Abstract
Hinge craniotomy (HC) is a technique that allows for a degree of decompression whilst retaining the bone flap in situ, in a ‘floating’ or ‘hinged’ fashion. This provides expansion potential for ensuing cerebral oedema whilst obviating the need for cranioplasty in the future. The exact indications, technique and outcomes of this procedure have yet to be determined, but it is likely that HC provides an alternative technique to decompressive craniectomy (DC) in certain contexts. The primary objective was to collate and describe the current evidence base for HC, including perioperative parameters, functional outcomes and complications. The secondary objective was to identify current nomenclature, operative technique and operative decision-making. A scoping review was performed in accordance with the PRISMA-ScR Checklist. Fifteen studies totalling 283 patients (mean age 45.1 and M:F 199:46) were included. There were 12 different terms for HC. The survival rate of the cohort was 74.6% (n = 211). Nine patients (3.2%) required subsequent formal DC. Six studies compared HC to DC following traumatic brain injury (TBI) and stroke, finding at least equivalent control of intracranial pressure (ICP). These studies also reported reduced rates of complications, including infection, in HC compared to DC. We have described the current evidence base of HC. There is no evidence of substantially worse outcomes compared to DC, although no randomised trials were identified. Eventually, a randomised trial will be useful to determine if HC should be offered as first-line treatment when indicated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A recent study estimated 60% of global neurosurgical caseload is traumatic brain injury (TBI) and stroke (6.2 and 2.8 million, respectively)—the majority in low-to-middle-income settings [1]. There are significant societal costs associated with TBI due to high levels of mortality and morbidity. A rigorous evidence base to guide treatment strategies remains an international public health priority.
The literature describing decompressive craniectomy (DC) is varied [2]. Recent and ongoing randomised controlled trials (RCTs) for the use of DC in TBI (DECRA [3]; RESCUEicp [4]; RESCUE-ASDH) and stroke (DECIMAL [5]; DESTINY [6]; HAMLET [7]) though have demonstrated its potential utility and efficacy, they raise ongoing concerns, in some of the studies, regarding the higher rates of disability observed in survivors following DC. Regarding TBI, the DECRA trial showed that neuroprotective bifrontal DC for moderate intracranial hypertension (ICP) is not helpful, whereas the RESCUEicp trial found that last-tier DC for severe and refractory ICP can significantly reduce the mortality rate but is associated with a higher rate of disability [2,3,4]. In relation to ischaemic stroke, a Cochrane review [8] including data from all the three extant randomised controlled trials (DECIMAL [5]; DESTINY [6]; HAMLET [7]) suggested that DC improves survival compared with best medical management, but that an increased proportion of individuals treated with DC survive with moderately severe or severe disability [8, 9].
A relatively novel and less well-utilised technique to achieve cerebral decompression in patients with brain swelling and/or raised ICP is the ‘hinge craniotomy’ (HC), also known as hinged decompressive craniectomy. The technique was first described by three independent groups in 2007 [10,11,12] specifically for surgical modulation of post-traumatic medically intractable raised ICP, although it has been used by neurosurgeons for several years for sundry other indications. Adoption of HC into neurosurgical practice can potentially yield benefits over traditional DC in specific situations, such as the potential to control at least moderate cerebral oedema whilst simultaneously obviating the need for a subsequent costly operative cranioplasty [2]. This is a particularly important consideration in resource-limited settings. Furthermore, unlike for the traditional surgical technique of DC, following HC, there are reports of potential reduction in axonal stretching and there are supposedly fewer complications such as syndrome of the trephined, problems with CSF hydrodynamics, infection and resorption of the autologous bone flap [13].
However, HC has possible limitations; these revolve mainly around whether sufficient extracranial brain expansion volume will be achieved and whether the patient will require the more traditional DC later on. Central to the HC vs DC debate is not just about post-operative patient survival, but the subsequent functional outcome and associated morbidity that may be incurred. There is a paucity of rigorous data evaluating HC, and contemporary evidence is based upon experience from small series in single centres from disparate regions of the world.
Our primary objective in this study was to collate, assess and describe the current evidence base for the use of HC. We assess the current indications, differing techniques, functional outcomes and complications of the procedure. To this end, we performed a scoping review; a relatively novel study design that determines the scope or coverage of a body of literature on a given topic and gives a broad overview [14, 15]. This review process is particularly useful for examining the emerging evidence relating to HC whilst it still remains relatively unclear what other, more specific questions can be posed and valuably addressed by a more precise systematic review and meta-analysis [14, 16]. This is important as there is variation in the definition and technique of HC as currently described by diverse workers interested in it from different regions of the world. Moreover, the exact indication for HC is unclear, for, although it may have a role between medical management and DC in both TBI and stroke, little robust evidence presently exists for it. A scoping review provides the perfect medium to report on the current evidence surrounding HC, using systematic methodology provided by the recently published PRISMA-ScR framework [17].
