Abstract
Background
A low protein diet (LPD) with essential amino acid ketoanalogue supplementation (KA) may contribute in improving of chronic kidney disease (CKD), while the exact mechanisms of KA’s effect are not established yet. We have conducted a prospective, randomized, controlled comparative study of LPD + KA and LPD alone in relation to serum Klotho, FGF-23 levels in CKD patients.
Methods
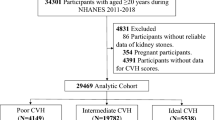
79 non-diabetic CKD 3b–4 stage patients, compliant with LPD diet (0.6 g/kg of body weight/day), had been selected. The patients were randomized into two groups. The first group (42 patients) received LPD + КA. The second group (37 patients) continued the LРD alone. In addition to routine tests, serum Klotho, FGF-23 levels, as well as bioimpedance analysis, sphygmography (stiffness (augmentation) indices (AI), central (aortal) blood pressure) with a «SphygmaCor» device; echocardiography (valvular calcification score (VCS) and LVMMI), were performed.
Results
There were body mass indices’ decrease (p = 0.046), including muscle body mass in men (p = 0.027) and woman (p = 0.044) in the LPD group to the end of study (14th month). In addition, lower FGF-23 (p = 0.029), and higher sKlotho (p = 0.037) were detected in the LPD + KA group compared to the LPD one. The increase in AI (p = 0.034), VCS (p = 0.048), and LVMMI (p = 0.023) was detected more often in the LPD group at the end of study.
Conclusion
LPD + KA provides support for nutrition status and contributes to more efficient correction of FGF-23 and Klotho abnormalities that may result in cardiovascular calcification and cardiac remodeling decreasing in CKD. At the same time, a prolonged LPD alone may lead to malnutrition.



Similar content being viewed by others
References
Levin A, Stevens PE, Bilous RW, Coresh J, De Francisco ALM, De Jong PE, et al. Kidney disease: Improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150.
Eckardt K-U, Kasiske BL, et al. KDIGO clinical practice guideline for the diagnosis, evolution, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Elsevier. 2009;76:S1–130.
Piccoli GB, Capizzi I, Vigotti FN, Leone F, D’Alessandro C, Giuffrida D, et al. Low protein diets in patients with chronic kidney disease: a bridge between mainstream and complementary-alternative medicines? BMC Nephrol. 2016;17:1–13.
Rysz J, Franczyk B, Ciałkowska-Rysz A, Gluba-Brzózka A. The effect of diet on the survival of patients with chronic kidney disease. Nutrients. 2017;9(5):495. https://doi.org/10.3390/nu9050495. ,.
Snelson M, Clarke RE, Coughlan MT. Stirring the pot: can dietary modification alleviate the burden of CKD? Nutrients. 2017; 9(3): 265. https://doi.org/10.3390/nu9030265.
Di Iorio BV, De Nicola BR, Minutolo L, Zamboli R, Trucillo P. et al. Very low protein diet supplemented with ketoanalogs improves blood pressure control in chronic kidney disease. Kidney Int. 2007;71(3):245–51. https://doi.org/10.1038/sj.ki.5001955.
Zha Y, Qian Q. Protein nutrition and malnutrition in CKD and ESRD. Nutrients. 2017;9(3):208. https://doi.org/10.3390/nu9030208.
Gutiérrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med. 2008;359:584–92.
Hu MC, Shi M, Zhang J, Quiñones H, Griffith C, Kuro-o M, et al. Klotho deficiency causes vascular calcification in chronic kidney disease. J Am Soc Nephrol Am Soc Nephrol. 2011;22:124–36.https://doi.org/10.1681/ASN.2009121311.
Seiler S, Rogacev KS, Roth HJ, Shafein P, Emrich I, Neuhaus S, et al. Associations of FGF-23 and sklotho with cardiovascular outcomes among patients with CKD stages 2–4. Clin J Am Soc Nephrol. 2014;9:1049–58. https://doi.org/10.2215/CJN.07870713.
Krieger NS, Culbertson CD, Kyker-Snowman K, Bushinsky DA. Metabolic acidosis increases fibroblast growth factor 23 in neonatal mouse bone. Am J Physiol Renal Physiol. 2012;303(3):431–6. https://doi.org/10.1152/ajprenal.00199.2012.
Dalton GD, Xie J, An S-W, Huang C-L. New insights into the mechanism of action of soluble klotho. Front Endocrinol (Lausann). 2017;8:323. https://doi.org/10.3389/fendo.2017.00323.
Bartali B, Semba RD, Araujo AB. Klotho, FGF21 and FGF23: novel pathways to musculoskeletal health? J Frailty Aging. 2013;2(4):179–83. https://doi.org/10.14283/jfa.2013.26.
Yilmaz MI, Sonmez A, Saglam M, Yaman H, Kilic S, Demirkaya E, et al. FGF-23 and vascular dysfunction in patients with stage 3 and 4 chronic kidney disease. Kidney Int. 2010;78:679–85. https://doi.org/10.1038/ki.2010.194.
Lu X, Hu MC. Klotho/FGF23 axis in chronic kidney disease and cardiovascular disease. Kidney Dis Karger Publ. 2016;17:1–9. https://doi.org/10.1159/000452880.
Kuczera P, Adamczak M, Wiecek A. Fibroblast growth factor-23—a potential uremic toxin. Toxins (Basel). 2016;8(12):369. https://doi.org/10.3390/toxins8120369.
