Abstract
Background
Sexual dysfunction (SD) is a common, yet under-reported, non-motor symptom (NMS) of Parkinson’s disease (PD). The present study investigated the sexual functions in PD male patients, its correlation with motor and other NMSs, and their impact on health-related quality of life (HRQoL).
Methods
The sexual functions of 40 PD male patients were assessed using the International Index of Erectile Function (IIEF) and compared to 25 healthy age-matched controls. Patients were evaluated using the NMS Scale (NMSS) and the Arabic version of the Parkinson’s-Disease Questionnaire (PDQ-39). We compared the sexual functions of younger (≤ 55 years) and elder (> 55 years) males and tested the correlations between sexual functions and motor, other NMSs, and HRQoL.
Results
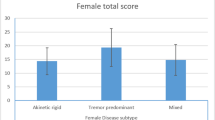
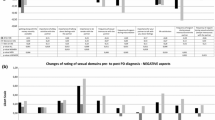
Seventy percent of PD male patients reported erectile dysfunction. They showed significantly worse total (p < 0.001) and subscores of IIEF, compared to healthy controls. The total IIEF was inversely correlated to age of patients (p = 0.013), age at onset (p = 0.043), total, cognitive/mood, gastrointestinal and urinary domains of NMSS, and the cognitive domain of PDQ-39 (p = 0.013). Age was the main predictor (ß = − 0.581, p = 0.006) of SD. Elder patients showed worse sexual functions, stronger correlations to other NMSs, and more impact on HRQoL than younger patients.
Conclusion
Sexual functions are worse among PD male patients with age as the main predictor. SD was associated with worse cognitive/mood and urinary domains of NMSS and has a negative impact on the patients’ HRQoL among elder males.
Similar content being viewed by others
Abbreviations
- ADL:
-
activities of daily living
- EF:
-
erectile function
- HRQoL:
-
health-related quality of life
- IIEF:
-
International Index of Erectile Function
- IS:
-
intercourse satisfaction
- NMSS:
-
Non-Motor Symptoms Scale
- OF:
-
orgasmic function
- OS:
-
overall satisfaction
- PD:
-
Parkinson’s disease
- PDQ-39:
-
39-item Parkinson’s Disease Questionnaire
- UPDRS:
-
Unified Parkinson’s Disease Rating Scale
References
Poewe W et al (2017) Parkinson disease. Nat Rev Dis Primers 3:17013
Chaudhuri KR, Sauerbier A, Rojo JM, Sethi K, Schapira AH, Brown RG, Antonini A, Stocchi F, Odin P, Bhattacharya K, Tsuboi Y, Abe K, Rizos A, Rodriguez-Blazquez C, Martinez-Martin P (2015) The burden of non-motor symptoms in Parkinson’s disease using a self-completed non-motor questionnaire: a simple grading system. Parkinsonism Relat Disord 21(3):287–291
Shalash AS et al (2018) Non-motor symptoms as predictors of quality of life in Egyptian patients with Parkinson’s disease: a cross-sectional study using a culturally adapted 39-item Parkinson’s Disease Questionnaire. Front Neurol 9:357
Ozcan T et al (2015) The relation of sexual dysfunction to depression and anxiety in patients with Parkinson’s disease. Acta Neuropsychiatr 27(1):33–37
Ferrucci R, Panzeri M, Ronconi L, Ardolino G, Cogiamanian F, Barbieri S, Barone P, Bertolasi L, Padovani A, Priori A (2016) Abnormal sexuality in Parkinson’s disease: fact or fancy? J Neurol Sci 369:5–10
Bronner G, Royter V, Korczyn AD, Giladi N (2004) Sexual dysfunction in Parkinson’s disease. J Sex Marital Ther 30(2):95–105
Sakakibara R, Shinotoh H, Uchiyama T, Sakuma M, Kashiwado M, Yoshiyama M, Hattori T (2001) Questionnaire-based assessment of pelvic organ dysfunction in Parkinson’s disease. Auton Neurosci 92(1–2):76–85
Papatsoris AG, Deliveliotis C, Singer C, Papapetropoulos S (2006) Erectile dysfunction in Parkinson’s disease. Urology 67(3):447–451
Roumiguie M et al (2011) Assessment of sexual function in men with idiopathic Parkinson’s disease using the iInternational Index of Erectile Dysfunction (IIEF-15). Prog Urol 21(1):67–71
Farhadi F et al (2017) Sexual dimorphism in Parkinson’s disease: differences in clinical manifestations, quality of life and psychosocial functioning between males and females. Neuropsychiatr Dis Treat 13:329–338
Buhmann C et al (2017) The impact of Parkinson disease on patients’ sexuality and relationship. J Neural Transm (Vienna) 124(8):983–996