Methods
Protocol and registration
This scoping review has been reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) [17]. Unlike systematic reviews, the protocol does not need to be registered with PROSPERO [15].
Eligibility criteria
The following advanced search strategy was used to search all PubMed on 22 June 2019:
((((((((craniotomy[Title/Abstract]) OR craniectomy[Title/Abstract]) OR decompress*[Title/Abstract])) AND ((((((hinge*[Title/Abstract]) OR float*[Title/Abstract]) OR in situ[Title/Abstract]) OR riding[Title/Abstract]) OR osteoplastic[Title/Abstract]) OR anchored[Title/Abstract]))) NOT “case reports”[Publication Type]))
Titles and abstracts were screened for relevance. Full-text articles were then assessed for eligibility according to the PICOS criteria below. The reference lists of eligible studies and relevant articles were searched for further studies not identified by the initial search strategy. Manuscripts were excluded if data was not available separately for the HC cohort; they were case reports; or were paediatric series.
PICOS criteria
-
Population: Diagnosis of TBI or stroke and exposure to HC
-
Intervention: Hinge craniotomy; in situ hinge craniectomy; the Tucci flap; in situ resin floating cranioplasty; in situ free floating craniectomy; osteoplastic decompression; hinge decompressive craniotomy temporalis; riding craniotomy; modified temporal muscle hinge decompressive craniotomy; floating anchored craniotomy
-
Comparison: Studies with and without controls were included due to nature of scoping review
-
Outcomes and other data collected: Demographics, description of indications and surgical techniques, intracranial pressure monitoring, mean length of stay, functional outcome, mortality
-
Study design: All prospective and retrospective case series, cohort studies, case-control and randomised controlled trials with n > 1 written in English were included
Selection of sources of evidence
The resulting titles and abstracts were screened independently by two authors (HLH and MM) using the PICOS criteria above. If disagreements occurred, a third author (AK) was consulted. Data extraction was performed independently by the same two authors with disagreements resolved via further review and discussion. Due to the heterogeneity of terminology used for hinge craniotomy in the global literature, whenever a new term was identified from the references, it was incorporated into the search strategy.
Data charting process
The data extraction process in a scoping review is known as ‘data charting’. Key variables were screened and extracted from the papers. These data were inputted into a Microsoft Excel Document, which was the basis of the data charting form. This was continuously updated in an iterative process, as heterogeneity of data and reported outcomes meant often non-contiguous data points. However, if the data was important and remained an essential component to report on in this paper, it was added to the charting process. Two reviewers independently (HLH & MM) charted data from each eligible article. Any disagreements were resolved through discussion between the two reviewers or further adjudication by a third reviewer (AK).
Data items
Indication for hinge craniotomy: age, sex and indication for hinge craniotomy. If there were multiple pathologies, for example subdural haematoma and intracerebral haemorrhage following TBI, then the first pathology was listed as the indication. For some of the studies, separate male:female ratio of HC cohort was not stated; therefore, the male:female ratio reported in Results is less than the total number of patients.
Surgical technique and nomenclature: the named procedure was recorded, with size of craniotomy, dural manipulation, hinge craniotomy practice and the placement of wound drain.
Perioperative parameters: pre- and post-operative variables (ICP, GCS, midline shift and CT-Rotterdam criteria) were recorded.
Clinical outcomes: survival, Glasgow Outcome Scale (GOS) and modified Rankin Score (mRS) and follow-up were recorded. The GOS is reported as favourable (GOS 4–5) and unfavourable (GOS 1–3). The mRS is reported as: ‘Good’ = 0–2; ‘Moderate’ = 3–4; and ‘Poor’ = 5–6.
Complications: inadequate cerebral decompression was reported if the bone flap needed to be removed subsequently due to refractory intracranial hypertension. Infection, need for reoperation and other complications were also recorded.
Comparison between HC and DC: studies that compared the two techniques were summarised.
Level of evidence: data was also extracted on article demographics (journal, institution, level of evidence, summary of article) and the income status of the country of origin.
Synthesis of results
The results in this manuscript are presented as a scoping review, including summary tables, and follow the following format: (1) indication for hinge craniotomy; (2) surgical technique and nomenclature; (3) perioperative parameters; (4) functional outcomes; (5) complications; (6) summary of comparison studies and (7) level of evidence.
