Abstract
Background
In dialysis patients, mortality risk due to cardiovascular diseases is remarkably high and prognosis is poor; coronary artery calcification is considered one of the major contributing factors. It is known that hyperphosphatemia is associated with coronary artery calcification. Therefore, controlling serum phosphate level and thereby mitigating vascular calcification could improve the poor prognosis of dialysis patients. However, the optimal phosphate level in dialysis patients remains unknown; hence, this study was planned to compare the effects of two types of non-calcium-based phosphate binders, and examine the effect of strict control of phosphate on coronary artery calcification.
Methods
EPISODE is a randomized, open-label, multi-center, interventional trial with a two-by-two factorial design (UMIN ID: UMIN000023648). This trial will enroll hemodialysis patients who have been on dialysis for at least 3 months with a pre-dialysis serum phosphate level of at least 5.0 mg/dL or at least 6.1 mg/dL, respectively, in those taking or not taking a phosphate binder, as measured during the observation period. Registered patients will be randomized to the sucroferric oxyhydroxide or lanthanum carbonate arm and will receive the assigned drug to reduce serum phosphate to two target levels (3.5–4.5 mg/dL in strict arm and 5.0–6.0 mg/dL in standard arm) for 12 months. The primary endpoint will be percent change in coronary artery calcification score, and the secondary endpoints will include change from baseline serum phosphate and calcium levels, change in renal anemia-related factors, etc. The desired sample size has been calculated to be 200 patients.
Similar content being viewed by others
Introduction and rationale
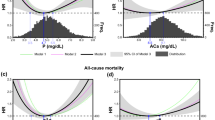
Dialysis patients have poor prognosis and very high mortality risk due to cardiovascular diseases (CVD) such as ischemic heart disease, cerebrovascular disorder, and heart failure. Coronary artery calcification is considered a major contributor to CVD, and the involvement of hyperphosphatemia in coronary artery calcification is widely known. Studies in stable dialysis patients showed that the addition of one calcified area in the vessel will increase the risk of all-cause mortality 1.9-fold and the risk of cardiovascular mortality 2.6-fold [1]. Furthermore, it was reported that the relative risk of mortality in dialysis patients increased when serum phosphate level was over 5.0 mg/dL; likewise, higher serum calcium level was associated with higher relative risk of mortality in hemodialysis patients [2]. Treatment with phosphorus binders was associated with decreased mortality compared with no treatment in the intention-to-treat, as-treated, and matched analyses [3]. Non-calcium-based phosphate binders, including lanthanum carbonate, were found to be more effective in attenuating coronary artery calcification than calcium-based phosphate binders [4,5,6]. Therefore, non-calcium-based phosphate binders could improve the prognosis of dialysis patients by attenuating vascular calcification. Sucroferric oxyhydroxide, a novel non-calcium-based phosphate binder, also has a potent serum phosphate-lowering effect; thus, the treatment with this drug is expected to improve the prognosis of dialysis patients [7, 8]. However, no reports have compared the effect of lanthanum carbonate with that of sucroferric oxyhydroxide on coronary artery calcification in chronic dialysis patients, who are at high risk of coronary artery calcification. Therefore, we planned a study to compare the effects of these two types of non-calcium-based phosphate binders on coronary artery calcification. Furthermore, it is also very important to determine whether strictly controlling serum phosphate level will lead to further decrease in the risk of coronary artery calcification in dialysis patients, although lowering serum phosphate level is closely associated with coronary artery calcification. In support of these goals, we will conduct a randomized trial using a two-by-two factorial design which allows comprehensive investigation of the effects of both factors—type of drug (lanthanum carbonate versus sucroferric oxyhydroxide) and different phosphate target level (standard treatment versus strict treatment for serum phosphate level control)—on coronary artery calcification risk.
