Abstract
Background
Frailty is a construct recently introduced in the context of inflammatory joint diseases. To date, it is not clear if frailty can act as a negative factor in the achievement of comprehensive disease control (CDC) in patients suffering from rheumatoid arthritis (RA).
Aim
To verify whether frailty is a factor hindering the achievement of CDC in patients with RA starting a biologic drug.
Methods
RA patients requiring a treatment with a biologic drug were included. Patients were classified as achieving or not achieving CDC after 12 months of treatment. Patients were classified as non-frail, mildly frail, moderately frail and severely frail according to the Comprehensive Rheumatologic Assessment of Frailty (CRAF). Frailty was tested using the Mann–Whitney or Kruskal-Wallis test for continuous variables and chi-square test or Fisher’s exact test for comparison with categorical variables. A multivariable logistic regression was performed to identify factors associated with prediction of CDC achievers.
Results
A total of 214 RA patients were followed for 12 months, 14.5% achieved CDC. Eighty-four (39.3%) patients were non-frail, 57 (26.6%) were mildly frail, 14 (6.5%) were moderately frail and 59 (27.6%) were severely frail. The multivariable logistic regression analysis identified the CRAF score at baseline as an independent variable for CDC achievement at 12 months (p = 0.0040).
Discussion
Frailty is a frequent condition in RA patients and reduces the chances of achieving CDC.
Conclusions
Frailty, measured by CRAF, reduced the likelihood of CDC achievement in RA patients treated with a biologic agent.
Key Points • Frailty is an under-researched condition in rheumatoid arthritis affecting more than 60% of patients. • Frailty is a condition that hinders the achievement of comprehensive disease control after 1 year of treatment with biological drugs in patients with rheumatoid arthritis. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is an inflammatory autoimmune joint disease that can lead to a significant disability and poor quality of life [1]. RA is, in a certain way, considered an immunological “emergency”, and the introduction at an early stage of a treatment with disease-modifying anti-rheumatic drugs (DMARD) is essential to suppress inflammation, maintain normal joint structure and consequently preserve adequate function [2]. Today’s treatment options allow this adequate control of disease activity in most of patients [3]. However, there are different definitions of disease activity control. One of these is comprehensive disease control (CDC), which includes several domains related to RA. Achieving CDC means reaching precise targets in tools that assess disease activity, function and radiological damage. Achieving CDC has been shown to provide significant benefits to patients in terms of symptoms (reduced pain and fatigue), quality of life and work ability. The effectiveness of this strategy has been well demonstrated in clinical trials [4, 5]. Achieving CDC is desirable in each RA patient, especially in young patients and in the absence of comorbidity.
However, in everyday clinical practice, the rheumatologist has to deal with patients outside of the “ideal” setting of clinical trials, is increasingly in contact with elderly and comorbid patients and therefore has to relate with subjects at an increased risk of becoming frail. The concept of frailty is relatively recent and emerging in rheumatology. Frailty is a construct aimed at the recognition of individuals who are more vulnerable to adverse events and more predisposed to unfavourable outcomes. The term “frailty” is used to define a category of elderly adults who appear to be vulnerable and weaker than those of the same age with similar demographic characteristics. RA is a disease that predisposes to frailty. The prevalence of frailty in the RA is higher than that of geriatric cohorts: the prevalence is 13% in patients with RA [6], compared to 4–11% in older geriatric cohorts. Pre-frailty conditions are more prevalent in RA patients (69%) than in geriatric cohorts (40–55%) [7, 8].
In the rheumatological literature, there are no data on the impact of frailty in reaching important targets such as CDC. Starting from these considerations, the objective of this study was to verify whether frailty is a factor hindering the achievement of CDC in patients with RA.
