Abstract
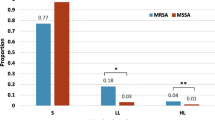
The emergence of methicillin-resistant staphylococci necessitated the search for alternative agents as linezolid, introduced to treat infections due to multidrug-resistant bacteria. Linezolid resistance has since emerged, yet its global prevalence remains low. In Egypt, little is known about the situation. We investigated the prevalence and mechanisms of resistance among Egyptian staphylococcal clinical isolates. Linezolid resistance among 232 staphylococcal isolates obtained from Alexandria Main Hospitals between 2011 and 2016 was assessed using disc diffusion and minimum inhibitory concentration. Resistant isolates were checked for cfr presence using polymerase chain reaction. The V domain of different alleles of 23S rRNA gene was investigated for mutations. Selection for linezolid-resistant mutants was performed in vitro through serial passages in linezolid sub-inhibitory concentrations. Combinations of linezolid with imipenem or anti-inflammatory agents were investigated using time-kill and modified checkerboard assays. Three Staphylococcus haemolyticus isolates (1.3%) from 2015 to 2016 were linezolid-resistant. One isolate carried cfr which was plasmid-borne, and together with another isolate which had a G2603T point mutation in the V domain of 23S rRNA gene. Successive exposure to linezolid sub-inhibitory concentrations was selected for three resistant Staphylococcus aureus mutants out of ten susceptible isolates. These mutants were more resistant towards different antibiotic classes than their susceptible parents. Linezolid combinations with imipenem, ibuprofen, or aspirin were synergistic against the isolates and mutants. Despite unregulated use of linezolid, resistance remains fairly low among the Egyptian isolates. Strict antimicrobial stewardship guidelines are needed in hospitals and the community to guard against further evolution of resistant mutants.


Similar content being viewed by others
Data availability
All raw data are available from the corresponding author upon reasonable request.
References
Davies J, Davies D (2010) Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev 74(3):417–433
Moghnieh RA, Kanafani ZA, Tabaja HZ, Sharara SL, Awad LS, Kanj SS (2018) Epidemiology of common resistant bacterial pathogens in the countries of the Arab League. Lancet Infect Dis 18(12):e379–e394. https://doi.org/10.1016/S1473-3099(18)30414-6
Ager S, Gould K (2012) Clinical update on linezolid in the treatment of Gram-positive bacterial infections. Infect Drug Resist 5:87–102
Moellering RC (2003) Linezolid: the first oxazolidinone antimicrobial. Ann Intern Med 138(2):135–142
Cidral TA, Carvalho MC, Figueiredo AM, de Melo MC (2015) Emergence of methicillin-resistant coagulase-negative staphylococci resistant to linezolid with rRNA gene C2190T and G2603T mutations. Apmis 123(10):867–871. https://doi.org/10.1111/apm.12426
Meka VG, Gold HS (2004) Antimicrobial resistance to linezolid. Clin Infect Dis 39(7):1010–1015
Long KS, Vester B (2012) Resistance to linezolid caused by modifications at its binding site on the ribosome. Antimicrob Agents Chemother 56(2):603–612
Musumeci R, Calaresu E, Gerosa J, Oggioni D, Bramati S, Morelli P, Mura I, Piana A, Are BM, Cocuzza CE (2016) Resistance to linezolid in Staphylococcus spp. clinical isolates associated with ribosomal binding site modifications: novel mutation in domain V of 23S rRNA. New Microbiol 39(4):269–273
Stefani S, Bongiorno D, Mongelli G, Campanile F (2010) Linezolid resistance in staphylococci. Pharmaceuticals (Basel, Switzerland) 3(7):1988–2006
Locke JB, Hilgers M, Shaw KJ (2009) Novel ribosomal mutations in Staphylococcus aureus strains identified through selection with the oxazolidinones linezolid and torezolid (TR-700). Antimicrob Agents Chemother 53(12):5265–5274
Toh SM, Xiong L, Arias CA, Villegas MV, Lolans K, Quinn J, Mankin AS (2007) Acquisition of a natural resistance gene renders a clinical strain of methicillin-resistant Staphylococcus aureus resistant to the synthetic antibiotic linezolid. Mol Microbiol 64(6):1506–1514