Study sample and procedures
Chronic maintenance hemodialysis patients with hyperphosphatemia who meet the inclusion criteria, but not the exclusion criteria in Table 1 will be enrolled in this trial. Registration will be conducted via a central registration method. The Electronic Data Capture (EDC) system (Forum PLUS®) will be used to register subjects and collect data via the internet. The investigators will obtain written consent from patients who meet the eligibility criteria during the observation period and enter the necessary information into the EDC system. Subjects will undergo multi-detector computed tomography (MDCT) scan at a designated medical institution specialized in MDCT testing as well as endocrine and special testing. Each participating medical institution will conduct observation period testing specified in the protocol, and enter and register necessary information into the EDC system. Randomization will be conducted via the EDC system at registration. Subjects will be switched to one of either of the two types of drugs according to the randomization result and receive the drug for 12 months to reduce serum phosphate to the target level. Subjects will undergo specified laboratory tests and other procedures during specified visits. Subjects will undergo MDCT scan at a medical institution specialized in MDCT testing as well as endocrine and special testing in the 12th month of the treatment period. The trial is being conducted under the Helsinki Declaration, and was approved by the Institutional Review Board at Osaka University Graduate School of Medicine. All participants have been fully informed by the investigators and gave their informed consent.
Treatment intervention
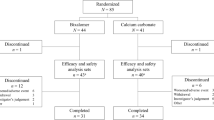
The randomization system in the EDC software platform will be used to allocate subjects as shown in Fig. 1 via the dynamic allocation method (minimization). During the 12-month treatment, individuals are randomly assigned in a 1:1 ration to receive sucroferric oxyhydroxide or lanthanum carbonate (Factor 1) to reduce serum phosphate to two target levels (3.5 mg/dL ≤ serum phosphate < 4.5 mg/dL in strict treatment arm and 5.0 mg/dL ≤ serum phosphate < 6.0 mg/dL in standard treatment arm; Factor 2). The investigators will check the drug allocated by the EDC system at registration and administer the drug per its prescription (dose and method of administration) for 12 months starting within 1 week of registration. Randomization will be controlled by three factors: age at consent (≥ 20 and ≤ 64 years old, ≥ 65 and ≤ 79 years old), CACS as measured during the observation period (≥ 30 and ≤ 400, ≥401 and ≤ 1000, ≥1001), and investigational site. The use of anti-hyperphosphatemia drugs other than sucroferric oxyhydroxide and lanthanum carbonate will be prohibited during the treatment period. However, when the target serum phosphate level is not reached, concomitant use of sevelamer hydrochloride and bixalomer will be allowed. Switching between different types of erythropoietin (EPO) formulations is not allowed during the treatment period. Investigational drug administration and testing will be performed according to Fig. 2. Observation and testing will be performed according to the schedule shown in Fig. 3.
Observation and testing schedule. Test items at the initiation of investigational treatment should be conducted within 1 week after the initiation of administration. The allowable window for observation and testing at months 3, 6, 9, and 12 is defined as the reference day ± 1 month (30 days). Filled circle: required item. Filled circle: sites which are capable of conducting endocrine and special testing.
End points
The primary end point is the percent change in CACS. Secondary end points are (1) changes in CACS, (2) changes in serum phosphate and calcium levels, changes in calcium phosphate product, and the ratio of patients who reached the target serum phosphate level, (3) changes in the level of intact parathyroid hormone (PTH), intact fibroblast growth factor (FGF)-23, and c-terminal FGF23, (4) effects on the renal anemia, assessed by transferrin saturation (TSAT), hemoglobin, and the changes in the dose of iron and EPO administration, (5) relationship between serum phosphate level and CACS, (6) average doses of phosphate binder required to achieve the target serum phosphate level, and (7) safety issue (adverse drug reactions). Imaging data scanned by MDCT with at least 16 rows will be submitted as electronic data in Digital Imaging and Communication in Medicine format via an electronic medium (either CD-R or DVD-R) to the MDCT committee. MDCT committee members will analyze the submitted imaging data and calculate CACS. The MDCT committee will discuss the validity of the calculated CACS, and determine the final CACS by consensus.
Target sample size
The target number of registered patients is 200 patients (50 patients per arm × 4 arms). Rationale for the sample size: our past research investigating the relationship between the average serum phosphate level and percent change in CACS at months 6, 12, and 18 after dialysis introduction in patients with a baseline CACS of 30 or higher (n = 64) showed that the median percent change in CACS was 20.3% for those with serum phosphate level ˂4.5 mg/dL (n = 18; mean serum phosphate level, 3.86 mg/dL) and 73.0% for those with serum phosphate level ≥ 5.0 mg/dL (n = 32; mean serum phosphate level, 5.81 mg/dL). The probability that an observation in the group with serum phosphate level < 4.5 mg/dL will be less than that in the group with serum phosphate level ≥ 5.0 mg/dL was estimated to be 0.77.
