Abstract
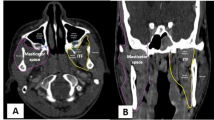
Meningiomas of the posterior fossa represent a heterogeneous group of tumors regarding difficulty of resection and functional outcome. The aim of this review was to focus on tumors located mainly on the posterior surface of the petrous bone and threatening hearing and facial functions. An anatomical classification was used to evaluate surgical outcome depending on the relationship of the tumor to the internal auditory meatus. The authors performed a retrospective chart review of 53 consecutive patients operated on for a posterior petrous bone meningioma in a tertiary referral center and a literature review. Tumors were classified in four groups according to the modified Desgeorges and Sterkers classification: posterior petrous (P; 17 tumors), meatus and internal auditory canal (M; 12 tumors), petrous apex without invasion of the internal auditory canal (A; 9 tumors), and cerebellopontine angle with invasion of the internal auditory canal (AMP; 15 tumors). The facial function was preserved in 100% of P and A tumors, 75% of group M tumors, and 53% of AMP tumors. Hearing preservation was attempted only in P, A, and M groups where rates of serviceable hearing preservation were 82%, 80%, and 66%, respectively. The cumulative rate of hearing preservation for AMP tumors was 45% in our literature review. The increased facial morbidity associated with AMP tumors compared with other groups was also confirmed by the review of the literature. In conclusion, this study shows that among posterior petrous bone meningiomas, tumors invading the internal auditory canal present with increased postoperative functional morbidity in spite of a tailored approach regarding dural insertion.

Similar content being viewed by others
References
Ausman JI (2006) A revolution in skull base surgery: the quality of life matters! Surg Neurol 65(6):635–636
Bacciu A, Piazza P, Di Lella F, Sanna M (2007) Intracanalicular meningioma: clinical features, radiologic findings, and surgical management. Otol Neurotol 28(3):391–399
Bassiouni H, Hunold A, Asgari S, Stolke D (2004) Meningiomas of the posterior petrous bone: functional outcome after microsurgery. J Neurosurg 100(6):1014–1024
Batra PS, Dutra JC, Wiet RJ (2002) Auditory and facial nerve function following surgery for cerebellopontine angle meningiomas. Arch Otolaryngol Head Neck Surg 128(4):369–374
Breuer T, Gjuric M, Wigand ME (2000) Extended middle fossa surgery for meningiomas within or at the internal auditory canal. Am J Otol 21(5):729–734
Bricolo AP, Turazzi S, Talacchi A, Cristofori L (1992) Microsurgical removal of petroclival meningiomas: a report of 33 patients. Neurosurgery 31(5):813–828, discussion 828
Castellano F, Ruggiero G (1953) Meningiomas of the posterior fossa. Acta Radiol 104:3–157
Anonymous (1995) Committee on hearing and equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). Otolaryngol Head Neck Surg 113:179–180
Couldwell WT, Fukushima T, Giannotta SL, Weiss MH (1996) Petroclival meningiomas: surgical experience in 109 cases. J Neurosurg 84(1):20–28
Darrouzet V, Guerin J, Aouad N, Dutkiewicz J, Blayney AW, Bebear JP (1997) The widened retrolabyrinthe approach: a new concept in acoustic neuroma surgery. J Neurosurg 86(5):812–821
Desgeorges M, Sterkers O (1994) Anatomo-radiological classification of meningioma of the posterior skull base. Neurochirurgie 40(5):273–295
Desgeorges M, Sterkers O, Poncet JL, Rey A, Sterkers JM (1995) Surgery for meningioma of the posterior skull base. 135 cases. Choice of approach and results. Neurochirurgie 41(4):265–290, discussion 290–264
Devèze A, Franco-Vidal V, Liguoro D, Guerin J, Darrouzet V (2007) Transpetrosal approaches for meningiomas of the posterior aspect of the petrous bone Results in 43 consecutive patients. Clin Neurol Neurosurg 109(7):578–588
House JW (1983) Facial nerve grading systems. Laryngoscope 93(8):1056–1069