Results
Indication and patient demographics
A total of 15 studies [10,11,12,13, 18,19,20,21,22,23,24,25,26,27,28] were eligible for inclusion (Fig. 1), comprising 283 patients with a mean age 45.1 years and a male:female of 199:46 (Table 1). The majority of patients (n = 230, 81.3%) underwent HC following TBI. Of the patients who suffered TBI, the most common pathology was acute subdural haematoma (n = 182, 79.1%), followed by intracerebral haemorrhage (n = 33, 14.3%) and epidural haematoma (n = 7, 3.0%). A number of patients (n = 53, 18.7%) underwent HC following stroke: haemorrhagic (n = 40, 75.5%) and ischaemic (n = 13, n = 24.5%).
Surgical technique and nomenclature
There were 12 separate terms used to describe hinge craniotomy, of which hinge craniotomy was the most common (n = 4, 33.3%). Every other term was used once (Table 2).
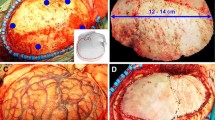
The ‘hinge’ was achieved via a variety of techniques (Table 2). Most commonly, the free bone flap was secured with miniplates. To achieve this, the inferior edge of the bone flap was re-secured to the inferior cranial edge with a straight titanium plate. The 5- or 6-millimetre screw on the inferior cranial edge protruded 1 to 1.5 mm above the plate to allow flap movement. A similar plate was screwed flush onto the superior edge of the bone flap. The distal end of the straight plate was not screwed to the nearby cranium thereby remaining unattached, and thus creating a hinge; this permitting portion of the flap to float on its hinge outward with brain swelling [11] whilst simultaneously reducing the risk of a sinking bone flap. Some of the groups fastened the upper initially unsecured screws several months later to secure the bone flap. Another technique used loosely tied sutures attached to the free bone [13] flap or a resin mould of the skull implanted [18]. This promoted symmetrical room for expansion if the brain was to swell, whilst the hinge technique provides only unilateral, and therefore asymmetrical, expansion potential. To increase expansion potential, the inner table of the free bone flap can be thinned. A separate technique, known as osteoplastic decompression [21], which has recently been adapted to the modified temporalis muscle hinge decompressive craniectomy [26], utilised the temporalis muscle as an anchor for the free bone flap which was partially secured using sutures in the anterior and posterior vertical cuts. Four reports using these techniques included the use of a subgaleal wound drain at wound closure.
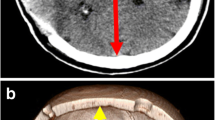
Perioperative parameters
The majority of patients undergoing HC were comatose (GCS < 9), with abnormal CT findings (significant midline shift and Rotterdam score) (Table 3). Pre-operative ICP values were sparse. Hinge craniotomy resulted in reduced ICP, a reduction in midline shift and also improved Rotterdam scores (Table 3). The GCS was not reported as a post-operative outcome. Specifically, of the studies that had pre-operative ICP recorded, patients undergoing HC demonstrated a reduced ICP post-operatively. Patients in the Guttman et al. [13] series had pre-operative ICP of 32.7 ± 8.1 mmHg compared to 16.0 ± 12.1 mmHg post-operatively. In Valenca et al. [20], the pre-operative ICP range was 15–35 mmHg and 6–12 mmHg post-operatively.
Direct comparison of HC to DC in relation to perioperative variables was limited (Table 6). Kenning et al. [19] demonstrated that ICP control at post-operative day 5 was adequate and equivalent (HC 12.1 ± 2.6 mmHg; DC 15.0 ± 6.3 mmHg), despite the smaller volume of expansion (HC 77.5 ± 54.1 ml; DC 105.1 ± 65.1 ml). The imaging in 15 of the patients revealed reversal of midline shift (MLS) pre- and post-operatively (HC post-op MLS 6.4 ± 4.4 mm; DC 5.5 ± 4.6 mm), although this difference was not statistically significant [19]. Furthermore, the MLS in patients receiving HC was also reduced. Peethambaran et al. [28] demonstrated a MLS of 13.1 ± 4.78 mm reduced to 6.6 ± 3.9 mm post-operatively, whilst Schmidt et al. [11] 10.6 to 5.1 mm following HC.