Materials and methods
Study population and inclusion criteria
Between March 2016 and January 2020, adult patients with RA, as defined by the American College of Rheumatology/European League Against Rheumatism [9], with poorly controlled disease activity (defined by a Simplified Disease Activity Index [SDAI] > 11) with synthetic DMARDs and candidates for treatment with biological DMARDs (bDMARDs) were included in this study. Patients with contraindications to start treatment with bDMARDs, i.e. patients with ongoing infections, active neoplasms, congestive heart failure, pregnant women and patients with comorbidities that may hinder clinical evaluation, i.e. patients with Alzheimer’s disease or other dementias, Parkinson’s disease, ischemic encephalopathy or major depression, were excluded. Once included, the study had an observational character and patients were followed for 1 year after the introduction of bDMARDs in therapy. After 1 year, only patients who maintained treatment with bDMARDs were evaluated, excluding patients who suspended bDMARDs or switched to other bDMARDs or targeted synthetic DMARDs.
Baseline assessment
Data were collected on demography (age, gender), work activity and education (primary, middle or high school or university). With regard to RA, the duration of the disease (defined by the first swollen joint), the number of tender and swollen joints (on the 28-joint count), visual analogue scale of pain (VAS pain), the physician global assessment of the disease activity (PhGA) and the patient global assessment of disease activity (PaGA) were recorded.
Laboratory indicators included C-reactive protein (CRP), anti-cyclic citrullinated peptide antibodies (ACPA) and rheumatoid factor (RF).
Disease activity was defined by SDAI [10], functional status by the Health Assessment Questionnaire-Disability Index (HAQ-DI) [11], while the presence of frailty was determined by the Comprehensive Rheumatologic Assessment of Frailty (CRAF) [12]. A brief description of these three indices follows.
SDAI employs the algebraic sum of SJC, TJC (28-joint count for these two parameters), PtGA, PhGA and CRP (in mg/dl); values can vary from 0 to 86. A SDAI > 26 defines high disease activity, SDAI > 11 and ≤ 26 defines moderate disease activity, SDAI ≤ 11 and > 3.3 defines low activity and SDAI ≤ 3.3 defines remission [10].
The HAQ-DI evaluates the physical function by estimating the degree of difficulty in performing the activities in eight functional areas, the level of difficulty in the last week is indicated for each activity on a 4-point scale (from 0, no difficulty, to 3, inability to perform). The highest value is considered for each functional area. The final HAQ-DI score is given by the mean of the eight scales [11].
The CRAF is a validated multidimensional index recently developed. CRAF does not require a calculator and investigates 10 health domains (nutritional status, weakness, falls, comorbidity, polypharmacy, social activity, pain, fatigue, physical function and depression). The weight of each factor is attributed according to a predefined table. Among the instrumental equipment for its computation, only a dynamometer is needed to evaluate handgrip strength in the weakness domain [12]. Each domain is given a score of three 0 and 1, then the average of the 10 domains is calculated and the final score ranges from 0 (no deficits present) to 1 (all deficits present). The cut-offs of frailty categories were then defined on the basis of Clegg’s criteria [13]: scores from 0 to 0.12 represent the absence of frailty, scores between 0.12 and 0.24 indicate mild frailty, higher scores between 0.24 and 0.36 indicate moderate frailty, while scores greater than 0.36 indicate patients with severe frailty [12].
The definition of radiological damage used in the CDC calculation was based on the Simple Erosion Narrowing Score (SENS) [14]. X-rays of hands, wrists and feet were then evaluated by a musculoskeletal radiologist (MC) who determined the presence of joint rhyme reduction and the presence of erosion in the joints included in the score. The SENS score ranged from 0 to 86 [14].
Finally, comorbidities were weighed through the Rheumatic Disease Comorbidity Index (RDCI). The RDCI was developed as a tool to assess the effect of comorbidities on quality of life, physical function and costs. The RDCI formula is: 2* lung disease + [2* (myocardial infarction, other cardiovascular diseases or stroke) or 1* hypertension] + 1* (ulcer or other gastrointestinal diseases) + 1* for each of the following conditions: diabetes, fracture, depression and cancer [15].