On the basis of the above results, the probability that percent change in CACS is lower in the strict treatment arm than in the standard treatment arm is conservatively estimated at 0.70; therefore, when a two-sided Wilcoxon rank sum test with a significance level of 2.5% is used, the required sample size will be 63 patients per arm to achieve a desired power of at least 95%. On the other hand, no previous research data are available to define the expected percent change in CACS for the lanthanum carbonate arm and sucroferric oxyhydroxide arm; thus, assuming a 0.675 probability that percent change in CACS is lower for the sucroferric oxyhydroxide arm than the lanthanum carbonate arm, the required sample size is 83 patients per arm to have at least 95% of power. Therefore, the larger sample size, 83 patients per arm (166 patients for both arms), will be the required sample size. Assuming that approximately 15% of all patients will be excluded from full analysis set, the target number of registered patients will be 100 patients per factor arm (a total of 200 patients).
Statistical analysis
Following the intention-to-treat principle, primary efficacy analyses will be conducted in the full analysis set and secondary analyses using the ‘per protocol set’ will be conducted only for the primary endpoint. Safety analysis will be conducted in all registered patients who have taken the investigational drug. The primary analysis objective of this study is to investigate the superiority of sucroferric oxyhydroxide to lanthanum carbonate, or strict treatment to standard treatment, in terms of the primary end point CACS. The significance level used for the tests will be 0.05 (two-sided) and missing data will not be imputed.
The following will be calculated per arm: the number of registered patients and number of analyzed patients for each analysis set, the appropriate summary statistics for patient characteristics and baseline data, and the appropriate summary statistics for administration duration and total dose of each investigational drug, discontinuation or not, reasons for discontinuation if any, etc. Cases excluded from the analysis set will be summarized by reason for exclusion. Percent change in CACS during the observation period (months 1–12) will be evaluated by arm, or factor. As for the primary analysis, the Wilcoxon rank sum test will be used to test null hypotheses that the percent change in CACS is equivalent between factors, or arms. In the primary analysis, a two-sided significance level of 2.5% will be used in testing to limit the overall study-wise type I error rate to no more than 5%. Sub-group analyses will be conducted by age at the time of consent acquisition, CACS as measured during the observation period, gender, and status of phosphate binder use during the observation period. As for the secondary end points, a linear mixed model will be used to compare serum phosphate and calcium levels, and change in calcium-phosphate product between arms, while the Chi-square test will be used to compare the proportion of patients who have achieved the target serum phosphate level between arms. Wilcoxon rank sum test will be used to compare changes of intact PTH, intact FGF23, and c-terminal FGF23 between arms. Other investigations will include comparison of the impact on nephrogenic anemia, relationship between serum phosphate level and CACS, and comparison of the average doses required to achieve the target serum phosphate level. As for safety, the total number of adverse events and number of individual adverse events will be calculated by arm, and serious adverse events will be tabulated.
Discussion
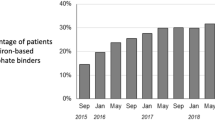
Hyperphosphatemia is an important condition that determines survival and prognosis of hemodialysis patients, with medications such as phosphate binders as well as dialysis and dietary interventions playing central roles in its treatment. The evolution of phosphate binders started with the era of aluminum-based products in the 1970s–1980s, and calcium-based products emerged in the 1990s. However, calcium-based products have drawbacks including inadequate phosphate-lowering effect and association with hypercalcemia. This has led to the development of novel anti-hyperphosphatemia drugs not containing calcium, or non-calcium-based products, such as sevelamer hydrochloride and lanthanum carbonate in the past decade [9,10,11]. Another drug in the non-calcium-based phosphate binder category, sucroferric oxyhydroxide, was launched in 2015. Because it dramatically lowered serum phosphate level, it soon became a new option in clinical practice [12]. In addition, this drug enabled strict control of phosphate. Sucroferric oxyhydroxide, as well as lanthanum carbonate, was also shown to have an FGF23 reduction effect and vascular calcification progression-suppressive effect in adenine-induced corticotropin-releasing hormone rats [13]; however, its effect on vascular calcification in humans remains unknown. Therefore, it would be highly desirable to conduct this clinical study of sucroferric oxyhydroxide aiming at evaluating percent change in CACS, as the primary end point, and compare it with lanthanum carbonate (another non-calcium-based product with a phosphate-binding effect).
References
Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension (Dallas: 1979) 2001;38:938–42.
