LS, Forsyth AD, Carey MP, Jaworski BC, Durant LE. Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27(2):155–80.
Mota RMS, Kerr LRFS, Kendall C, Pinho A, de Mello MB, Dourado I, et al. Reliability of self-report of HIV status among men who have sex with men in Brazil. JAIDS. 2011;57:S153–6.
Funding
This study was funded by the Universal Issuance 477016/2013-8 Universal Public Call 14/2013—Track C by of the Brazilian National Council of Technological and Scientific Development (CNPQ), and through PROEX and PDSE grants from the Coordination for the Improvement of Higher Education Personnel (CAPES).
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly and are in agreement regarding the contents of this manuscript. AC designed the study, wrote the protocol, was responsible for analysis, and participated in data interpretation, draft of the article and final approval of this version. AF, JS and RC participated in data analysis and interpretation, draft of the article and final approval of this version. HF, DG, KS and PP participated in the study design and final approval of the article. AS, HN, ML and SK were responsible for the study design and data interpretation, as well as draft of the article and its final approval.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Costa, A.B., Fontanari, A.M.V., Catelan, R.F. et al. HIV-Related Healthcare Needs and Access Barriers for Brazilian Transgender and Gender Diverse People. AIDS Behav 22, 2534–2542 (2018). https://doi.org/10.1007/s10461-017-2021-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-2021-1