Definition of 12-month comprehensive disease control
CDC achievement was evaluated after 12 months of bDMARD treatment. CDC was defined by the contemporary achievement of clinical remission (SDAI < 3.3), normal physical function (HAQ-DI < 0.5), absence of radiographic progression (worsening SENS < 2.28). The score of 2.28 was adopted for SENS because this value represents the smallest detectable change (SDD) for the tool [16].
Statistical analysis
Data were registered in a Microsoft Excel database and processed with MedCalc 19.0.6 (statistical software packages for Windows XP). The Shapiro-Wilk test was used to study the normal distribution. Data are presented both as mean and standard deviation (SD) and as median and interquartile range (IQR). CRAF scores were calculated and participants were classified as severely frail, moderately frail, mildly frail or non-frail. The comparison between the frailty categories was made using the Mann-Whitney U test or the Kruskal-Wallis test for continuous variables and the chi-square test or Fisher's exact test for comparison with the categorical variables. Spearman's non-parametric correlation coefficient was used to evaluate the relationships between clinical, functional and radiological measurements and CRAF scores. Differences in participants’ characteristics between the frailty categories were tested with one-way analysis of variance (ANOVA), or Kruskal-Wallis analysis, where appropriate. p values < 0.05 were considered statistically significant. Patients were categorized into CDC achievers vs CDC non-achievers, and the difference between variables (age, gender, educational level, disease duration, BMI, RDCI, RF, ACPA, CRAF and SENS) was firstly assessed with a univariate analysis (Student’s t test or Mann-Whitney U test). Then, to assess the contribution of the individual independent variables on CDC achievement (dependent variable), a multivariate logistic regression analysis was used.
Results
A total of 222 RA patients started the study. Eight patients (3.6%) were lost to follow-up and therefore were ruled out. After 1 year, complete data were available for 214 (96.4%) patients (162 women and 52 men), and those were included in the analyses. The mean (SD) age was 60.2 (12.72) years, with a mean (SD) disease duration of 7.34 (2.79) years, and a mean (SD) BMI of 26.39 (4.48). All patients had moderate or active disease, with a mean (SD) SDAI of 27.11 (12.61), and a mean (SD) HAQ-DI of 0.92 (0.54). A total of 149 (69.6%) patients were RF positive and 126 (58.9%) were ACPA positive. Of the 214 patients included, 145 (67.8%) reported one or more medical comorbidities, mostly cardiovascular (26.2%), respiratory (23.4%) and metabolic (22%) disorders. Polypharmacy was very common in our study population, with 57% of the patients receiving 5–8 drugs per day and 13.1% receiving 10 drugs per day or more. The mean number of drugs prescribed per day was 6.2 (SD 2.9, min = 0, max = 14). All patients were receiving at least one bDMARD, respectively, 59 (27.6%) etanercept, 54 (25.2%) adalimumab, 33 (15.4%) abatacept, 26 (12.2%) golimumab, 22 (10.3%) tocilizumab, 11 (5.1%) certolizumab pegol and 9 (4.2%) infliximab. The majority of the patients were on their first biologic agent. Approximately 61% of the patients receive a csDMARD, usually methotrexate (72.3%). A total of 102 patients (47.7%) were taking oral corticosteroids, at a mean prednisone or equivalent dose of 3.9 mg/day (range 2.5–16), and 131 (61.2%) were prescribed non-steroidal anti-inflammatory drugs (NSAIDs) on demand. Table 1 summarizes the baseline characteristics of the patients.
Figure 1 presents estimates of central tendency and distribution of the CRAF, which was non-normally distributed. The median of CRAF was 0.20 (IQR, 0.08–0.43) (Table 1), and according to CRAF definition, 84 (39.3 %) patients were non-frail, 57 (26.6%) were mildly frail, 14 (6.5%) were moderately frail and 59 (27.6%) were severely frail.
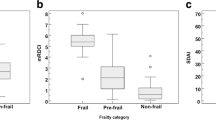
Distinguishing patients according to the CRAF category, after 12 months of treatment, the disease activity (Fig. 2a) and function (Fig. 2b) showed a significant improvement in non-frail patients compared to severely frail patients (p = 0.00013 for SDAI, p < 0.0001 for HAQ-DI). No significant changes were also identified with respect to the structural damage measured with SENS (p = 0.092).