The same group 3 years later demonstrated no statistically significant difference in post-operative ICP control for the duration of monitoring (HC 10.8 ± 3.4 mmHg; DC 11.9 ± 3.5 mmHg) [24], in addition to a similar finding of a smaller expansion volume (HC 77.6 ± 44.7 ml; DC 96.3 ± 54.4 ml) [24]. Furthermore, Tsermoulas et al. [25] compared DC to ‘riding craniotomy’ (HC from hereon) in ASDH, demonstrating the post-operative intracranial hypertension index was not worse than DC (HC 13.8; DC 16.6), in a patient cohort with similar baseline characteristics.
Clinical outcomes
Two hundred and eighty-three patients underwent HC, of which 211 survived (74.6%). There was a paucity of data reported relating to functional outcome and duration of follow-up (Table 4).
Comparing survival outcomes of HC to DC, Kenning et al. [19] found no significant difference between hospital survival (HC n = 15, 75%; DC n = 21, 70%), whilst their second study investigating HC in stroke management found that hospital survival was significantly higher in the DC group (HC n = 5, 56%; DC n = 17, 89%, p = 0.04) [24] (Table 6). However, they also found that despite the higher in-hospital mortality, HC was associated with better long-term functional outcome, as determined by mRS scores at the 30–90 day period (HC 2.8 ± 1.1; DC 4.4 ± 0.9, p = 0.01) and at the 90- to 180-day period (HC 2.5 ± 0.6; DC 3.9 ± 1.0, p = 0.03) [24]. A study from India [28] also demonstrated that both DC and ‘four-quadrant osteoplastic decompressive craniotomy’ (hinge craniotomy in this case) were comparable in relation to the duration of surgery, duration of ICU stay and survival (p > 0.05). Furthermore, there was significant brain expansion potential and reversal of MLS. Tsermoulas et al. [25] also found that more patients in the DC group had poor functional status at 6 months compared with the HC group at 6 months (HC n = 6, 35%; DC n = 41, 59%). On the contrary, Kano et al. [23] compared DC with hinge craniotomy following TBI or stroke and found no significant difference in the long-term functional outcome, as measured by post-operative GOS and mRS. There were variable lengths of follow-up, if at all stated. Nine studies explicitly stated the length of follow-up, which ranged from 2 to 18 months. Furthermore, not all studies recorded functional outcome status at the end of follow-up, merely just that the patient was seen by healthcare practitioners in the time period. Six studies did not state duration of follow-up.
Complications
There were 54 reported complications in the HC cohort (Table 5). Nine patients (n = 9/283, 3.2%) required subsequent decompressive craniectomy due to uncontrollable ICP, or in other words, ‘failure’ of hinge craniotomy. In one study [23], the bone flap was removed in 2 cases due to acute hydrocephalus or brain herniation causing low cerebral perfusion pressure and in the other 2 cases, ICP was elevated immediately secondary to CT-confirmed epidural haemotoma requiring progression to DC. In another study [24], one patient was placed in a barbiturate-induced coma at the request of the treating neurologist, although the paper states that ICP was in normal range.
Regarding the replaced free bone flap specifically, there were 2 incidences of malfunctioning technique requiring removal of the bone flap [22] and two incidences of bone flap depression [26] utilising the temporalis HC technique. One patient required reoperation to secure the bone flap due to increased mobility [19]. There was no reported syndrome of the trephined or other complications uniquely associated with decompressive craniectomy. In the reported studies, one patient, who underwent HC with a resin implant, requested subsequent cranioplasty for cosmetic reasons [18]. The remaining patients receiving HC group had satisfactory cosmetic outcomes. Ko et al. [10] refastened the hinge in 8 patients during the proceeding post-operative months, using local anaesthetic. Two patients refused this and subsequently died within the 8 months of follow-up.
Kenning et al. [19, 24] found that there was no significant difference between HC and DC in terms of operative time, need for reoperation, duration of mechanical ventilation or ICU stay. Their analysis revealed a greater degree (not statistically significant) of post-operative parenchymal contusion enlargement with DC, which may reflect blossoming of the contusions secondary to unconstrained brain expansion [19]. Furthermore, Kenning et al. reported only one patient undergoing HC requiring subsequent cranioplasty compared to 17 patients who received DC (HC 1/5, 20%; DC 17/17, 100%) [24].
Kano et al. [23] report no bone flap infections in HC whilst there were 6 of such in DC after autologous cranioplasty (p = 0.02). The earliest of the six cases of bone flap infection in DC occurred 1 week after the cranioplasty, and the latest case occurred more than 4 months after cranioplasty (mean, 4.1 weeks). Additionally, we extracted data of the complications from the DC groups of the controlled studies. There were 15 infections (8.7%) in the DC group versus 12 infections (4.2%) in the HC (p = 0.065, Fisher’s).