Hutchinson DK (2003) Oxazolidinone antibacterial agents: a critical review. Curr Top Med Chem 3(9):1021–1042
Tsiodras S, Gold HS, Sakoulas G, Eliopoulos GM, Wennersten C, Venkataraman L, Moellering RC, Ferraro MJ (2001) Linezolid resistance in a clinical isolate of Staphylococcus aureus. Lancet (London, England) 358(9277):207–208. https://doi.org/10.1016/s0140-6736(01)05410-1
Flamm RK, Mendes RE, Hogan PA, Streit JM, Ross JE, Jones RN (2016) Linezolid surveillance results for the United States (LEADER Surveillance Program 2014). Antimicrob Agents Chemother 60(4):2273–2280
Mendes RE, Deshpande L, Streit JM, Sader HS, Castanheira M, Hogan PA, Flamm RK (2018) ZAAPS programme results for 2016: an activity and spectrum analysis of linezolid using clinical isolates from medical centres in 42 countries. J Antimicrob Chemother 73(7):1880–1887
Abouelfetouh A (2017) The status of methicillin resistance among Egyptian Staphylococcus aureus isolates: an overview. Infect Disord Drug Targets 17(1):67–69
Azzab MM, El-Sokkary RH, Tawfeek MM, Gebriel MG (2017) Multidrug-resistant bacteria among patients with ventilatorassociated pneumonia in an emergency intensive care unit, Egypt. East Mediterr Health J 22(12):894–903
Hashem AA, Abd El Fadeal NM, Shehata AS (2017) In vitro activities of vancomycin and linezolid against biofilm-producing methicillin-resistant staphylococci species isolated from catheter-related bloodstream infections from an Egyptian tertiary hospital. J Med Microbiol 66(6):744–752. https://doi.org/10.1099/jmm.0.000490
Ashour HM, el-Sharif A (2007) Microbial spectrum and antibiotic susceptibility profile of gram-positive aerobic bacteria isolated from cancer patients. J Clin Oncol 25(36):5763–5769
ElSayed N, Ashour M, Amine AEK (2018) Vancomycin resistance among Staphylococcus aureus isolates in a rural setting, Egypt. Germs 8(3):134–139. https://doi.org/10.18683/germs.2018.1140
CLSI (2020) Clinical and Laboratory Standards Institute. 2020. Performance standards for antimicrobial susceptibility testing: 30th informational supplement M100-ED30. Wayne, PA
Kateete DP, Kimani CN, Katabazi FA, Okeng A, Okee MS, Nanteza A, Joloba ML, Najjuka FC (2010) Identification of Staphylococcus aureus: DNase and mannitol salt agar improve the efficiency of the tube coagulase test. Ann Clin Microbiol Antimicrob 9:23
Boerlin P, Kuhnert P, Hussy D, Schaellibaum M (2003) Methods for identification of Staphylococcus aureus isolates in cases of bovine mastitis. J Clin Microbiol 41(2):767–771
Ince D, Zhang X, Hooper DC (2003) Activity of and resistance to moxifloxacin in Staphylococcus aureus. Antimicrob Agents Chemother 47(4):1410–1415
Sambrook J, Fritsch EF, Maniatis T (1989) Molecular cloning: a laboratory manual, 2nd edn. Cold Spring Harbor Laboratory Press, Cold Spring Harbor
Kehrenberg C, Schwarz S (2006) Distribution of florfenicol resistance genes fexA and cfr among chloramphenicol-resistant Staphylococcus isolates. Antimicrob Agents Chemother 50(4):1156–1163. https://doi.org/10.1128/aac.50.4.1156-1163.2006
Letchumanan V, Chan KG, Lee LH (2015) An insight of traditional plasmid curing in Vibrio species. Front Microbiol 6:735
Pillai SK, Sakoulas G, Wennersten C, Eliopoulos GM, Moellering RC Jr, Ferraro MJ, Gold HS (2002) Linezolid resistance in Staphylococcus aureus: characterization and stability of resistant phenotype. J Infect Dis 186(11):1603–1607. https://doi.org/10.1086/345368
Singh SR, Bacon AE 3rd, Young DC, Couch KA (2009) In vitro 24-hour time-kill studies of vancomycin and linezolid in combination versus methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 53(10):4495–4497
Orhan G, Bayram A, Zer Y, Balci I (2005) Synergy tests by E test and checkerboard methods of antimicrobial combinations against Brucella melitensis. J Clin Microbiol 43(1):140–143
Biedenbach DJ, Moet GJ, Jones RN (2004) Occurrence and antimicrobial resistance pattern comparisons among bloodstream infection isolates from the SENTRY Antimicrobial Surveillance Program (1997-2002). Diagn Microbiol Infect Dis 50(1):59–69