Disease activity and functional ability according to frailty categories. Box–whisker plots showing the changes in the scores of Simplified Disease Activity Index (SDAI) (A) and of Health Assessment Questionnaire Disability Index (HAQ-DI) (B) after 12 months, in relation to the frailty categories (Kruskal-Wallis test) of the Comprehensive Rheumatologic Assessment of Frailty (CRAF). The horizontal lines in each box represent the median, and the box height represents the interquartile range
At 12 months, CDC was achieved in 31 (14.4%) patients versus 183 (85.6%) patients who did not achieve CDC. Table 2 summarizes the differences at baseline between variables in CDC achievers vs CDC non-achievers in the univariate analysis. Statistically significant differences emerged in all variables, which were subsequently included in the logistic regression analysis. The variables associated with CDC achievement in logistic regression analysis are presented in Table 3. The CRAF score was found to be the only independent variable significantly related (p = 0.004) to CDC achievement.
Table 4 shows the mean (SD) and median (IQR) change scores of SDAI, HAQ-DI and SENS at 12-month intervals in CDC achievers and in non-achievers. CDC achievers had significantly (p < 0.001) lower changes or worsening, in physical function (HAQ-DI) and disease activity (SDAI). No statistically significant changes (p = 0.092) were found in radiologic damage (SENS) between the two groups.
Discussion
This is the first study demonstrating that frailty is a condition that reduces the chances of achieving CDC in RA patients.
Achieving complete control of RA in terms of disease activity, function and joint damage is the ideal goal in all patients. Identifying the factors that hinder the achievement of this goal is a prerogative for the rheumatologist [17, 18].
Frailty is a syndrome with multiple causes contributing to its onset. Frailty is characterized by a reduction of strength, resistance and physiological functions, predisposing the subject to be more vulnerable and at greater risk of becoming dependent or dying [19,20,21]. Among its clinical expressiveness, RA can predispose patients to multiple factors included in the frailty definition [21].
Well-known in the geriatric field, where it has been documented that it is associated with multiple unfavourable outcomes (risk of hospitalization, institutionalization and death) [22, 23], frailty must also be recognized in other settings such as rheumatology since it is an evolutive but potentially reversible syndromic scenario [24, 25].
The prevalence of frailty (defined as severe frailty at CRAF) in our cohort of RA patients, with a mean age of 60 years, was 27.6%. This prevalence is significantly higher than that described in cohorts 10 years older. Pre-frailty conditions (mild and moderate frailty at CRAF) are in line with those of the geriatric cohorts [7, 8]. Compared to other cohorts of RA patients, who used the definition of the Survey of Health, Aging and Retirement in Europe–Frailty Instrument (SHARE-FI) [26], the prevalence observed in our study was higher. This may be due to the fact that SHARE-FI mainly evaluates frailty limited to a biopsychosocial paradigm. SHARE-FI is devoted to primary care; it does not take into account variables such as pain, fatigue and depression, very common conditions in RA patients [26].
The interrelationships between inflammation, physical fatigue, muscle dysfunction, pain and psychological factors have been suggested as implied pathogenic mechanisms of frailty in RA patients [27]. However, the specific mechanisms of frailty in RA have not been studied in detail. Previous studies demonstrated that a high disease activity, assessed by SDAI, was highly correlated to frailty [12, 28]. Systemic inflammation is closely linked to frailty [29]. RA is also characterized by early ageing of the immune system [30,31,32]. High levels of IL-6 and TNFα are correlated with reduced muscle mass and reduced strength [33, 34]. Frailty, reduced functional ability and reduced mobility are associated with higher levels of pro-inflammatory cytokines [35, 36]. Some experimental evidence also documents the direct action of certain cytokines on the central nervous system in favour of the perception of fatigue [37, 38]. Fatigue can be considered a manifestation of changes in neuronal function secondary to inflammatory stimuli [39]. IL-6, the pro-inflammatory cytokine by definition, can cross the blood-brain barrier and induce these neuronal changes.
