Abstract
Background
We propose a modified quality-adjusted life year (QALY) calculation that aims to be consistent with guidance for interpreting change in patient-reported outcomes. This calculation incorporates the minimally important difference (MID) in generic preference-based health-related quality of life (HRQL) change scores to reflect what might be considered meaningful HRQL improvement/deterioration. In doing so, we review common issues in QALY calculations such as adjustment for baseline scores and standardizing for between-group differences.
Methods
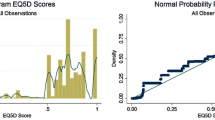
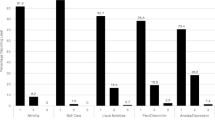
Using EQ-5D-5L outcome data from the Alberta TEAMCare-Primary Care Network trial in the management of depression for patients with type 2 diabetes (n = 98), this study compared results from different QALY calculation methods to investigate the impact of (i) adjusting for baseline HRQL score, (ii) standardizing between-group differences at baseline, and (iii) adjusting for ‘meaningful’ HRQL changes. The following QALY calculation methods are examined: area under curve (QALY-AUC), change from baseline (QALY-CFB), regression modelling (QALY-R), and incorporating an MID for HRQL changes from baseline (QALY-MID).
Results
The incremental QALY-AUC estimate favoured the Collaborative Care group (0.031) while the incremental QALY-CFB (−0.028) estimate favoured Enhanced Care. Adjusting for meaningful HRQL changes resulted in a crude incremental QALY-MID of −0.023; however, after adjusting for between-group differences at baseline, QALY-R and adjusted incremental QALY-MID estimates were −0.007 and −0.001, respectively. In addition, recursive regression analyses showed that very low baseline HRQL scores impact incremental QALY estimates.
Conclusions
Uncertainty in incremental QALY estimates reflects uncertainty in the value of small within-individual change as well as the impact of small differences between groups at baseline. Applying a responder-definition approach yielded crude and adjusted QALY-MID estimates that were more in favour of Collaborative Care than QALY-CFB and QALY-R estimates, respectively, suggesting that ambiguous small changes in HRQL scores have the potential to influence QALY outcomes used in economic or non-economic applications.





Similar content being viewed by others
Data availability
The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study.
Code availability
The R code used to conduct the analyses in this study is available from the corresponding author on reasonable request.
References
Nord, E.: Quality-adjusted life-years. In: Cuyler, A.J. (ed.) Encyclopedia of health economics, pp. 231–234. Elsevier (2014)
Olsen, J.A.: Principles in health economics and policy. Oxford University Press (2017)
Manca, A., Hawkins, N., Sculpher, M.J.: Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 14, 487–496 (2005). https://doi.org/10.1002/hec.944
Coon, C.D., Cook, K.F.: Moving from significance to real-world meaning: methods for interpreting change in clinical outcome assessment scores. Qual. Life Res. 27, 33–40 (2018). https://doi.org/10.1007/s11136-017-1616-3
Food, U.S., Administration, D.: Patient-focused drug development guidance public workshop-discussion document: incorporating clinical outcome assessments into endpoints for regulatory decision-making. FDA (2019)
MacKillop, E., Sheard, S.: Quantifying life: understanding the history of quality-adjusted life-years (QALYs). Soc. Sci. Med. 211, 359–366 (2018). https://doi.org/10.1016/j.socscimed.2018.07.004
Pickles, K., Lancsar, E., Seymour, J., Parkin, D., Donaldson, C., Carter, S.M.: Accounts from developers of generic health state utility instruments explain why they produce different QALYs: a qualitative study. Soc. Sci. Med. 240, 112560 (2019). https://doi.org/10.1016/j.socscimed.2019.112560
Kind, P., Lafata, J.E., Matuszewski, K., Raisch, D.: The use of QALYs in clinical and patient decision-making: issues and prospects. Value Health. 12(Suppl 1), S27-30 (2009). https://doi.org/10.1111/j.1524-4733.2009.00519.x