Level of evidence
The level of evidence for the majority of the HC literature was poor, according to the University of Oxford’s Centre for Evidence-based Medicine Levels of Evidence [29]. There was 1 level V study [12] (6.7%), 8 level IV studies [10, 11, 13, 18, 20,21,22, 26] (53.3%) and 6 level III studies [19, 22, 24, 25, 27, 28] (40.0%). Twelve studies were retrospective in nature. Five studies [10,11,12, 19, 24] were from the USA, the most common origin of study. Four studies were from LMIC countries [22, 26,27,28]—India and Nigeria. The remaining 11 studies were in developed healthcare settings.
Discussion
This review highlights the heterogeneity of nomenclature as well as the technical variations in the operative procedure of HC as currently reported in the global literature. Nonetheless, the evidence base, still limited though, regarding its indications and effectiveness suggests that HC may have a role to play in the treatment of TBI and/or stroke, obviating secondary complications usually associated with decompressive craniectomy, as well as the cost and complications of the consequent cranioplasty.
Nomenclature and technique
Since being described by three groups in 2007 [10,11,12], HC has 12 different terms to our knowledge. The most common term was ‘hinge craniotomy’ (Table 2). Despite heterogenous techniques and nomenclature, the general principles appear unanimous: partial decompression to relieve raised intracranial pressure with subsequent immediate replacement of the bone flap, over the surgical cranial window, in a ‘loose’ or ‘hinged’ fashion in an attempt to accommodate cerebral oedema and subsequent swelling, without further neurosurgical intervention. This principal attempts to reduce complications such as infection, syndrome of the trephined, hydrodynamic disturbances and secondary cranioplasty whilst maintaining adequate cerebral decompression.
We believe that from hereon, it would be useful to agree and adhere to one umbrella term (e.g. decompressive craniotomy), and this can be used to describe all variations of this technique. Nevertheless, the following questions (Fig. 2) remain open to the neurosurgical community.
Efficacy of hinge craniotomy
Intracranial pressure
Hinge craniotomy was reported to be effective at controlling ICP. All studies that reported post-operative readings demonstrated a decrease in ICP and associated reduction in midline shift (Table 3). The studies comparing HC to DC suggest that HC is at least as effective as DC in this respect (Table 6). Kano et al. [23] compared HC with DC in TBI and stroke, and summarising their data, averred ‘the hinge technique with ICP monitoring was effective and safe for the management for head trauma and stroke’. Furthermore, Kenning et al. [19, 24] suggested that ‘hinge craniotomy was at least as good as decompressive craniectomy in providing post-operative ICP control’. Furthermore, out of 283 patients undergoing HC, only 9 patients (3.2%) required subsequent DC, suggesting that adequate cerebral decompression was achieved by HC alone. In the RESCUEicp trial, which enrolled patients with severe TBI and ICP raised and refractory to medical management, of the patients who were randomised and received a DC (n = 187), 12 required a barbiturate infusion post-DC due to ongoing issues with ICP control (6.4%). Obviously, the patients included in the studies of the present scoping review are not directly comparable to the RESCUEicp population but this figure can give an indication as to the proportion of patients with refractory ICP despite DC.
This concept is further reinforced by a biomechanical study in human cadaver skulls [30], which compared DC to HC and ‘dynamic decompressive craniotomy’ and the effect on ICP after abrupt increase in intracranial volume. They found that both the dynamic craniotomy and the HC techniques provided significant control of ICP during 120 ml increase in intracranial volume as compared with craniotomy rigidly fixed with plates (4.86 mmHg, 8.36 mmHg, 44.84 mmHg, respectively).
Clinical and functional outcomes
Central to the clinical management of raised ICP in TBI or stroke is the patient’s quality of life after receiving treatment for the injury. This was highlighted in the recent RESCUEicp trial [4] which demonstrated that more patients with refractory ICP (> 25 mmHg) who underwent decompressive craniectomy had decreased mortality but increased disability when compared with medical therapy alone. In RESCUEicp [4], the survival of the DC patients at 6 months was 73.1%. The overall survival of patients undergoing HC was 74.6% (n = 211) (Table 4) and thus very similar to the RESCUEicp mortality, although it is important to appreciate that RESCUEicp was looking at secondary DC. The studies included in this manuscript had limited long-term functional outcome reported (Tables 4 and 6). Furthermore, the presence of extracranial injuries or injuries of different severity makes direct summary of outcomes difficult. Lastly, as the evidence informing treatment strategies in TBI is developing, morbidity outcome post-surgical intervention is key and thus central to optimal intervention.
