Abstract
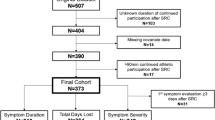
The purpose of this study was to compare global and specific health-related quality of life (HRQOL) throughout concussion recovery between those with and without concussion history. Student-athletes diagnosed with concussion completed global (Short Form-12v2; SF-12) and specific (Hospital Anxiety and Depression Scale: HADS) HRQOL assessments at baseline, 24–48 h, asymptomatic, return-to-play, and 6-months post-injury. Baseline scores were compared to post-injury time points for SF-12 subscores (physical and mental; PCS-12, MCS-12) and HADS subscores (depression and anxiety; HADS-D, HADS-A). We conducted a 2 × 5 mixed model ANOVA for group (with and without concussion history) and time (four post-injury assessments compared to baseline). We did not observe interaction or main effects for group, except those with concussion history had worse HADS-D subscores than those without concussion history. PCS-12 subscores were worse at 24–48 h, asymptomatic, and return-to-play compared to baseline, but returned to baseline 6-months post-injury. MCS-12 subscores did not differ at any time points. HADS-D subscores worsened 24–48 h post-injury, but improved for additional assessments compared to baseline. HADS-A improved post-injury compared to baseline at asymptomatic, return-to-play, and 6-month assessments, but was similar to baseline 24–48 h post-injury. HRQOL physical aspects slightly worsened post-injury and restored to baseline after returning to play.




Similar content being viewed by others
References
Bailey, C. M., H. L. Samples, D. K. Broshek, J. R. Freeman, and J. T. Barth. The relationship between psychological distress and baseline sports-related concussion testing. Clin. J. Sport Med. 20(4):272–277, 2010.
Broglio, R. C. Cantu, and G. A. Gioia. National Athletic Trainers’ Association position statement: management of sport concussion. J. Athl. Train. 49(2):245–265, 2014.
Broglio, S. P., M. McCrea, T. McAllister, et al. A national study on the effects of concussion in collegiate athletes and US Military Service Academy Members: the NCAA-DoD Concussion Assessment, Research and Education (CARE) Consortium Structure and Methods. Sports Med. 47(7):1437–1451, 2017.
Brooks, M. A., K. Peterson, K. Biese, J. Sanfilippo, B. C. Heiderscheit, and D. R. Bell. Concussion increases odds of sustaining a lower extremity musculoskeletal injury after return to play among collegiate athletes. Am. J. Sports Med. 44(3):742–747, 2016.
Cho, C.-H., K.-S. Song, I. Hwang, and J. J. Warner. Does rotator cuff repair improve psychologic status and quality of life in patients with rotator cuff tear? Clin. Orthopaedics Relat. Res.® 473(11):3494–3500, 2015.
Covassin, T., R. J. Elbin, III, E. Larson, and A. P. Kontos. Sex and age differences in depression and baseline sport-related concussion neurocognitive performance and symptoms. Clin. J. Sport Med. 22(2):98–104, 2012.
Cross, M., S. Kemp, A. Smith, G. Trewartha, and K. Stokes. Professional Rugby Union players have a 60% greater risk of time loss injury after concussion: a 2-season prospective study of clinical outcomes. Br. J. Sports Med. 2015:bjsports-2015-094982, 2015.
Crossing the Quality Chasm. A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001.
Da Silva-Gane, M., D. Wellsted, H. Greenshields, S. Norton, S. M. Chandna, and K. Farrington. Quality of life and survival in patients with advanced kidney failure managed conservatively or by dialysis. Clin. J. Am. Soc. Nephrol. 7(12):2002–2009, 2012.
Decq, P., N. Gault, M. Blandeau, et al. Long-term consequences of recurrent sports concussion. Acta Neurochir. 158(2):289–300, 2016.
Fitzpatrick, R., C. Davey, J. Buxton, and D. Jones. Evaluating patient-based outcome measures for use in clinical trials. Health Technol. Assess. 1(14):1–69, 1998.
Gandek, B., J. E. Ware, N. K. Aaronson, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J. Clin. Epidemiol. 51(11):1171–1178, 1998.
Gilbert, F. C., G. T. Burdette, A. B. Joyner, T. A. Llewellyn, and T. A. Buckley. Association between concussion and lower extremity injuries in collegiate athletes. Sports Health. 8(6):561–567, 2016.
Guskiewicz, K., S. W. Marshall, J. Bailes, et al. Recurrent concussion and risk of depression in retired professional football players. Med. Sci. Sports Exerc. 39(6):903, 2007.
Herman, D. C., D. Jones, A. Harrison, et al. Concussion may increase the risk of subsequent lower extremity musculoskeletal injury in collegiate athletes. Sports Med. 47(5):1003–1010, 2017.
Howell, D. R., R. C. Lynall, T. A. Buckley, and D. C. Herman. Neuromuscular control deficits and the risk of subsequent injury after a concussion: a scoping review. Sports Med. 48:1097–1115, 2018.