Ichinose T, Goto T, Ishibashi K, Takami T, Ohata K (2010) The role of radical microsurgical resection in multimodal treatment for skull base meningioma. J Neurosurg 113(5):1072–1078
Kano T, Kawase T, Horiguchi T, Yoshida K (2010) Meningiomas of the ventral foramen magnum and lower clivus: factors influencing surgical morbidity, the extent of tumour resection, and tumour recurrence. Acta Neurochir (Wien) 152(1):79–86, discussion 86
Kawase T, Shiobara R, Ohira T, Toya S (1996) Developmental patterns and characteristic symptoms of petroclival meningiomas. Neurol Med Chir Tokyo 36(1):1–6
Kawase T, Shiobara R, Toya S (1991) Anterior transpetrosal-transtentorial approach for sphenopetroclival meningiomas: surgical method and results in 10 patients. Neurosurgery 28(6):869–875, discussion 875–866
Lang DA, Neil-Dwyer G, Garfield J (1999) Outcome after complex neurosurgery: the caregiver’s burden is forgotten. J Neurosurg 91(3):359–363
Lecuire J, Dechaume JP, Buffard P, Bochu M (1971) Meningiomas of the posterior cranial fossa. Neurochirurgie 17:1–146
Liu JK, Gottfried ON, Couldwell WT (2003) Surgical management of posterior petrous meningiomas. Neurosurg Focus 14(6):e7
Nakamura M, Roser F, Dormiani M, Matthies C, Vorkapic P, Samii M (2005) Facial and cochlear nerve function after surgery of cerebellopontine angle meningiomas. Neurosurgery 57(1):77–90, discussion 77–90
Nakamura M, Roser F, Mirzai S, Matthies C, Vorkapic P, Samii M (2004) Meningiomas of the internal auditory canal. Neurosurgery 55(1):119–127, discussion 127–118
Natarajan SK, Sekhar LN, Schessel D, Morita A (2007) Petroclival meningiomas: multimodality treatment and outcomes at long-term follow-up. Neurosurgery 60(6):965–979, discussion 979–981
Qu FJ, Zhou XD, Wang XL, Li F, Lu XD, Liu YG, Zhong YH, Yang HA, Ni SL (2009) The classification of posterior petrous meningiomas and its clinical significance. J Int Med Res 37(3):949–957
Raj Wijetunga LH, Fagan PA, Sheehy JP (1998) Petrous apex meningiomas: an alternative surgical approach. J Clin Neurosci 5(3):310–317
Roberti F, Sekhar LN, Kalavakonda C, Wright DC (2001) Posterior fossa meningiomas: surgical experience in 161 cases. Surg Neurol 56(1):8–20, discussion 20–21
Rosenorn J (1989) The risk of ischaemic brain damage during the use of self-retaining brain retractors. Acta Neurol Scand Suppl 120:1–30
Rosenorn J, Diemer NH (1982) Reduction of regional cerebral blood flow during brain retraction pressure in the rat. J Neurosurg 56(6):826–829
Roser F, Nakamura M, Dormiani M, Matthies C, Vorkapic P, Samii M (2005) Meningiomas of the cerebellopontine angle with extension into the internal auditory canal. J Neurosurg 102(1):17–23
Samii M, Tatagiba M (1992) Experience with 36 surgical cases of petroclival meningiomas. Acta Neurochir Wien 118(1–2):27–32
Sanna M, Bacciu A, Pasanisi E, Taibah A, Piazza P (2007) Posterior petrous face meningiomas: an algorithm for surgical management. Otol Neurotol 28(7):942–950
Schaller B, Merlo A, Gratzl O, Probst R (1999) Premeatal and retromeatal cerebellopontine angle meningioma. Two distinct clinical entities. Acta Neurochir Wien 141(5):465–471
Seifert V (2010) Clinical management of petroclival meningiomas and the eternal quest for preservation of quality of life: personal experiences over a period of 20years. Acta Neurochir (Wien) 152(7):1099–1116
Sekhar LN, Jannetta PJ (1984) Cerebellopontine angle meningiomas. Microsurgical excision and follow-up results. J Neurosurg 60(3):500–505
Sekhar LN, Jannetta PJ, Burkhart LE, Janosky JE (1990) Meningiomas involving the clivus: a six-year experience with 41 patients. Neurosurgery 27(5):764–781, discussion 781
Selesnick SH, Nguyen TD, Gutin PH, Lavyne MH (2001) Posterior petrous face meningiomas. Otolaryngol Head Neck Surg 124(4):408–413
Sughrue ME, Kane AJ, Shangari G, Rutkowski MJ, McDermott MW, Berger MS, Parsa AT (2010) The relevance of Simpson Grade I and II resection in modern neurosurgical treatment of World Health Organization Grade I meningiomas. J Neurosurg 113(5):1029–1035