Complications
The standard procedure of DC is associated with several complications, including syndrome of the trephined, subdural hygromas/effusions, contusion/haematoma progression, incisional cerebrospinal fluid leak and hydrocephalus. In contrast, HC might provide a means to reduce these complications, particularly obviating the need for subsequent costly cranioplasty, further hospital admission and likely prolonged ITU stay. Nevertheless, one quite significant complication of the latter to consider is the possibility of ‘failure’ of HC to provide adequate ICP control and therefore progression to DC, of which there were 6 cases in this review (Table 5). Otherwise, the data presented in this study suggest that HC is associated with a trend towards reduced infection and complications described above (Table 5). Due to the retrospective nature of the vast majority of studies, underreporting of complications may be a potential issue and obviously due to the lack of randomisation, differences in the baseline characteristics could be responsible for the observed trends.
Hinge craniotomy in low-to-middle-income settings
Perhaps one of the most interesting facets to this review is the emerging practice during HC of using the temporalis muscle, without any other costly biomaterial implant, as an anchor for the bone flap in low-to-middle-income settings. Adeleye et al. [22, 26] report on this technique (Table 2), as well as a low-cost duraplasty, and using a unitized tube-and-reservoir urine drainage system, the Uri-bag, as a wound drain to significantly reduce the cost of TBI treatment. Obviating the need for cranioplasty further reduces costs and logistical issues. This is particularly relevant as the LMIC have the majority of TBI burden, with the least resources, facilities and trained neurosurgeons [1, 31]. Therefore, hinge craniotomy provides potential clinical utility, in addition to economic benefits, further reinforcing the need for a more substantial evidence base relating to its use in these settings.
Novel devices
Central to developing this field of neurosurgery are innovative devices to facilitate surgical theory. Two devices, the ‘Skull Flap’ (SF) [32] and the ‘expandable dynamic craniotomy bone flap fixation plate’ [33], provide biomechanical evidence of utility in controlling ICP by providing adequate volume expansion whilst preventing sinking of the bone flap. Furthermore, the devices are durable, low-cost and easy to use.
The SF [32] is a hinge system comprised with plate and sliding track that carries a locking-unlocking system, connected to a titanium wire tunnelled and externalised in the scalp. This wire serves as traction for repositioning of the flap back to its anatomical position once cerebral oedema has subsided, permitting bony fusion of the flap edges.
Another recent manuscript explores the biomechanics of a ‘novel expandable dynamic craniotomy bone flap fixation plate’ [33]. The dynamic plate comprises solid ends with holes for placement of screws into the bone flap at one end and the skull at the other end. The solid portions are connected with a configuration of flat interconnections that function similarly to a spring that reversibly expands and contracts as well as angulates, depending upon the tension exerted. The plates allow outward bone flap movement to accommodate an increase in ICP and/or intracranial volume and retract the bone flap in a flush position once the ICP normalizes. The group evaluated the plates characteristics in human cadaver skulls and demonstrated significant increase in intracranial volume expansion due to compliance of the bone flap in comparison to a rigid or hinged bone flap. In essence, the reversibly expandable, MRI/CT-compatible plates provide for a low-profile bone flap fixation with rigid restriction of bone flap sinking and also enable cranial decompression with a high tolerance for repetitive expansion and contraction.
Cost-effectiveness
An important aspect to consider especially for low- and middle-income countries is if HC is actually cost-effective or at least cost neutral compared to DC. Unfortunately, raw cost data was not available in the included studies. However, DC is thought to be an expensive procedure with a mean patient cost of over US$ 20,000 when performed in a developing country [34]. HC is potentially a cheaper alternative due to autologous tissues being utilised and reducing the need for a second operation for a cranioplasty [26]. A formal cost-effectiveness analysis evaluating the many different factors that influence cost needs to be undertaken, which is one of the future aims of our neurotrauma study group at the University of Cambridge.
Limitations of the present study
The lack of robust comparative HC vs DC data, the combined indications (TBI and stroke) for HC in some of the reports, heterogenous pre-operative and radiological metrics, paucity of pre-operative ICP monitoring, short-term follow-up and poor reporting of long-term functional outcomes makes absolute conclusion difficult. Furthermore, GOS recorded at discharge is not necessarily a true representative of long-term outcomes, and the paucity of robust follow-up investigating associated morbidity, a key metric, in most reports is also of note. Additionally, mRS is the most commonly used outcome scale in the field of stroke but many of the included studies used the GOS to assess outcomes in the TBI but also stroke patients. The two scales examine slightly different aspects of functional outcome but the Glasgow Outcome Scale correlates well with the mRS in patients with stroke [35].