Layer F, Vourli S, Karavasilis V, Strommenger B, Dafopoulou K, Tsakris A, Werner G, Pournaras S (2018) Dissemination of linezolid-dependent, linezolid-resistant Staphylococcus epidermidis clinical isolates belonging to CC5 in German hospitals. J Antimicrob Chemother 73(5):1181–1184
Morales G, Picazo JJ, Baos E, Candel FJ, Arribi A, Pelaez B, Andrade R, de la Torre MA, Fereres J, Sanchez-Garcia M (2010) Resistance to linezolid is mediated by the cfr gene in the first report of an outbreak of linezolid-resistant Staphylococcus aureus. Clin Infect Dis 50(6):821–825
LaMarre J, Mendes RE, Szal T, Schwarz S, Jones RN, Mankin AS (2013) The genetic environment of the cfr gene and the presence of other mechanisms account for the very high linezolid resistance of Staphylococcus epidermidis isolate 426-3147L. Antimicrob Agents Chemother 57(3):1173–1179
Chamon RC, Iorio NL, Cavalcante FS, Teodoro CR, de Oliveira AP, Maia F, dos Santos KR (2014) Linezolid-resistant Staphylococcus haemolyticus and Staphylococcus hominis: single and double mutations at the domain V of 23S rRNA among isolates from a Rio de Janeiro hospital. Diagn Microbiol Infect Dis 80(4):307–310
Arias CA, Vallejo M, Reyes J, Panesso D, Moreno J, Castaneda E, Villegas MV, Murray BE, Quinn JP (2008) Clinical and microbiological aspects of linezolid resistance mediated by the cfr gene encoding a 23S rRNA methyltransferase. J Clin Microbiol 46(3):892–896
Zhou W, Niu D, Cao X, Ning M, Zhang Z, Shen H, Zhang K (2015) Clonal dissemination of linezolid-resistant Staphylococcus capitis with G2603T mutation in domain V of the 23S rRNA and the cfr gene at a tertiary care hospital in China. BMC Infect Dis 15:97
Rio-Marques L, Hartke A, Bizzini A (2014) The effect of inoculum size on selection of in vitro resistance to vancomycin, daptomycin, and linezolid in methicillin-resistant Staphylococcus aureus. Microb Drug Resist (Larchmont NY) 20(6):539–543
Sweeney MT, Zurenko GE (2003) In vitro activities of linezolid combined with other antimicrobial agents against Staphylococci, Enterococci, Pneumococci, and selected gram-negative organisms. Antimicrob Agents Chemother 47(6):1902–1906
Yehia H, El Said M, Azmy M, Badawy M, Mansy S, Gohar H, Madany N (2016) Effect of linezolid alone and in combination with other antibiotics, on methicillin-resistant Staphylococcus aureus. J Egypt Soc Parasitol 46(1):57–66
Godon N, Denizot S, Podevin G, Caillon J, Potel G, Christophe Roze J, Gras-Le Guen C (2006) Effectiveness of linezolid and imipenem association in the treatment of severe community-acquired pneumonia in children: two case reports. Scand J Infect Dis 38(5):381–383
Zimmermann P, Curtis N (2017) Antimicrobial effects of antipyretics. Antimicrob Agents Chemother 61(4):e02268-16. https://doi.org/10.1128/AAC.02268-16
Acknowledgements
The authors would like to thank Dr. Marwa Naguib, Dr. Eva Adel, and Dr. Mustafa Alseqely for their help in isolate collection and PD Dr. med. Wilma Ziebuhr, Prof. Andrew Whitelaw Dr. Revathi Gunturu for their helpful insights.
Funding
This work was supported by the Academic Thesis Research Fund (ATRF), Faculty of Pharmacy, Alexandria University and DFG grant ZI665/3-1.
Author information
Authors and Affiliations
Contributions
Lina Maarouf carried out the experimental part of the study, including data analysis, and participated in manuscript writing. Hoda Omar followed up the performance of the experiments, analysis of the data, and manuscript writing. Moustafa El-Nakeeb designed the study and followed the progress of the work and writing of the manuscript. Alaa Abouelfetouh designed the study, participated in data analysis, and manuscript writing. All authors approved of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics statement
No human subjects or animals were involved so approval was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maarouf, L., Omar, H., El-Nakeeb, M. et al. Prevalence and mechanisms of linezolid resistance among staphylococcal clinical isolates from Egypt. Eur J Clin Microbiol Infect Dis 40, 815–823 (2021). https://doi.org/10.1007/s10096-020-04045-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-04045-w