Taniguchi M, Fukagawa M, Fujii N, Hamano T, Shoji T, Yokoyama K, Nakai S, Shigematsu T, Iseki K, Tsubakihara Y. Serum phosphate and calcium should be primarily and consistently controlled in prevalent hemodialysis patients. Therapeutic apheresis and dialysis: official peer-reviewed journal of the International Society for Apheresis, the Japanese Society for Apheresis. Jpn Soc Dial Therapy. 2013;17:221–8.
Isakova T, Gutierrez OM, Chang Y, Shah A, Tamez H, Smith K, Thadhani R, Wolf M. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol: JASN. 2009;20:388–96.
Kalil RS, Flanigan M, Stanford W, Haynes WG. Dissociation between progression of coronary artery calcification and endothelial function in hemodialysis patients: a prospective pilot study. Clin Nephrol. 2012;78:1–9.
Ohtake T, Kobayashi S, Oka M, Furuya R, Iwagami M, Tsutsumi D, Mochida Y, Maesato K, Ishioka K, Moriya H, Hidaka S. Lanthanum carbonate delays progression of coronary artery calcification compared with calcium-based phosphate binders in patients on hemodialysis: a pilot study. J Cardiovasc Pharmacol Ther. 2013;18:439–46.
Toussaint ND, Lau KK, Polkinghorne KR, Kerr PG. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in haemodialysis: a pilot randomized controlled trial. Nephrology (Carlton Vic). 2011;16:290–8.
Floege J, Covic AC, Ketteler M, Mann JF, Rastogi A, Spinowitz B, Chong EM, Gaillard S, Lisk LJ, Sprague SM. Long-term effects of the iron-based phosphate binder, sucroferric oxyhydroxide, in dialysis patients. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association. Eur Renal Assoc. 2015;30:1037–46.
Hergesell O, Ritz E. Stabilized polynuclear iron hydroxide is an efficient oral phosphate binder in uraemic patients. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association. Eur Renal Assoc. 1999;14:863–7.
Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–52.
Hutchison AJ, Barnett ME, Krause R, Kwan JT, Siami GA. Long-term efficacy and safety profile of lanthanum carbonate: results for up to 6 years of treatment. Nephron Clin Pract. 2008;110:c15-23.
Hutchison AJ, Maes B, Vanwalleghem J, Asmus G, Mohamed E, Schmieder R, Backs W, Jamar R, Vosskuhler A. Efficacy, tolerability, and safety of lanthanum carbonate in hyperphosphatemia: a 6-month, randomized, comparative trial versus calcium carbonate. Nephron Clin Pract. 2005;100:c8-19.
Floege J, Covic AC, Ketteler M, Rastogi A, Chong EM, Gaillard S, Lisk LJ, Sprague SM. A phase III study of the efficacy and safety of a novel iron-based phosphate binder in dialysis patients. Kidney Int. 2014;86:638–47.
Phan O, Maillard M, Peregaux C, Mordasini D, Stehle JC, Funk F, Burnier M. PA21, a new iron-based noncalcium phosphate binder, prevents vascular calcification in chronic renal failure rats. J Pharmacol Exp Ther. 2013;346:281–9.
Acknowledgements
The authors would like to thank the Japan Academic Research Forum which coordinated this study and KISSEI PHARMACEUTICAL CO., LTD. for financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y.I. & Y.T. received lecture fee and fees for the chairperson from Kissei Pharmaceutical Co.Ltd. and Bayer Yakuhin Ltd. T.H, received lecture fee from Kissei Pharmaceutical Co.Ltd. and Bayer Yakuhin Ltd. H.F. received lecture fees and grants from Kissei Pharmaceutical Co.Ltd. and Bayer Yakuhin Ltd. S.T. received research grants from Kissei Pharmaceutical Co.Ltd. None of the data presented has been published in whole or in part.
Ethical approval
All procedures performed in studies involving human participants will be in accordance with the ethical standards of the Osaka University Hospital clinical research committee (IRB approval number: 16112-5) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Isaka, Y., Fujii, H., Tsujimoto, Y. et al. Rationale, design, and characteristics of a trial to evaluate the new phosphate iron-based binder sucroferric oxyhydroxide in dialysis patients with the goal of advancing the practice of E.B.M. (EPISODE). Clin Exp Nephrol 22, 967–972 (2018). https://doi.org/10.1007/s10157-018-1547-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1547-5