Developing the evidence base
To continue developing the evidence base for HC, we would advocate following the IDEAL Methodology [36]. This is a 5-stage description of the surgical development process, a crucial tool for systematic evaluation of surgical innovation and that is instrumental for achieving improved design, conduct and reporting of surgical research. Currently, HC is between stage IIb and III ‘Exploration’ and ‘Assessment’, i.e. the technique is stable, has been replicated by numerous study groups and there is some literature demonstrating comparison to existing practice (DC).
It must be appreciated that HC cannot, as yet, be considered an alternative to all the DCs, but rather an alternative to primary DC, not to secondary DC. Whereas HC has been performed most often for persistent brain swelling after evacuation of intracranial hematoma, DC has been performed most often as a part of second- or third-tier therapy as in DECRA [3] and RESCUEicp [4] trials for patients with medically refractory intracranial hypertension. In such cases, it is unlikely that a HC will be performed instead of DC.
To further develop HC, additional evaluation of the technique prospectively and co-operatively may help mature consensus over definition, quality and indications. Ultimately, an international effort, with a multi-centre randomised controlled trial, with participation from low- and middle-income countries is required. The trial could compare HC to DC with criteria for progression from HC to DC in selected cases. In addition, ICP monitoring, if already used clinically, would aid meaningful comparison. Importantly, such a study would aim to compare long-term functional outcomes and surgical morbidity (Table 7).
Conclusion
Hinge craniotomy has a potential role in the surgical management of TBI/stroke, yielding adequate cerebral decompression in the majority of reported cases, a reduction in complications and potentially offers substantial economic savings (both operative costs and the cost of living with significant morbidity). It is likely that HC offers an intermediate intervention between treatment-refractive medical therapy and traditional decompressive craniectomy. Future work should aim to facilitate a global consensus about HC and its utility as treatment, ultimately paving the way for a randomised controlled trial.
References
Dewan, M. C. et al. (2018) Estimating the global incidence of traumatic brain injury. J Neurosurg 1–18. https://doi.org/10.3171/2017.10.jns17352
Kolias AG et al (2018) The current status of decompressive craniectomy in traumatic brain injury. Curr Trauma Rep 4:326–332
Cooper JD et al (2011) Decompressive craniectomy in diffuse traumatic brain injury. New Engl J Med 364:1493–1502
Hutchinson PJ et al (2016) Trial of decompressive craniectomy for traumatic intracranial hypertension. New Engl J Med 375:1119–1130
Vahedi K et al (2007) Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke 38:2506–2517
Jüttler E et al (2007) Decompressive surgery for the treatment of malignant infarction of the middle cerebral artery (DESTINY). Stroke 38:2518–2525
Hofmeijer J et al (2009) Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol 8:326–333
Cruz-Flores S, Berge E, Whittle IR (2012) Surgical decompression for cerebral oedema in acute ischaemic stroke. Cochrane Db Syst Rev. https://doi.org/10.1002/14651858.cd003435.pub2
Kolias AG, Kirkpatrick PJ, Hutchinson PJ (2013) Decompressive craniectomy: past, present and future. Nat Rev Neurol 9:405
Ko K, Segan S (2007) In situ hinge craniectomy. Oper Neurosurg 60:ONS-255–ONS-259
Schmidt JH, Reyes BJ, Fischer R, Flaherty SK (2007) Use of hinge craniotomy for cerebral decompression. J Neurosurg 107:678–682
Goettler CE, Tucci KA (2007) Decreasing the morbidity of decompressive craniectomy: the Tucci Flap. J Trauma Acute Care 62:777
Gutman M, How E, Withers T (2017) The floating anchored craniotomy. Surg Neurol Int 8:130
Armstrong R, Hall BJ, Doyle J, Waters E (2011) ‘Scoping the scope’ of a cochrane review. J Public Health 33:147–150
Munn Z et al (2018) Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 18(143)
Munn Z, Stern C, Aromataris E, Lockwood C, Jordan Z (2018) What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol 18(5)
Tricco AC et al (2018) PRISMA extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. https://doi.org/10.7326/m18-0850
Ahn D-H, Kim D-W, Kang S-D (2009) In situ floating resin cranioplasty for cerebral decompression. J Korean Neurosurg S 46:417–420
Kenning TJ, Gandhi RH, German JW (2009) A comparison of hinge craniotomy and decompressive craniectomy for the treatment of malignant intracranial hypertension: early clinical and radiographic analysis. Neurosurg Focus 26:E6