Frailty is also predicted by pain, emphasizing the importance of its treatment, potentially contributing to the prevention of vulnerability, dependency and mortality [40]. Among comorbidities inducing frailty, depression is the most frequent in RA patients. A 2013 systematic review and meta-analysis found that 16.7% of those with RA meet diagnostic criteria for major depressive disorder [41]. Comorbid depression negatively impacts RA patients’ health-related quality of life, physical function, mental function, mortality and experience of pain and symptom severity [42]. Depressive symptoms may be a risk factor for frailty, causing changes in behaviour and activity that result in increased disability, leading to frailty [43]. Conversely, depressive symptoms may also be an early symptom of frailty. Sanders et al. demonstrates a strong association between pain and depressive symptoms over time [44]. Moreover, this association remained unaffected by follow-up time, age or frailty status. This interaction has been labelled by some as the depression-pain dyad [45]. With an increasing number of comorbidities occurring with ageing, a better understanding of the reciprocal link between pain and depression may identify factors suitable for prevention or improved treatment outcomes.
Pain and depression are other frailty-related variable. Of fundamental importance is the treatment of pain, which could contribute to avoid the onset of frailty itself and its consequences [40]. A detailed understanding of the interaction between pain and depression can lead to the identification of factors on which preventive interventions can be implemented.
Several limitations of our study should be recognized. First, since our main objective was to determine if frailty was associated with a therapeutic response, the analysis was limited to a time interval. Secondly, certain CRAF parameters, such as depression, were detected by a VAS in the thermometer format [46]. This type of patient-reported method is certainly not the optimal one. Third, the effect of other factors, such as the use of other drugs (e.g. corticosteroids), was not investigated. Fourth, although the components of CDC have been found in clinical trials, some variables, such as HAQ-DI, may be influenced by age, and over 65 years of age an HAQ-DI < 0.5 may be incorrect as a functional remission criterion [47]. Finally, few patients reached CDC at 12 months, so the analyses may have been affected by the small number of patients in this subgroup.
The main strength of this study is the prospective observational design, and the novelty of using a dedicated frailty index should be emphasized. The results of this study suggest dedicating more and more attention to frailty in patients with RA, in all its determinant variables, through dedicated tools such as CRAF or other validated frailty questionnaires [48].
Data availability
The data are available upon reasonable request to the corresponding author.
References
Dl S, Wolfe F, Huizinga TW (2010) Rheumatoid arthritis. Lancet 376:1094–1108. https://doi.org/10.1016/S0140-6736(10)60826-4
Smolen JS, Landewé RBM, Bijlsma JWJ, Burmester GR, Dougados M, Kerschbaumer A, McInnes IB, Sepriano A, van Vollenhoven RF, de Wit M, Aletaha D, Aringer M, Askling J, Balsa A, Boers M, den Broeder AA, Buch MH, Buttgereit F, Caporali R, Cardiel MH, de Cock D, Codreanu C, Cutolo M, Edwards CJ, van Eijk-Hustings Y, Emery P, Finckh A, Gossec L, Gottenberg JE, Hetland ML, Huizinga TWJ, Koloumas M, Li Z, Mariette X, Müller-Ladner U, Mysler EF, da Silva JAP, Poór G, Pope JE, Rubbert-Roth A, Ruyssen-Witrand A, Saag KG, Strangfeld A, Takeuchi T, Voshaar M, Westhovens R, van der Heijde D (2020) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 79:685–699. https://doi.org/10.1136/annrheumdis-2019-216655
