Abstract
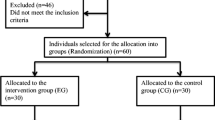
The objective of this research was to compare the effect single low-level laser therapy (LLLT) irradiation on pain perception in patients having fixed appliance treatment in the clinic of orthodontics. Sixty-two patients were recruited to participate in this randomized, double-blinded, placebo-controlled study. The patients were assigned to four groups: group I—laser on the right side; group II—placebo on the right side; group III—laser on the left side; group IV—placebo on the left. The laser or placebo was applied before separation, 24 and 48 h after separation of their first permanent molars in the lower arch. Just after the separation, the average of the pain for the placebo group was 1.6, significantly greater than the average of 1.1 registered for the laser group (p = 0.013). After 24 h and before the new irradiation, the values registered among the different groups did not show any differences. In relation to the gender, only after the first irradiation in placebo group, the female had a level of pain (0.1) significantly higher (p = 0.04) compared to male, and after 48 h, the group where the laser was applied had a difference (p = 0.04) among the gender with a value of lower pain for men (0.6) than for women (1.6).
The laser irradiation to minimize the pain was only effective when applied immediately after treatment and separation. In general way, there were no differences between the genders, except after the first placebo group irradiation in which the female had a significantly higher level of pain compared to male and after 48 h. The pain cycle observed in this study had its peak in 24 h, both for laser’s and placebo’s group.


Similar content being viewed by others
References
Ngan P, Kess B, Wilson S (1989) Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofac Orthop 96(1):47–53
Scheurer PA, Firestone AR, Burgin WB (1996) Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod 18(4):349–357
Jones M, Chan C (1992) The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofac Orthop 102(4):373–381
Bergius M, Berggren U, Kiliaridis S (2002) Experience of pain during an orthodontic procedure. Eur J Oral Sci 110(2):92–98
Erdinc AM, Dincer B (2004) Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod 26(1):79–85
Polat O, Karaman AI (2005) Pain control during fixed orthodontic appliance therapy. Angle Orthod 75(2):214–219. https://doi.org/10.1043/0003-3219(2005)075<0210:PCDFOA>2.0.CO;2
Oliver RG, Knapman YM (1985) Attitudes to orthodontic treatment. Br J Orthod 12(4):179–188
Haynes S (1974) Discontinuation of orthodontic treatment relative to patient age. J Dent 2(4):138–142
Brown DF, Moerenhout RG (1991) The pain experience and psychological adjustment to orthodontic treatment of preadolescents, adolescents, and adults. Am J Orthod Dentofac Orthop 100(4):349–356. https://doi.org/10.1016/0889-5406(91)70073-6
Yamasaki K, Shibata Y, Imai S, Tani Y, Shibasaki Y, Fukuhara T (1984) Clinical application of prostaglandin E1 (PGE1) upon orthodontic tooth movement. Am J Orthod 85(6):508–518
Roth PM, Thrash WJ (1986) Effect of transcutaneous electrical nerve stimulation for controlling pain associated with orthodontic tooth movement. Am J Orthod Dentofac Orthop 90(2):132–138
Kehoe MJ, Cohen SM, Zarrinnia K, Cowan A (1996) The effect of acetaminophen, ibuprofen, and misoprostol on prostaglandin E2 synthesis and the degree and rate of orthodontic tooth movement. Angle Orthod 66(5):339–349. https://doi.org/10.1043/0003-3219(1996)066<0339:TEOAIA>2.3.CO;2
Bergius M, Kiliaridis S, Berggren U (2000) Pain in orthodontics. A review and discussion of the literature. J Orofac Orthop 61(2):125–137
Steen Law SL, Southard KA, Law AS, Logan HL, Jakobsen JR (2000) An evaluation of preoperative ibuprofen for treatment of pain associated with orthodontic separator placement. Am J Orthod Dentofac Orthop 118(6):629–635. https://doi.org/10.1067/mod.2000.110638
Kluemper GT, Hiser DG, Rayens MK, Jay MJ (2002) Efficacy of a wax containing benzocaine in the relief of oral mucosal pain caused by orthodontic appliances. Am J Orthod Dentofac Orthop 122(4):359–365
Polat O, Karaman AI, Durmus E (2005) Effects of preoperative ibuprofen and naproxen sodium on orthodontic pain. Angle Orthod 75(5):791–796. https://doi.org/10.1043/0003-3219(2005)75[791:EOPIAN]2.0.CO;2
