Abstract
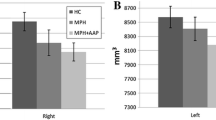
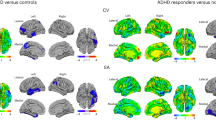
Methylphenidate (MPH) is the first choice of medical treatment for attention-deficit/hyperactivity disorder (ADHD). Its mechanism of action is to inhibit the reuptake of dopamine and noradrenaline mainly in the region of the striatum. It has been estimated that 10–30 % of patients with ADHD do not respond adequately to MPH. The aim of this study was to evaluate whether striatal differences exist between good and poor responders to MPH. The sample included 27 treatment-naïve children with ADHD between the ages of 6 and 14. MPH administration started 1 day after the MRI acquisition. After a month, psychiatrists established the good or poor response to treatment according to clinical criteria. MRI images were analyzed using a technique based on regions of interest applied specifically to the caudate and accumbens nuclei. Sixteen patients showed good response to MPH and 11 a poor one. Regions of interest analysis showed that good responders had a higher concentration of gray matter in the head of both caudate nuclei and the right nucleus accumbens. Furthermore, a significant correlation was found between caudate and accumbens nuclei volume and the Conners’ Parent Rating Scale and Continuous Performance Test improvement. These results support the hypothesis of the involvement of the caudate and accumbens nuclei in MPH response and in ADHD pathophysiology.


Similar content being viewed by others
References
Achenbach TM, Ruffle TM (2000) The child behavior checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev 21(8):265–271
Almeida Montes LG, Ricardo-Garcell J, De La Torre Barajas LB, Prado Alcántara H, Martínez García RB, Fernández-Bouzas A, Avila Acosta D (2010) Clinical correlations of grey matter reductions in the caudate nucleus of adults with attention deficit hyperactivity disorder. J Psychiatry Neurosci 35(4):238–246
Amador-Campos JA, Idiázabal-Alecha MA, Sangorrín-García J, Espadaler-Gamissans JM, Forns-Santacana M (2002) Utilidad de las escalas de Conners para discriminar entre sujetos con y sin trastorno por déficit de atención con hiperactividad. Psicothema 14(2):350–356
American Psychiatric Association (2004) Diagnostic and statistical manual of mental disorders, 4ª edn. American Psychiatric Association, Washington DC
Barkley RA (1976) Predicting the response of hyperkinetic children to stimulant drugs: a review. J Abnorm Child Psychol 4(4):327–348
Blouin B, Maddeaux C, Stanley Firestone J, van Stralen J (2010) Predicting response of ADHD symptoms to methylphenidate treatment based on comorbid anxiety. J Atten Disord 13(4):414–419
Buitelaar JK, Van der Gaag RJ, Swaab-Barneveld H, Kuiper M (1995) Prediction of clinical response to methylphenidate in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 34(8):1025–1032
Bush G, Spencer TJ, Holmes J, Shin LM, Valera EM, Seidman LJ, Makris N, Surman C, Aleardi M, Mick E, Biederman J (2008) Functional magnetic resonance imaging of methylphenidate and placebo in attention-deficit/hyperactivity disorder during the multi-source interference task. Arch Gen Psychiatry 65(1):102–114
Carmona S, Proal E, Hoekzema EA, Gispert JD, Picado M, Moreno I, Soliva JC, Bielsa A, Rovira M, Hilferty J, Bulbena A, Casas M, Tobeña A, Vilarroya O (2009) Ventro-striatal reductions underpin symptoms of hyperactivity and impulsivity in attention-deficit/hyperactivity disorder. Biol Psychiatry 66(10):972–977
Castellanos FX, Elia J, Kruesi MJ, Marsh WL, Gulotta CS, Potter WZ, Ritchie GF, Hamburger SD, Rapoport JL (1996) Cerebrospinal fluid homovanillic acid predicts behavioral response to stimulants in 45 boys with attention deficit/hyperactivity disorder. Neuropsychopharmacology 14(2):125–137
Castellanos FX, Giedd JN, Berquin PC, Walter JM, Sharp W, Tran T, Vaituzis AC, Blumenthal JD, Nelson J, Bastain TM, Zijdenbos A, Evans AC, Rapoport JL (2001) Quantitative brain magnetic resonance imaging in girls with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 58(3):289–295
Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenstein DK, Clasen LS, Blumenthal JD, James RS, Ebens CL, Walter JM, Zijdenbos A, Evans AC, Giedd JN, Rapoport JL (2002) Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA 288(14):1740–1748
Conners C (2004) Conners’ continuous performance test II version 5 (CPT II V.5). TEA Ediciones, Madrid
Conners C, Sitarenios G, Parker J, Epstein J (1998) The revised Conners parent rating scale (CPRS-S): factor structure, reliability, and criterion validity. J Abnorm Child Psychol 26(4):257–268