Hutchison, M., L. M. Mainwaring, P. Comper, D. W. Richards, and S. M. Bisschop. Differential emotional responses of varsity athletes to concussion and musculoskeletal injuries. Clin. J. Sport Med. 19(1):13–19, 2009.
Hutchison, M. G., L. Mainwaring, A. Senthinathan, N. Churchill, S. Thomas, and D. Richards. Psychological and physiological markers of stress in concussed athletes across recovery milestones. J. Head Trauma Rehabil. 32(3):E38–E48, 2017.
Hyodo, I., K. Eguchi, N. Takigawa, et al. Psychological impact of informed consent in hospitalized cancer patients. Support Care Cancer. 7(6):396–399, 1999.
Jalan, R., R. Gooday, R. E. O’Carroll, D. N. Redhead, R. A. Elton, and P. C. Hayes. A prospective evaluation of changes in neuropsychological and liver function tests following transjugular intrahepatic portosystemic stent-shunt. J Hepatol. 23(6):697–705, 1995.
Kerr, Z. Y., S. W. Marshall, H. P. Harding, and K. M. Guskiewicz. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am. J. Sports Med. 40(10):2206–2212, 2012.
Kuehl, M. D., A. R. Snyder, S. E. Erickson, and T. C. V. McLeod. Impact of prior concussions on health-related quality of life in collegiate athletes. Clin. J. Sport Med. 20(2):86–91, 2010.
Leach, C. A., R. C. Bay, and T. C. V. McLeod. Baseline self-report symptoms and health-related quality of life in high school athletes: influence of sex and prior concussion history. Athl. Train. Sports Health Care. 5(3):115–122, 2013.
Lynall, R. C., T. C. Mauntel, D. A. Padua, and J. P. Mihalik. Acute lower extremity injury rates increase after concussion in college athletes. Med. Sci. Sports Exerc. 47(12):2487–2492, 2015.
Lynall, R. C., T. C. Mauntel, R. T. Pohlig, et al. Lower extremity musculoskeletal injury risk after concussion recovery in high school athletes. J. Athl. Train. 52(11):1028–1034, 2017.
Mainwaring, L. M., S. M. Bisschop, R. E. Green, et al. Emotional reaction of varsity athletes to sport-related concussion. J. Sport Exerc. Psychol. 26(1):119–135, 2004.
Martens, E. J., and P. de Jonge. Developing depression after a myocardial infarction increases risk of cardiac mortality but pre-existing depression does not. Evid. Based Ment. Health. 12(1):8, 2009.
McLeod, T. C. V., R. C. Bay, and A. R. Snyder. Self-reported history of concussion affects health-related quality of life in adolescent athletes. Athl. Train. Sports Health Care. 2(5):219–226, 2010.
Moran, L. M., H. G. Taylor, J. Rusin, et al. Quality of life in pediatric mild traumatic brain injury and its relationship to postconcussive symptoms. J. Pediatr. Psychol. 37(7):736–744, 2011.
National Collegiate Athletic Association. Concussion Management and Diagnosis Best Practices: Diagnosis and Management of Sport-Related Concussion Guidelines. Indianapolis: National Collegiate Athletic Association, 2014.
Nordström, A., P. Nordström, and J. Ekstrand. Sports-related concussion increases the risk of subsequent injury by about 50% in elite male football players. Br. J. Sports Med. 48(19):1447–1450, 2014.
Novak, Z., M. Aglipay, N. Barrowman, et al. Association of persistent postconcussion symptoms with pediatric quality of life. JAMA Pediatr. 170(12):e162900–e162900, 2016.
Parker, S. L., S. K. Mendenhall, D. N. Shau, et al. Minimum clinically important difference in pain, disability, and quality of life after neural decompression and fusion for same-level recurrent lumbar stenosis: understanding clinical versus statistical significance. J. Neurosurg. Spine. 16(5):471–478, 2012.
Russell, K., E. Selci, S. Chu, S. Fineblit, L. Ritchie, and M. J. Ellis. Longitudinal assessment of health-related quality of life following adolescent sports-related concussion. J. Neurotrauma. 34:2147–2153, 2017.
Sackett, D. L., W. M. Rosenberg, J. M. Gray, R. B. Haynes, and W. S. Richardson. Evidence based medicine: what it is and what it isn’t. Br. Med. J. Publ. Group 312:71–73, 1996.
SF-12v2 Health Survey. How to Score the SF-12v2 Summary Measures. Tehran: SF-12v2 Health Survey: QualityMetric, Inc, 2000.
Smid, D. E., F. M. Franssen, S. Houben-Wilke, et al. Responsiveness and MCID estimates for CAT, CCQ, and HADS in patients with COPD undergoing pulmonary rehabilitation: a prospective analysis. J. Am. Med. Dir. Assoc. 18(1):53–58, 2017.
Snaith, R. P. The hospital anxiety and depression scale. Health Qual Life Outcomes. 1(1):29, 2003.