Singh JA, Christensen R, Wells GA, et al (2009) Biologics for rheumatoid arthritis: an overview of Cochrane reviews. Cochrane Database Syst Rev CD007848. doi: https://doi.org/10.1002/14651858.CD007848.pub2
Emery P, Kavanaugh A, Bao Y, Ganguli A, Mulani P (2015) Comprehensive disease control (CDC): what does achieving CDC mean for patients with rheumatoid arthritis? Ann Rheum Dis 74:2165–2174. https://doi.org/10.1136/annrheumdis-2014-205302
Keystone EC, Breedveld FC, van der Heijde D et al (2017) Achieving comprehensive disease control in patients with early and established rheumatoid arthritis treated with adalimumab plus methotrexate versus methotrexate alone. RMD Open 3:e000445. https://doi.org/10.1136/rmdopen-2017-000445
Andrews JS, Trupin L, Yelin EH, Hough CL, Covinsky KE, Katz PP (2017) Frailty and reduced physical function go hand in hand in adults with rheumatoid arthritis: a US observational cohort study. Clin Rheumatol 36:1031–1039. https://doi.org/10.1007/s10067-017-3541-9
Cawthon PM, Marshall LM, Michael Y, Dam TT, Ensrud KE, Barrett-Connor E, Orwoll ES, for the Osteoporotic Fractures in Men Research Group (2007) Frailty in older men: prevalence, progression, and relationship with mortality. J Am Geriatr Soc 55:1216–1223. https://doi.org/10.1111/j.1532-5415.2007.01259.x
Bandeen-Roche K, Xue QL, Ferrucci L, Walston J, Guralnik JM, Chaves P, Zeger SL, Fried LP (2006) Phenotype of frailty: characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci 61:262–266. https://doi.org/10.1093/gerona/61.3.262
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO III, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JMW, Hobbs K, Huizinga TWJ, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Ménard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovský J, Wolfe F, Hawker G (2010) 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62:2569–2581. https://doi.org/10.1002/art.27584
Aletaha D, Smolen JS (2007) The Simplified Disease Activity Index (SDAI) and Clinical Disease Activity Index (CDAI) to monitor patients in standard clinical care. Best Pract Res Clin Rheumatol 21:663–675. https://doi.org/10.1016/j.berh.2007.02.004
Fries JF, Spitz P, Kraines RG, Holman HR (1980) Measurement of patient outcome in arthritis. Arthritis Rheum 23:137–145. https://doi.org/10.1002/art.1780230202
Salaffi F, Di Carlo M, Farah S, Carotti M (2020) The Comprehensive Rheumatologic Assessment of Frailty (CRAF): development and validation of a multidimensional frailty screening tool in patients with rheumatoid arthritis. Clin Exp Rheumatol 38:488–499
Cleggs A, Bates C, Young J et al (2016) Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 45:353–360. https://doi.org/10.1093/ageing/afw039
van der Heijde D, Dankert T, Nieman F, Rau R, Boers M (1999) Reliability and sensitivity to change of a simplification of the Sharp/van der Heijde radiological assessment in rheumatoid arthritis. Rheumatology (Oxford) 38:941–947. https://doi.org/10.1093/rheumatology/38.10.941
England BR, Sayles H, Mikuls TR, Johnson DS, Michaud K (2015) Validation of the rheumatic disease comorbidity index. Arthritis Care Res 67:865–872. https://doi.org/10.1002/acr.22456
Dias EM, Lukas C, Landewé R, Fatenejad S, van der Heijde D (2008) Reliability and sensitivity to change of the Simple Erosion Narrowing Score compared with the Sharp-van der Heijde method for scoring radiographs in rheumatoid arthritis. Ann Rheum Dis 67:375–379. https://doi.org/10.1136/ard.2007.072785
Verschueren P, Esselens G, Westhovens R (2009) Predictors of remission, normalized physical function, and changes in the working situation during follow-up of patients with early rheumatoid arthritis: an observational study. Scand J Rheumatol 38:166–172. https://doi.org/10.1080/03009740802484846