Ahmed, S., Berzon, R.A., Revicki, D.A., Lenderking, W.R., Moinpour, C.M., Basch, E., Reeve, B.B., Wu, A.W.: International society for quality of life research: the use of patient-reported outcomes (PRO) within comparative effectiveness research: implications for clinical practice and health care policy. Med. Care. 50, 1060–1070 (2012). https://doi.org/10.1097/MLR.0b013e318268aaff
Carr, A.J.: Measuring quality of life: are quality of life measures patient centred? BMJ 322, 1357–1360 (2001). https://doi.org/10.1136/bmj.322.7298.1357
Parkin, D., Appleby, J., Maynard, A.: Economics: the biggest fraud ever perpetrated on the world? Lancet 382, 11–15 (2013). https://doi.org/10.1016/S0140-6736(13)61178-2
Franklin, E.F., Nichols, H.M., Charap, E., Buzaglo, J.S., Zaleta, A.K., House, L.: Perspectives of patients with cancer on the quality-adjusted life year as a measure of value in healthcare. Value Health. 22, 474–481 (2019). https://doi.org/10.1016/j.jval.2018.09.2844
Mokkink, L.B., Terwee, C.B., Patrick, D.L., Alonso, J., Stratford, P.W., Knol, D.L., Bouter, L.M., de Vet, H.C.: The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual. Life Res. 19, 539–549 (2010). https://doi.org/10.1007/s11136-010-9606-8
Jayadevappa, R., Cook, R., Chhatre, S.: Minimal important difference to infer changes in health-related quality of life—a systematic review. J. Clin. Epidemiol. 89, 188–198 (2017). https://doi.org/10.1016/j.jclinepi.2017.06.009
Francis, D.O., McPheeters, M.L., Noud, M., Penson, D.F., Feurer, I.D.: Checklist to operationalize measurement characteristics of patient-reported outcome measures. Syst. Rev. 5, 129 (2016). https://doi.org/10.1186/s13643-016-0307-4
McClure, N.S., Al Sayah, F., Ohinmaa, A., Johnson, J.A.: Minimally important difference of the EQ-5D-5L index score in adults with type 2 diabetes. Value Health 21, 1090–1097 (2018). https://doi.org/10.1016/j.jval.2018.02.007
Carrasco-Labra, A., Devji, T., Qasim, A., Phillips, M.R., Wang, Y., Johnston, B.C., Devasenapathy, N., Zeraatkar, D., Bhatt, M., Jin, X., Brignardello-Petersen, R., Urquhart, O., Foroutan, F., Schandelmaier, S., Pardo-Hernandez, H., Hao, Q., Wong, V., Ye, Z., Yao, L., Vernooij, R.W.M., Huang, H., Zeng, L., Rizwan, Y., Siemieniuk, R., Lytvyn, L., Patrick, D.L., Ebrahim, S., Furukawa, T.A., Nesrallah, G., Schünemann, H.J., Bhandari, M., Thabane, L., Guyatt, G.H.: Minimal important difference estimates for patient-reported outcomes: A systematic survey. J. Clin. Epidemiol. 133, 61–71 (2021). https://doi.org/10.1016/j.jclinepi.2020.11.024
Revicki, D., Hays, R.D., Cella, D., Sloan, J.: Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J. Clin. Epidemiol. 61, 102–109 (2008). https://doi.org/10.1016/j.jclinepi.2007.03.012
Johnson, J.A., Sayah, FAl., Wozniak, L., Rees, S., Soprovich, A., Chik, C.L., Chue, P., Florence, P., Jacquier, J., Lysak, P., Opgenorth, A., Katon, W.J., Majumdar, S.R.: Controlled trial of a collaborative primary care team model for patients with diabetes and depression: rationale and design for a comprehensive evaluation. BMC Health Serv Res. (2012). https://doi.org/10.1186/1472-6963-12-258
Johnson, J.A., Al Sayah, F., Wozniak, L., Rees, S., Soprovich, A., Qiu, W., Chik, C.L., Chue, P., Florence, P., Jacquier, J., Lysak, P., Opgenorth, A., Katon, W., Majumdar, S.R.: Collaborative care versus screening and follow-up for patients with diabetes and depressive symptoms: results of a primary care-based comparative effectiveness trial. Diabetes Care 37, 3220–3226 (2014). https://doi.org/10.2337/dc14-1308
Johnson, J.A., Lier, D.A., Soprovich, A., Sayah, F., Qiu, W., Majumdar, S.R.: Cost-effectiveness evaluation of collaborative care for diabetes and depression in primary care. Am. J. Prev. Med. 5, e13–e20 (2016). https://doi.org/10.1016/j.amepre.2016.01.010
Olsen, J.A., Misajon, R.A.: A conceptual map of health-related quality of life dimensions: key lessons for a new instrument. Qual. Life Res. 29, 733–743 (2020). https://doi.org/10.1007/s11136-019-02341-3
EQ-5D: EuroQol group research foundation, http://www.euroqol.org/
Xie, F., Pullenayegum, E., Gaebel, K., Bansback, N., Bryan, S., Ohinmaa, A., Poissant, L., Johnson, J.A.: Canadian EQ-5D-5L valuation study group: a time trade-off-derived value set of the EQ-5D-5L for Canada. Med. Care. 54, 98–105 (2016). https://doi.org/10.1097/MLR.0000000000000447