Young AN, Taylor RW, Taylor SE, Linnebur SA, Buschang PH (2006) Evaluation of preemptive valdecoxib therapy on initial archwire placement discomfort in adults. Angle Orthod 76(2):251–259. https://doi.org/10.1043/0003-3219(2006)076[0251:EOPVTO]2.0.CO;2
Bradley RL, Ellis PE, Thomas P, Bellis H, Ireland AJ, Sandy JR (2007) A randomized clinical trial comparing the efficacy of ibuprofen and paracetamol in the control of orthodontic pain. Am J Orthod Dentofac Orthop 132(4):511–517. https://doi.org/10.1016/j.ajodo.2006.12.009
Lim HM, Lew KK, Tay DK (1995) A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofac Orthop 108(6):614–622
Topolski F, Moro A, Correr GM, Schimim SC (2018) Optimal management of orthodontic pain. J Pain Res 11:589–598. https://doi.org/10.2147/JPR.S127945
Deana NF, Zaror C, Sandoval P, Alves N (2017) Effectiveness of low-level laser therapy in reducing orthodontic pain: a systematic review and meta-analysis. Pain Res Manag 2017:8560652. https://doi.org/10.1155/2017/8560652
Cetiner S, Kahraman SA, Yucetas S (2006) Evaluation of low-level laser therapy in the treatment of temporomandibular disorders. Photomed Laser Surg 24(5):637–641. https://doi.org/10.1089/pho.2006.24.637
Sun G, Tuner J (2004) Low-level laser therapy in dentistry. Dent Clin N Am 48 (4):1061–1076, viii. doi:https://doi.org/10.1016/j.cden.2004.05.004
Farsaii A, Al-Jewair T (2017) Insufficient evidence supports the use of low-level laser therapy to accelerate tooth movement, prevent orthodontic relapse, and modulate acute pain during orthodontic treatment. J Evid Based Dent Pract 17(3):262–264. https://doi.org/10.1016/j.jebdp.2017.06.008
Turhani D, Scheriau M, Kapral D, Benesch T, Jonke E, Bantleon HP (2006) Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am J Orthod Dentofac Orthop 130(3):371–377. https://doi.org/10.1016/j.ajodo.2005.04.036
Fujiyama K, Deguchi T, Murakami T, Fujii A, Kushima K, Takano-Yamamoto T (2008) Clinical effect of CO(2) laser in reducing pain in orthodontics. Angle Orthod 78(2):299–303. https://doi.org/10.2319/033007-153.1
Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M (2008) The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci 23(1):27–33. https://doi.org/10.1007/s10103-007-0449-7
Tortamano A, Lenzi DC, Haddad AC, Bottino MC, Dominguez GC, Vigorito JW (2009) Low-level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. Am J Orthod Dentofac Orthop 136(5):662–667. https://doi.org/10.1016/j.ajodo.2008.06.028
Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofac Orthop 141(3):289–297. https://doi.org/10.1016/j.ajodo.2011.09.009
Harazaki M, Isshiki Y (1997) Soft laser irradiation effects on pain reduction in orthodontic treatment. Bull Tokyo Dent Coll 38(4):291–295
Harazaki M, Takahashi H, Ito A, Isshiki Y (1998) Soft laser irradiation induced pain reduction in orthodontic treatment. Bull Tokyo Dent Coll 39(2):95–101
Ren C, McGrath C, Yang Y (2015) The effectiveness of low-level diode laser therapy on orthodontic pain management: a systematic review and meta-analysis. Lasers Med Sci 30(7):1881–1893. https://doi.org/10.1007/s10103-015-1743-4
Sonesson M, De Geer E, Subraian J, Petren S (2016) Efficacy of low-level laser therapy in accelerating tooth movement, preventing relapse and managing acute pain during orthodontic treatment in humans: a systematic review. BMC Oral Health 17(1):11. https://doi.org/10.1186/s12903-016-0242-8
Sousa MV, Pinzan A, Consolaro A, Henriques JF, de Freitas MR (2014) Systematic literature review: influence of low-level laser on orthodontic movement and pain control in humans. Photomed Laser Surg 32(11):592–599. https://doi.org/10.1089/pho.2014.3789
Li FJ, Zhang JY, Zeng XT, Guo Y (2015) Low-level laser therapy for orthodontic pain: a systematic review. Lasers Med Sci 30(6):1789–1803. https://doi.org/10.1007/s10103-014-1661-x
Role of funding source
This study was funded by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Protocol 23/10 FOAr/UNESP
Rights and permissions
About this article
Cite this article
Martins, I.P., Martins, R.P., Caldas, S.G.F.R. et al. Low-level laser therapy (830 nm) on orthodontic pain: blinded randomized clinical trial. Lasers Med Sci 34, 281–286 (2019). https://doi.org/10.1007/s10103-018-2583-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-018-2583-9