Conners C, Sitarenios G, Parker J, Epstein J (1998) Revision and restandardization of the Conners teacher rating scale (StRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol 26(4):279–291
Duong S, Chung K, Wigal SB (2012) Metabolic, toxicological, and safety considerations for drugs used to treat ADHD. Expert Opin Drug Metab Toxicol 8(5):543–552
Efron D, Jarman F, Barker M (1997) Methylphenidate versus dexamphetamine in children with attention deficit hyperactivity disorder: a double-blind, crossover trial. Pediatrics 100(6):E6
Epstein JN, Casey BJ, Tonev ST, Davidson MC, Reiss AL, Garrett A, Hinshaw SP, Greenhill LL, Glover G, Shafritz KM, Vitolo A, Kotler LA, Jarrett MA, Spicer J (2007) ADHD- and medication-related brain activation effects in concordantly affected parent-child dyads with ADHD. J Child Psychol Psychiatry 48(9):899–913
Filipek PA, Semrud-Clikeman M, Steingard RJ, Renshaw PF, Kennedy DN, Biederman J (1997) Volumetric MRI analysis comparing subjects having attention-deficit hyperactivity disorder with normal controls. Neurology 48(3):589–601
Grizenko N, Kovacina B, Amor LB, Schwartz G, Ter-Stepanian M, Joober R (2006) Relationship between response to methylphenidate treatment in children with ADHD and psychopathology in their families. J Am Acad Child Adolesc Psychiatry 45(1):47–53
Grupo de trabajo de la Guía de Práctica Clínica sobre el Trastorno por Défi cit de Atención con Hiperactividad (TDAH) en Niños y Adolescentes. Fundació Sant Joan de Déu, coordinador. Guía de Práctica Clínica sobre el Trastorno por Défi cit de Atención con Hiperactividad (TDAH) en Niños y Adolescentes. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad, Política Social e Igualdad. Agència d′Informació, Avaluació i Qualitat (AIAQS) de Cataluña; 2010. Guías de Práctica Clínica en el SNS: AATRM Nº 2007/18
Gunduz H, Wu H, Ashtari M, Bogerts B, Crandall D, Robinson DG, Alvir J, Lieberman J, Kane J, Bilder R (2002) Basal ganglia volumes in first-episode schizophrenia and healthy comparison subjects. Biol Psychiatry 51(10):801–808
Guy W (1976) Early Clinical Drug Evaluation (ECDEU) assessment manual for psychopharmacology. National Institute of Mental Health, Washington DC
Hale JB, Reddy LA, Semrud-Clikeman M, Hain LA, Whitaker J, Morley J, Lawrence K, Smith A, Jones N (2011) Executive impairment determines ADHD medication response: implications for academic achievement. J Learn Disabil 44(2):196–212
Hoekzema E, Carmona S, Ramos-Quiroga JA, Canals C, Moreno A, Fernández VR, Picado M, Bosch R, Duñó L, Soliva JC, Rovira M, Bulbena A, Tobeña A, Casas M, Vilarroya O (2012) Stimulant drugs trigger transient volumetric changes in the human ventral striatum. Brain Struct Funct. doi:10.1007/s00429-012-0481-7
Ilgin N, Senol S, Gucuyener K, Gokcora N, Sener S (2001) Is increased D2 receptor availability associated with response to stimulant medication in ADHD. Dev Med Child Neurol 43(11):755–760
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36(7):980–988
Mahone EM, Crocetti D, Ranta ME, Gaddis A, Cataldo M, Slifer KJ, Denckla MB, Mostofsky SH (2011) A preliminary neuroimaging study of preschool children with ADHD. Clin Neuropsychol 25(6):1009–1028
MTA cooperative group (2004) National Institute of Mental Health multimodal treatment study of ADHD follow-up: changes in effectiveness and growth after the end of treatment. Pediatrics 113(4):762–769
Mulas F, Roselló B, Morant A, Hernández S, Pitarch I (2002) Efectos de los psicoestimulantes en el desempeño cognitivo y conductual de los niños con un déficit de atención con hiperactividad subtipo combinado. Rev Neurol 35(1):17–24
Nakao T, Radua J, Rubia K, Mataix-Cols D (2011) Gray matter volume abnormalities in ADHD: voxel-based meta-analysis exploring the effects of age and stimulant medication. Am J Psychiatry 168(11):1154–1163
Owens EB, Hinshaw SP, Kraemer HC, Arnold LE, Abikoff HB, Cantwell DP, Conners CK, Elliott G, Greenhill LL, Hechtman L, Hoza B, Jensen PS, March JS, Newcorn JH, Pelham WE, Severe JB, Swanson JM, Vitiello B, Wells KC, Wigal T (2003) Which treatment for whom for ADHD? Moderators of treatment response in the MTA. J Consult Clin Psychol 71(3):540–552
Pelham WE Jr, Walker JL, Sturges J, Hoza J (1989) Comparative effects of methylphenidate on ADD girls and ADD boys. J Am Acad Child Adolesc Psychiatry 28(5):773–776
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164(6):942–948
Rapport MD, Denney C (1997) Titrating methylphenidate in children with attention-deficit/hyperactivity disorder: is body mass predictive of clinical response? J Am Acad Child Adolesc Psychiatry 36(4):523–530