Schisterman, E.F., Cole, S.R., Platt, R.W.: Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 20, 488–495 (2009). https://doi.org/10.1097/EDE.0b013e3181a819a1
Mills, T.C.: Testing for stability in regression models. In: Patterson, K., Mills, T.C. (eds.) Analysing economic data a concise introduction, pp. 231–243. Palgrave Macmillan (2014)
R Core Team: R: A language and environment for statistical computing. The R Foundation for Statistical Computing (2020)
Hunter, R.M., Baio, G., Butt, T., Morris, S., Round, J., Freemantle, N.: An educational review of the statistical issues in analysing utility data for cost-utility analysis. Pharmacoeconomics 33, 355–366 (2015). https://doi.org/10.1007/s40273-014-0247-6
Pearl, J., Mackenzie, D.: From buccaneers to guinea pigs: the genesis of causal inference: the book of why: the new science of cause and effect. Basic Books (2018)
Karimi, M., Brazier, J., Paisley, S.: Are preferences over health states informed? Health Qual. Life Outcomes 15, 105 (2017). https://doi.org/10.1186/s12955-017-0678-9
Brazier, J., Ara, R., Rowen, D., Chevrou-Severac, H.: A review of generic preference-based measures for use in cost-effectiveness models. Pharmacoeconomics 35, 21–31 (2017). https://doi.org/10.1007/s40273-017-0545-x
Ogorevc, M., Murovec, N., Fernandez, N.B., Rupel, V.P.: Questioning the differences between general public vs patient based preferences towards EQ-5D-5L defined hypothetical health states. Health Policy 123, 166–172 (2019). https://doi.org/10.1016/j.healthpol.2017.03.011
Dirksen, C.D.: The use of research evidence on patient preferences in health care decision-making: issues, controversies and moving forward. Expert Rev. Pharmacoeconomics Outcomes Res. 14, 785–794 (2014). https://doi.org/10.1586/14737167.2014.948852
Helgesson, G., Ernstsson, O., Åström, M., Burström, K.: Whom should we ask? A systematic literature review of the arguments regarding the most accurate source of information for valuation of health states. Qual. Life Res. (2020). https://doi.org/10.1007/s11136-020-02426-4
Korn, E.L., Othus, M., Chen, T., Freidlin, B.: Assessing treatment efficacy in the subset of responders in a randomized clinical trial. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 28, 1640–1647 (2017). https://doi.org/10.1093/annonc/mdx197
European Medicines Agency: Committee for medicinal products for human use (CHMP)—guideline on the evaluation of anticancer medicinal products in man. EMA (2017)
Funding
Financial support for this study was provided in part by a grant from Alberta Innovates awarded to NSM as a Graduate Studentship. The funding agreement ensured the author’s independence in designing the study, interpreting the data, writing, and publishing the study.
Author information
Authors and Affiliations
Contributions
NSM and JAJ conceived the study. JAJ was the investigator for the Alberta TEAMCare-PCN trial. MP and AO contributed to the study design. Material preparation, data collection and analysis were performed by NSM. The first draft of the manuscript was written by NSM and all authors commented on later versions of the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
JAJ and AO are members of the EuroQol Group. The views expressed by the authors in this paper do not necessarily reflect the views of the EuroQol Group. Other authors declare that they have no conflict of interest.
Ethics approval
This study followed requirements outlined in the Canadian Tri-Council Policy Statement: Ethical Conduct of Research Involving Humans. Ethics approval for the study was granted from the Health Research Ethics Board (HREB #Pro00087637) at the University of Alberta.
Consent to participate
Informed consent was obtained from all individual participants included in the TEAMCare-PCN trial.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McClure, N.S., Paulden, M., Ohinmaa, A. et al. Modifying the quality-adjusted life year calculation to account for meaningful change in health-related quality of life: insights from a pragmatic clinical trial. Eur J Health Econ 22, 1441–1451 (2021). https://doi.org/10.1007/s10198-021-01324-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-021-01324-x
Keywords
- Quality-adjusted life year
- Health-related quality of life
- Minimally important difference
- Type 2 diabetes
- Depression