Valença MM, Martins C, da Silva J (2010) “In-window” craniotomy and “bridgelike” duraplasty: an alternative to decompressive hemicraniectomy. J Neurosurg 113:982–989
Mracek J, Choc M, Mork J, Vacek P, Mracek Z (2011) Osteoplastic decompressive craniotomy—an alternative to decompressive craniectomy. Acta Neurochir 153:2259
Adeleye AO, Azeez A (2011) Decompressive craniectomy bone flap hinged on the temporalis muscle: a new inexpensive use for an old neurosurgical technique. Surg Neurol Int 2:150
Kano T, Kurosaki S, Wada H (2012) Retrospective analysis of hinge technique for head trauma or stroke. Neurol Med-Chir 52:816–821
Kenning TJ et al (2012) Cranial decompression for the treatment of malignant intracranial hypertension after ischemic cerebral infarction: decompressive craniectomy and hinge craniotomy. J Neurosurg 116:1289–1298
Tsermoulas G et al (2016) Surgery for acute subdural hematoma: replace or remove the bone flap? World Neurosurg 88:569–575
Adeleye AO (2016) Clinical and radiologic outcome of a less invasive, low-cost surgical technique of osteoplastic decompressive craniectomy. J Neurol Surg Part Central European Neurosurg 77:167–175
Mezue W, Ndubuisi C, Ohaegbulam S, Chikani M, Erechukwu U (2013) Cranial bony decompressions in the management of head injuries: decompressive craniotomy or craniectomy? Niger J Clin Pract 16:343–347
(2015) Four-quadrant osteoplastic decompressive craniotomy: a novel technique for refractory intracranial hypertension - A pilot study. Neurol India 63:895–902
(2009) Oxford Centre for Evidence-based Medicine – Levels of Evidence (March 2009)
Khanna R, Ferrara L (2016) Dynamic telescopic craniotomy: a cadaveric study of a novel device and technique. J Neurosurg 125:674–682
Dewan MC, et al. (2018) Global neurosurgery: the current capacity and deficit in the provision of essential neurosurgical care. Executive Summary of the Global Neurosurgery Initiative at the Program in Global Surgery and Social Change. J Neurosurg 1–10. https://doi.org/10.3171/2017.11.jns171500
Chibbaro S et al (2013) The ‘Skull Flap’ a new conceived device for decompressive craniectomy/cranioplasty: feasibility study on cadaver specimen. J Neurosci Rural Pract 4:283–287
Khanna R, Ferrara L, Khanna S (2019) Biomechanics of a novel reversibly expandable dynamic craniotomy bone flap fixation plate. J Neurosurg:1–8. https://doi.org/10.3171/2018.8.jns172614
Badke G et al (2018) Analysis of direct costs of decompressive craniectomy in victims of traumatic brain injury. Arq Neuropsiquiatr 76(4):257–264
Kasner SE (2006) Clinical interpretation and use of stroke scales. Lancet Neurol 5(7):603–612
McCulloch P et al (2009) No surgical innovation without evaluation: the IDEAL recommendations. Lancet 374:1105–1112
Acknowledgements
Many thanks to Dr Veronica Phillips, Medical Library, University of Cambridge for her assistance with the search strategy.
Funding
This research was commissioned by the National Institute for Health Research (NIHR) Global Health Research Group on Neurotrauma (16/137/105) using UK aid from the UK Government. Aswin Chari is supported by a Great Ormond Street Hospital (GOSH) Children’s Charity Surgeon Scientist Fellowship and the National Institute for Health Research GOSH Biomedical Research Centre. Peter Hutchinson is supported by a Research Professorship from the National Institute for Health Research (NIHR), the NIHR Cambridge Biomedical Research Centre, a European Union Seventh Framework Program grant (CENTER-TBI; grant no. 602150) and the Royal College of Surgeons of England. Angelos Kolias is supported by a Clinical Lectureship, School of Clinical Medicine, University of Cambridge.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Franco Servadei has received personal fees from Takeda Pharmaceutical Company, grants and personal fees from Integra LifeSciences and grants and personal fees from Finceramica SpA. The rest of the authors declare that they have no conflict of interest related to this manuscript.
Ethical approval
Ethical approval is not applicable for a scoping review.
Informed consent
Informed consent is not applicable for a scoping review.
Disclaimer
The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hugo Layard Horsfall and Midhun Mohan are joint first authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Layard Horsfall, H., Mohan, M., Devi, B.I. et al. Hinge/floating craniotomy as an alternative technique for cerebral decompression: a scoping review. Neurosurg Rev 43, 1493–1507 (2020). https://doi.org/10.1007/s10143-019-01180-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01180-7