Riccio CA, Waldrop JJ, Reynolds CR, Lowe P (2001) Effects of stimulants on the continuous performance test (CPT): implications for CPT use and interpretation. J Neuropsychiatry Clin Neurosci 13(3):326–335
Rubia K, Halari R, Cubillo A, Smith AB, Mohammad AM, Brammer M, Taylor E (2011) Methylphenidate normalizes fronto-striatal underactivation during interference inhibition in medication-naïve boys with attention-deficit hyperactivity disorder. Neuropsychopharmacology 36(8):1575–1586
Rubio B, Hernández S, Verche E, Martín R, González-Pérez P (2011) A pilot study: differential effects of methylphenidate-OROS on working memory and attention functions in children with attention-deficit/hyperactivity disorder with and without behavioural comorbidities. Atten Defic Hyperact Disord 3(1):13–20
Scheres A, Oosterlaan J, Sergeant JA (2006) Speed of inhibition predicts teacher-rated medication response in boys with attention deficit hyperactivity disorder. IJDDE 53:93–109
Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S (1983) A children’s global assessment scale (CGAS). Arch Gen Psychiatry 40(11):1228–1231
Shekim WO, Javaid J, Davis JM, Bylund DB (1983) Urinary MHPG and HVA excretion in boys with attention deficit disorder and hyperactivity treated with d-amphetamine. Biol Psychiatry 18(6):707–714
Solanto M, Newcorn J, Vail L, Gilbert S, Ivanov I, Lara R (2009) Stimulant drug response in the predominantly inattentive and combined subtypes of attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 19(6):663–671
Spielberger CD, Gorsuch RL, Lushene RE (1970) Manual for the state/trait anxiety inventory in children (version española TEA 1988). Consulting Psychologists Press, Palo Alto
Ter-Stepanian M, Grizenko N, Zappitelli M, Joober R (2010) Clinical response to methylphenidate in children diagnosed with attention-deficit hyperactivity disorder and comorbid psychiatric disorders. Can J Psychiatry 55(5):305–312
The MTA cooperative group (1999) Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: the multimodal treatment study of children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 56(12):1088–1096
Tremols V, Bielsa A, Soliva JC, Raheb C, Carmona S, Tomas J, Gispert JD, Rovira M, Fauquet J, Tobeña A, Bulbena A, Vilarroya O (2008) Differential abnormalities of the head and body of the caudate nucleus in attention deficit-hyperactivity disorder. Psychiatry Res 163(3):270–278
van der Oord S, Geurts HM, Prins PJ, Emmelkamp PM, Oosterlaan J (2012) Prepotent response inhibition predicts treatment outcome in attention deficit/hiperactivity disorder. Child Neuropsychol 18(1):50–61
van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp PM (2008) Treatment of attention deficit hyperactivity disorder in children. Eur Child Adolesc Psychiatry 17(2):73–81
Volkow ND, Wang GJ, Fowler JS, Telang F, Maynard L, Logan J, Gatley SJ, Pappas N, Wong C, Vaska P, Zhu W, Swanson JM (2004) Evidence that methylphenidate enhances the saliency of a mathematical task by increasing dopamine in the human brain. Am J Psychiatry 161(7):1173–1180
Volkow ND, Wang GJ, Tomasi D, Kollins SH, Wigal TL, Newcorn JH, Telang FW, Fowler JS, Logan J, Wong CT, Swanson JM (2012) Methylphenidate-elicited dopamine increases in ventral striatum are associated with long-term symptom improvement in adults with attention deficit hyperactivity disorder. J Neurosci 32(3):841–849
Wechsler D (2005) Escala de Inteligencia de Wechsler para niños (WISC-IV). TEA Ediciones, Madrid
Woodward ND, Zald DH, Ding Z, Riccardi P, Ansari MS, Baldwin RM, Cowan RL, Li R, Kessler RM (2009) Cerebral morphology and dopamine D2/D3 receptor distribution in humans: a combined [18F]fallypride and voxel-based morphometry study. Neuroimage 46(1):31–38
Yildiz O, Sismanlar SG, Memik NC, Karakaya I, Agaoglu B (2011) Atomoxetine and methylphenidate treatment in children with ADHD: the efficacy, tolerability and effects on executive functions. Child Psychiatry Hum Dev 42(3):257–269
Zalsman G, Pumeranz O, Peretz G, Ben-Dor DH, Dekel S, Horesh N, Fischel T, Nahshoni E, Goldberg PH, Sever J, Apter A (2003) Attention patterns in children with attention deficit disorder with or without hyperactivity. Sci World J 3:1093–1107
Acknowledgments
This research was supported by the Alicia Koplowitz Foundation Grant.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moreno, A., Duñó, L., Hoekzema, E. et al. Striatal volume deficits in children with ADHD who present a poor response to methylphenidate. Eur Child Adolesc Psychiatry 23, 805–812 (2014). https://doi.org/10.1007/s00787-013-0510-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-013-0510-y