Kekow J, Moots RJ, Emery P, Durez P, Koenig A, Singh A, Pedersen R, Robertson D, Freundlich B, Sato R (2010) Patient-reported outcomes improve with etanercept plus methotrexate in active early rheumatoid arthritis and the improvement is strongly associated with remission: the COMET trial. Ann Rheum Dis 69:222–225. https://doi.org/10.1136/ard.2008.102509
Gobbens RJ, Van Assen MA, Luijkx KG, Schols JM (2012) Testing an integral conceptual model of frailty. J Adv Nurs 68:2047–2060. https://doi.org/10.1111/j.1365-2648.2011.05896.x
Morley JE, Vellas B, Van Kan GA et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14:392–397. https://doi.org/10.1016/j.jamda.2013.03.022
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156. https://doi.org/10.1093/gerona/56.3.m146
Pugh JA, Wang CP, Espinoza SE, Noël PH, Bollinger M, Amuan M, Finley E, Pugh MJ (2014) Influence of frailty-related diagnoses. High-risk prescribing in elderly adults and primary care use on readmissions in fewer than 30 days for veterans aged 65 and older. J Am Geriatr Soc 62:291–298. https://doi.org/10.1111/jgs.12656
Joosten E, Demuynck M, Detroyer E, Milisen K (2014) Prevalence of frailty and its ability to predict in hospital delirium, falls, and 6-month mortality in hospitalized older patients. BMC Geriatr 14:1. https://doi.org/10.1186/1471-2318-14-1
Gill TM, Gahbauer EA, Allore HG, Han L (2006) Transitions between frailty states among community-living older persons. Arch Intern Med 166:418–423. https://doi.org/10.1001/archinte.166.4.418
Haider S, Grabovac I, Berner C, Lamprecht T, Fenzl KH, Erlacher L, Quittan M, Dorner TE (2019) Frailty in seropositive rheumatoid arthritis patients of working age: a cross-sectional study. Clin Exp Rheumatol 37:585–592
Romero-Ortuno R (2011) The Frailty Instrument of the Survey of Health, Ageing and Retirement in Europe (SHARE-FI) predicts mortality beyond age, comorbidities, disability, self-rated health, education and depression. Eur Geriatr Med 2:323–326. https://doi.org/10.1016/j.eurger.2011.08.005
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381:752–762. https://doi.org/10.1016/S0140-6736(12)62167-9
Salaffi F, Di Carlo M, Farah S, Di Donato E, Carotti M (2019) Prevalence of frailty and its associated factors in patients with rheumatoid arthritis: a cross-sectional analysis. Clin Rheumatol 38:1823–1830. https://doi.org/10.1007/s10067-019-04486-5
Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A (2018) Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat Rev Endocrinol 14:576–590
Fujii H, Shao L, Colmegna I, Goronzy JJ, Weyand CM (2009) Telomerase insufficiency in rheumatoid arthritis. Proc Natl Acad Sci U S A 106:4360–4365. https://doi.org/10.1038/s41574-018-0059-4
Weyand CM, Fujii H, Shao L, Goronzy JJ (2009) Rejuvenating the immune system in rheumatoid arthritis. Nat Rev Rheumatol 5:583–588. https://doi.org/10.1038/nrrheum.2009.180
Koetz K, Bryl E, Spickschen K, O'fallon WM, Goronzy JJ, Weyand CM (2000) T cell homeostasis in patients with rheumatoid arthritis. Proc Natl Acad Sci U S A 97:9203–9208. https://doi.org/10.1073/pnas.97.16.9203
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB (2002) Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci 57:M326–M332. https://doi.org/10.1093/gerona/57.5.m326
Leng S, Chaves P, Koenig K, Walston J (2002) Serum interleukin-6 and hemoglobin as physiological correlates in the geriatric syndrome of frailty: a pilot study. J Am Geriatr Soc 50:1268–1271. https://doi.org/10.1046/j.1532-5415.2002.50315.x
Langmann GA, Perera S, Ferchak MA, Nace DA, Resnick NM, Greenspan SL (2017) Inflammatory markers and frailty in long-term care residents. J Am Geriatr Soc 65:1777–1783. https://doi.org/10.1111/jgs.14876