Gao X, Chen H, Schwarzschild MA, Glasser DB, Logroscino G, Rimm EB, Ascherio A (2007) Erectile function and risk of Parkinson’s disease. Am J Epidemiol 166(12):1446–1450
Yang Y et al (2017) Relationship between erectile dysfunction, comorbidity, and Parkinson’s disease: evidence from a population-based longitudinal study. J Clin Neurol 13(3):250–258
Hughes AJ et al (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55(3):181–184
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Chaudhuri KR et al (2007) The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 22(13):1901–1911
Shamloul R, Ghanem H, Abou-zeid A (2004) Validity of the Arabic version of the sexual health inventory for men among Egyptians. Int J Impot Res 16(5):452–455
Bronner G, Korczyn AD (2018) The role of sex therapy in the management of patients with Parkinson’s disease. Mov Disord Clin Pract 5(1):6–13
Kotkova P, Weiss P (2013) Psychiatric factors related to sexual functioning in patients with Parkinson’s disease. Clin Neurol Neurosurg 115(4):419–424
Okun MS, McDonald WM, DeLong MR (2002) Refractory nonmotor symptoms in male patients with Parkinson disease due to testosterone deficiency: a common unrecognized comorbidity. Arch Neurol 59(5):807–811
Goldstein DS (2003) Dysautonomia in Parkinson’s disease: neurocardiological abnormalities. Lancet Neurol 2(11):669–676
Reid WG et al (2011) Dementia in Parkinson’s disease: a 20-year neuropsychological study (Sydney Multicentre Study). J Neurol Neurosurg Psychiatry 82(9):1033–1037
Kummer A, Cardoso F, Teixeira AL (2009) Loss of libido in Parkinson’s disease. J Sex Med 6(4):1024–1031
Derouesné C, Guigot J, Chermat V, Winchester N, Lacomblez L (1996) Sexual behavioral changes in Alzheimer disease. Alzheimer Dis Assoc Disord 10(2):86–92
Tsai S-J et al (1999) Inappropriate sexual behaviors in dementia: a preliminary report. Alzheimer Dis Assoc Disord 13(1):60–62
Cannas A, Solla P, Floris GL, Serra G, Tacconi P, Marrosu MG (2007) Aberrant sexual behaviours in Parkinson’s disease during dopaminergic treatment. J Neurol 254(1):110–112
Harvey N (1988) Serial cognitive profiles in levodopa-induced hypersexuality. Br J Psychiatry 153(6):833–836
Bronner G, Cohen OS, Yahalom G, Kozlova E, Orlev Y, Molshatzki N, Strauss H, Hassin-Baer S (2014) Correlates of quality of sexual life in male and female patients with Parkinson disease and their partners. Parkinsonism Relat Disord 20(10):1085–1088
Moisan F et al (2016) Parkinson disease male-to-female ratios increase with age: French nationwide study and meta-analysis. J Neurol Neurosurg Psychiatry 87(9):952–957
Ozcan T et al (2016) The association between symptoms of sexual dysfunction and age at onset in Parkinson’s disease. Clin Auton Res 26(3):205–209
Wagle KC, Carrejo MH, Tan RS (2012) The implications of increasing age on erectile dysfunction. Am J Mens Health 6(4):273–279
Wickremaratchi MM et al (2011) The motor phenotype of Parkinson’s disease in relation to age at onset. Mov Disord 26(3):457–463
Okun MS, DeLong M, Hanfelt J, Gearing M, Levey A (2004) Plasma testosterone levels in Alzheimer and Parkinson diseases. Neurology 62(3):411–413
Celikel E, Ozel-Kizil ET, Akbostanci MC, Cevik A (2008) Assessment of sexual dysfunction in patients with Parkinson’s disease: a case-control study. Eur J Neurol 15(11):1168–1172
Lundberg PO (2015) Approach to the male patient with sexual dysfunction. Handb Clin Neurol 130:137–142
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical statement
The study was approved by the institutional Ethics Committee at the Faculty of Medicine, Ain Shams University. All subjects gave written informed consent according to the Declaration of Helsinki of 1975, as revised in 2008.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Shalash, A., Hamid, E., Elrassas, H. et al. Sexual dysfunction in male patients with Parkinson’s disease: related factors and impact on quality of life. Neurol Sci 41, 2201–2206 (2020). https://doi.org/10.1007/s10072-020-04328-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04328-2