von Eckardstein KL, Driscoll CLW, Link MJ (2010) Outcome after microsurgery for meningiomas involving the internal auditory canal. Neurosurgery 67(5):1236–1242
Voss NF, Vrionis FD, Heilman CB, Robertson JH (2000) Meningiomas of the cerebellopontine angle. Surg Neurol 53(5):439–446, discussion 446–437
Wu ZB, Yu CJ, Guan SS (2005) Posterior petrous meningiomas: 82 cases. J Neurosurg 102(2):284–289
Yasargil M, Mortara R, Curcic M (1980) Meningiomas of basal posterior cranial fossa. Adv Tech Stand Neurosurg 7:3–115
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Sunil Manjila, Nicholas C. Bambakidis, Cleveland, USA
We read with interest the clinical case series of 53 cases of posterior petrous meningiomas, with special attention to the facial nerve function and serviceable hearing loss; their surgical outcome is impressive at 35 months of mean follow-up. The established facts about these lesions are reassertained: more anterior lesions are less amenable to GTR, residual tumors are commonly left in the petrous apex/cave area, subtotal resections are reserved for debilitated patients and poor brainstem interface, and cumbersome hearing and facial nerve preservation with advanced tumors. It is noted that the authors have used transpetrous approaches in majority of the patients (57%) compared with the common workhorse approach—retrosigmoid suboccipital approach. We agree with the use of these approaches in selected circumstances, though we feel that acceptable Simpson grades of resection can be achieved using a standard retrosigmoid approach. We reserve use of combined transpetrosal approaches in cases in which tumors are located entirely medial to the internal acoustic meatus and span both the posterior and middle cranial fossae. In most of such cases, we attempt to preserve hearing unless it has been preoperatively compromised or if tumor size dictates that a greater degree of exposure is required.
Andreas Raabe, Bern, Switzerland
In this interesting paper, the authors classify the risk of surgery of posterior petrosal tumors according to their location in respect to the internal auditory canal. Their series is large and the classification makes sense, however, it is not surprising. In our institution, we do not always consider tumors of the posterior petrous bone to threaten the VII/VIII nerve but only those in contact with the internal auditory canal. This is confirmed by the functional results of this study with a 100% preservation rate for the facial nerve in the petrous apex and posterior petrous tumors. Tumors of the internal auditory canal and CPA-meningiomas with invasion of the internal auditory canal had less favorable facial nerve preservations of 75% and 53%. As expected, the results of hearing preservation are less favorable but show a similar risk distribution. Interestingly, the authors used predominantly transpetrous approaches, contrary to our practice of using retrosigmoid approach for most cases. This may be explained by the fact that we do not follow the rule of the authors to always attack a meningioma from the site of dural attachment. This is certainly the best approach in terms of interrupting the blood supply and complete tumor resection but not necessarily for a multimodal treatment concept focusing on preservation of the facial and hearing nerve. Subtotal resection can also be the surgical goal for tumors invading the internal auditory canal followed by radiosurgical treatment. I would just repeat one of the key statements of the article: “In an era of multimodal treatment, gross-total resection is not mandatory to achieve functional preservation and good tumor control.” The authors should be congratulated for their study, techniques, and outcomes.
Rights and permissions
About this article
Cite this article
Peyre, M., Bozorg-Grayeli, A., Rey, A. et al. Posterior petrous bone meningiomas: surgical experience in 53 patients and literature review. Neurosurg Rev 35, 53–66 (2012). https://doi.org/10.1007/s10143-011-0333-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0333-6