Soysal P, Stubbs B, Lucato P, Luchini C, Solmi M, Peluso R, Sergi G, Isik AT, Manzato E, Maggi S, Maggio M, Prina AM, Cosco TD, Wu YT, Veronese N (2016) Inflammation and frailty in the elderly: A systematic review and meta-analysis. Ageing Res Rev 31:1–8. https://doi.org/10.1016/j.arr.2016.08.006
Banks WA (2005) Blood-brain barrier transport of cytokines: a mechanism for neuropathology. Curr Pharm Des 11:973–984. https://doi.org/10.2174/1381612053381684
Varlagadda A, Alfson E, Clayton AH (2009) The blood brain barrier and the role of cytokines in neuropsychiatry. Psychiatry (Edgmont) 6:18–22
Dantzer R, Kelley KW (2007) Twenty years of research on cytokine induced sickness behavior. Brain Behav Immun 21:153–160. https://doi.org/10.1016/j.bbi.2006.09.006
Coelho T, Paúl C, Gobbens RJJ, Fernandes L (2017) Multidimensional frailty and pain in community dwelling elderly. Pain Med 18:693–701. https://doi.org/10.1111/pme.12746
Matcham F, Rayne L, Steer S, Hotopf M (2013) The prevalence of depression in rheumatoid arthritis: a systematic review and meta-analysis. Rheumatology (Oxford) 52:2136–2148. https://doi.org/10.1093/rheumatology/ket169
Li N, Chan E, Peterson S (2019) The economic burden of depression among adults with rheumatoid arthritis in the United States. J Med Econ 22:372–378. https://doi.org/10.1080/13696998.2019.1572015
Aprahamian I, Suemoto CK, Lin SM, de Siqueira ASS, Biella MM, de Melo BAR, Jacob-Filho W (2019) Depression is associated with self-rated frailty in older adults from an outpatient clinic: a prospective study. Int Psychogeriatr 31:425–434. https://doi.org/10.1017/S104161021800100X
Sanders JB, Comijs HC, Bremmer MA, Deeg DJ, Beekman AT (2015) A 13-year prospective cohort study on the effects of aging and frailty on the depression-pain relationship in older adults. Int J Geriatr Psychiatry 30:751–757. https://doi.org/10.1002/gps.4224
Bair MJ, Robinson RL, Katon W, Kroenke K (2003) Depression and pain comorbidity: a literature review. Arch Intern Med 163:2433–2445. https://doi.org/10.1001/archinte.163.20.2433
Salaffi F, Di Carlo M, Carotti M, Farah S (2018) The Patient-Reported Outcomes Thermometer-5-Item Scale (5T-PROs): Validation of a New Tool for the Quick Assessment of Overall Health Status in Painful Rheumatic Diseases. Pain Res Manag 2018:3496846. https://doi.org/10.1155/2018/3496846
Yoshii I, Chijiwa T, Sawada N (2019) Validity of adopting a Health Assessment Questionnaire Disability Index less than 0.5 as a target in elderly rheumatoid arthritis patients. Clin Rheumatol 38:3351–3360. https://doi.org/10.1007/s10067-019-04692-1
Oetsma S, Boonen A, Starmans M, Peeters R, Van Onna M (2020) Validation of two frailty questionnaires in older patients with rheumatoid arthritis: a cross-sectional study. Clin Exp Rheumatol 38:523–528
Code availability
Not applicable.
Funding
Open access funding provided by Università Politecnica delle Marche within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
FS, RDA and MC conceived the study. FS, SF and MDC were involved in data collection. FS and MDC interpreted the data. FS was the major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures carried out in the study were approved by the local Ethics Committee (Comitato Unico Regionale–number 2015 0458 AS) and were in accordance with the Helsinki Declaration of 1975 and its later amendments.
Consent to participate
All patients approved participation in the study, signed informed consent
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salaffi, F., De Angelis, R., Farah, S. et al. Frailty as a novel predictor of achieving comprehensive disease control (CDC) in rheumatoid arthritis. Clin Rheumatol 40, 4869–4877 (2021). https://doi.org/10.1007/s10067-021-05744-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05744-1