Isakova T, Wahl P, Vargas GS, Gutiérrez OM, Scialla J, Xie H, et al. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 2011;79:1370–8.
Hu MC, Shiizaki K, Kuro-O M, Moe OW. Fibroblast growth factor 23 and klotho: physiology and pathophysiology of an endocrine network of mineral metabolism. Annu Rev Physiol. 2013. p. 503–33. https://doi.org/10.1146/annurev-physiol-030212-183727.
Neyra JA, Hu MC. αKlotho and chronic kidney disease. Vitam Horm. 2016. p. 257–310. https://doi.org/10.1016/bs.vh.2016.02.007.
Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390:45–51.
Kurosu H, Yamamoto M, Clark JD, Pastor JV, Nandi A, Gurnani P, et al. Suppression of aging in mice by the Hormone Klotho. Science. 2005;309:1829–33.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med Massachusetts Med Soc. 2004;351:1296–305.
Hu MC, Kuro-o M, Moe OW. Secreted Klotho And Chronic Kidney disease. Adv Exp Med Biol. 2012;728:126–57. https://doi.org/10.1007/978-1-4614-0887-1_9.
Hu M-C, Shi M, Cho HJ, Zhang J, Pavlenco A, Liu S, et al. The erythropoietin receptor is a downstream effector of Klotho-induced cytoprotection. Kidney Int. 2013;84:468–81.
De Borst MH, Vervloet MG, Ter Wee PM, Navis G. Cross talk between the renin-angiotensin-aldosterone system and vitamin D-FGF-23-klotho in chronic kidney disease. J Am Soc Nephrol. 2011;22:1603–9. https://doi.org/10.1681/ASN.2010121251.
Mancia G, De Backer G, Dominiczak A, et al. The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013. https://doi.org/10.1093/eurheartj/eht151.
Ermolenko VM, Volgina GV, Dobronravov VA, et al. National recommendations on mineral and bone disorders in chronic kidney disease. Russian Dialysis Society (May 2010).Nephrologia I Dialis. 2011;13(1):33–51.
Garneata L, Stancu A, Dragomir D, Stefan G, Mircescu G. Ketoanalogue-supplemented vegetarian very low–protein diet and CKD progression. J Am Soc Nephrol. 2016;27(7):2164–76. https://doi.org/10.1681/ASN.2015040369.
Kovesdy RCM,AS-F, Kalantar-Zadeh CP. K. Low-protein diet for conservative management of chronic kidney disease: a systematic review and meta-analysis of controlled trials. J Cachexia Sarcopenia Muscle. 2018;9(2):235–45. https://doi.org/10.1002/jcsm.12264.
Milovanova LY, Mukhin NA, Kozlovskaya LV, Milovanov YS, Kiyakbaev GG, Rogova IV, et al. Decreased serum levels of klotho protein in chronic kidney disease patients: clinical importance. Vestn Ross Akad Meditsinskikh Nauk. 2016;71:288–96. https://doi.org/10.15690/vramn581.
Neyra JA, Hu MC. Potential application of klotho in human chronic kidney disease. Bone. 2017. https://doi.org/10.1016/j.bone.2017.01.017.
Xie J, Cha S-K, An S-W, Kuro-o M, Birnbaumer L, Huang C-L. Cardioprotection by Klotho through downregulation of TRPC6 channels in the mouse heart. Nat Commun. 2012;3:1238. https://doi.org/10.1038/ncomms2240.
NasrAllah MM, El-Shehaby AR, Osman NA, Fayad T, Nassef A, Salem MM, et al. The association between fibroblast growth factor-23 and vascular calcification is mitigated by inflammation markers. Nephron Extra. 2013;3(1):106–12. https://doi.org/10.1159/000356118.
Steitz SA, Speer MY, Curinga G, Yang H-Y, Haynes P, Aebersold R, et al. Smooth muscle cell phenotypic transition associated with calcification: upregulation of Cbfa1 and downregulation of smooth muscle lineage markers. Circ Res. 2001;89:1147–54.
Zhou D, Tan RJ, Fu H, Liu Y. Wnt/[beta]-catenin signaling in kidney injury and repair: a double-edged sword. Lab Invest. 2016;96:156–67. https://doi.org/10.1038/labinvest.2015.153.
Fang Y, Ginsberg C, Seifert M, Agapova O, Sugatani T, Register TC, et al. CKD-induced wingless/integration1 inhibitors and phosphorus cause the CKD-mineral and bone disorder. J Am Soc Nephrol. 2014;25:1760–73. https://doi.org/10.1681/ASN.2013080818.
Acknowledgements
This work was supported by the Russian Science Foundation (Grant No. 14-15-00947 2014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Institutional Review Board of the Sechenov First Moscow State Medical University (Protocol No. 06–14, 16.06.2014). All the patients provided written informed consent. All the described procedures were performed in accordance with the Helsinki Declaration.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Milovanova, L., Fomin, V., Moiseev, S. et al. Effect of essential amino acid кetoanalogues and protein restriction diet on morphogenetic proteins (FGF-23 and Кlotho) in 3b–4 stages chronic кidney disease patients: a randomized pilot study. Clin Exp Nephrol 22, 1351–1359 (2018). https://doi.org/10.1007/s10157-018-1591-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1591-1