Snyder, A. R., J. T. Parsons, T. C. Valovich McLeod, R. Curtis Bay, L. A. Michener, and E. L. Sauers. Using disablement models and clinical outcomes assessment to enable evidence-based athletic training practice, part I: disablement models. J. Athl. Train. 43(4):428–436, 2008.
Spira, J. L., C. E. Lathan, J. Bleiberg, and J. W. Tsao. The impact of multiple concussions on emotional distress, post-concussive symptoms, and neurocognitive functioning in active duty United States marines independent of combat exposure or emotional distress. J. Neurotrauma. 31(22):1823–1834, 2014.
Steer, J., G. J. Gibson, and S. C. Bourke. Longitudinal change in quality of life following hospitalisation for acute exacerbations of COPD. BMJ Open Respir. Res. 2(1):e000069, 2015.
Stocker, R. P., H. Khan, L. Henry, and A. Germain. Effects of sleep loss on subjective complaints and objective neurocognitive performance as measured by the immediate post-concussion assessment and cognitive testing. Arch. Clin. Neuropsychol. 32(3):349–368, 2017.
Tsai, J., J. M. Whealin, J. C. Scott, I. Harpaz-Rotem, and R. H. Pietrzak. Examining the relation between combat-related concussion, a novel 5-factor model of posttraumatic stress symptoms, and health-related quality of life in Iraq and Afghanistan veterans. J. Clin. Psychiatry. 73(8):1110–1118, 2012.
Turner, S., J. Langdon, G. Shaver, V. Graham, K. Naugle, and T. Buckley. Comparison of psychological response between concussion and musculoskeletal injury in collegiate athletes. Sport Exerc. Perform. Psychol. 6(3):277, 2017.
Valovich McLeod, T. C. R.-M., and K. Johna. Clinical outcomes assessment for the mangement of sport-related concussion. J. Sport Rehabil. 20:46–60, 2011.
Ware Jr, J. E., M. Kosinski, and S. D. Keller. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales (2nd ed.). Boston, MA: The Health Institute, New England Medical Center, 1995.
Ware, Jr, J. E., M. Kosinski, and S. D. Keller. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 34(3):220–233, 1996.
Yengo-Kahn, A. M., and G. Solomon. Are psychotropic medications associated with differences in baseline neurocognitive assessment scores for young athletes? A pilot study. Phys. Sportsmed. 43(3):227–235, 2015.
Zigmond, A. S., and R. P. Snaith. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67(6):361–370, 1983.
Acknowledgments
CARE Consortium Investigators are as follows: April Marie (Reed) Hoy, MS, ATC (Azusa Pacific University); Joseph B. Hazzard Jr, EdD, ATC (Bloomsburg University); Louise A. Kelly, PhD (California Lutheran University); Justus D. Ortega, PhD (Humboldt State University); Nicholas Port, PhD (Indiana University); Margot Putukian MD (Princeton University); T. Dianne Langford, PhD, and Ryan Tierney, PhD, ATC (Temple University); Darren E. Campbell, MD, and Gerald McGinty, DPT (United States Air Force Academy); Patrick O’Donnell, MHA (United States Coast Guard Academy); Holly J. Benjamin MD (University of Chicago); Thomas Buckley, EdD, ATC, and Thomas W. Kaminski, PhD, ATC (University of Delaware); James R. Clugston, MD, MS (University of Florida); Julianne D. Schmidt, PhD, ATC (University of Georgia); Luis A. Feigenbaum, DPT, ATC (University of Miami); James T. Eckner, MD, MS (University of Michigan); Kevin Guskiewicz, PhD, ATC, and Jason P. Mihalik, PhD, CAT(C), ATC (University of North Carolina at Chapel Hill); Jessica Dysart Miles, PhD, ATC (University of North Georgia); Christina L. Master, MD (University of Pennsylvania); Micky Collins, PhD, and Anthony P. Kontos, PhD (University of Pittsburgh Medical Center); Jeffrey J. Bazarian, MD, MPH (University of Rochester); Sara P.D. Chrisman, MD, MPH (University of Washington); Christopher Todd Bullers, MD, and Christopher M. Miles, MD (Wake Forest University); Brian H. Dykhuizen, MS, ATC (Wilmington College).
Funding
This project was supported, in part, with support from the Grand Alliance Concussion Assessment, Research, and Education (CARE) Consortium, funded, in part by the National Collegiate Athletic Association (NCAA) and the Department of Defense (DOD). The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Psychological Health and Traumatic Brain Injury Program under Award NO W81XWH-14-2-0151. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense (DHP funds).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Associate Editor Stefan Duma oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Weber, M.L., Lynall, R.C., Hoffman, N.L. et al. Health-Related Quality of Life Following Concussion in Collegiate Student-Athletes With and Without Concussion History. Ann Biomed Eng 47, 2136–2146 (2019). https://doi.org/10.1007/s10439-018-02151-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-018-02151-7