Abstract
Objectives
The aim of this systematic review was to evaluate the prevalence of temporomandibular joint disorders (TMJD) among the general population.
Materials and methods
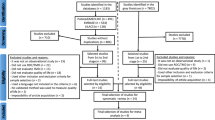
Five main electronic databases and three grey literature were searched to identify observational studies in which TMJD was diagnosed using the research diagnostic criteria (RDC/TMD) or diagnostic criteria (DC/TMD). The studies were blindly selected by two reviewers based on eligibility criteria. Risk of bias (RoB) was assessed using the Joanna Briggs Institute Critical Appraisal Checklist, and the “R” Statistics software was used to perform meta-analyses.
Results
From 2741 articles, 21 were included. Ten studies were judged at low RoB, seven at moderate, and four at high. The TMJD investigated were as follows: arthralgia, disk displacement (DDs) with reduction (DDwR), DDwR with intermittent locking, DDs without reduction (DDwoR) with limited opening, DDwoR without limited opening, degenerative joint disease (DJD), osteoarthritis, osteoarthrosis, and subluxation. The main results from prevalence overall meta-analyses for adults/elderly are as follows: TMJD (31.1%), DDs (19.1%), and DJD (9.8%). Furthermore, for children/adolescents are as follows: TMJD (11.3%), DDs (8.3%), and DJD (0.4%). Considering the individual diagnosis meta-analyses, the most prevalent TMJD is DDwR for adults/elderly (25.9%) and children/adolescents (7.4%).
Conclusions
The overall prevalence of TMJD was approximately 31% for adults/elderly and 11% for children/adolescents, and the most prevalent TMJD was DDwR.
Clinical relevance
Knowledge about the frequency of TMJD can encourage dentists to consider appropriate strategies for early and correct diagnosis and, if need be, correct management.


Similar content being viewed by others
References
de Leeuw R, Klasser GD (2013) Orofacial pain: guidelines for assessment, diagnosis, and management. Quintessence, New York
National Institute of Dental and Craniofacial Research (2018) Prevalence of TMJD and its signs and symptoms. https://www.nidcr.nih.gov/research/data-statistics/facial-pain/prevalence. Accessed 26 March 2020
List T, Jensen RH (2017) Temporomandibular disorders: old ideas and new concepts. Cephalalgia 37(7):692–704. https://doi.org/10.1177/0333102416686302
Bender SD (2012) Temporomandibular disorders, facial pain, and headaches. Headache 52(Suppl 1):22–25. https://doi.org/10.1111/j.1526-4610.2012.02134.x
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo F, Michelotti A, Brooks SL, Ceusters W, Drangsholt M, Ettlin D, Gaul C, Goldberg LJ, Haythornthwaite JA, Hollender L, Maixner W, van der Meulen M, Murray GM, Nixdorf DR, Palla S, Petersson A, Pionchon P, Smith B, Visscher CM, Zakrzewska J, Dworkin SF (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J Oral Facial Pain Headache 28(1):6–27. https://doi.org/10.11607/jop.1151
Dworkin SF, Leresche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Temporomandib Disord 6(4):301–355
(2020) International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia 40(2):129–221. https://doi.org/10.1177/0333102419893823
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:g7647. https://doi.org/10.1136/bmj.g7647
Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L (2011) An international registry of systematic-review protocols. Lancet 377(9760):108–109. https://doi.org/10.1016/S0140-6736(10)60903-8
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan - a web and mobile app for systematic reviews. Syst Rev 5(1):210. https://doi.org/10.1186/s13643-016-0384-4
Munn Z, Moola S, Riitano D, Lisy K (2014) The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag 3(3):123–128. https://doi.org/10.15171/ijhpm.2014.71
Polmann H, Domingos FL, Melo G, Stuginski-Barbosa J, Guerra ENDS, Porporatti AL, Dick BD, Flores-Mir C, De Luca CG (2019) Association between sleep bruxism and anxiety symptoms in adults: a systematic review. J Oral Rehabil 46(5):482–491. https://doi.org/10.1111/joor.1278
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1(2):97–111. https://doi.org/10.1002/jrsm.12
Marpaung C, van Selms MKA, Lobbezoo F (2018) Temporomandibular joint anterior disc displacement with reduction in a young population: prevalence and risk indicators. Int J Paediatr Dent 29(1):66–73. https://doi.org/10.1111/ipd.12426
Schmitter M, Essig M, Seneadza V, Balke Z, Schroder J, Rammelsberg P (2010) Prevalence of clinical and radiographic signs of osteoarthrosis of the temporomandibular joint in an older person community. Dentomaxillofac Radiol 39(4):231–234. https://doi.org/10.1259/dmfr/16270943
Progiante P, Pattussi M, Lawrence H, Goya S, Grossi P, Grossi M (2015) Prevalence of temporomandibular disorders in an adult Brazilian community population using the research diagnostic criteria (axes I and II) for temporomandibular disorders (the Maringá Study). Int J Prosthodont 28(6):600–609. https://doi.org/10.11607/ijp.4026
Pereira LJ, Pereira-Cenci T, Cury AADB, Pereira SM, Pereira AC, Ambosano GMB, Gavião MBD (2010) Risk indicators of temporomandibular disorder incidences in early adolescence. Am Acad Pediatr Dent 32(4):324–328
Wu N, Hirsch C (2010) Temporomandibular disorders in German and Chinese adolescents. J Orofac Orthop 71(3):187–198. https://doi.org/10.1007/s00056-010-1004-x
Al-Khotani A, Naimi-Akbar A, Albadawi E, Ernberg M, Hedenberg-Magnusson B, Christidis N (2016) Prevalence of diagnosed temporomandibular disorders among Saudi Arabian children and adolescents. J Headache Pain 17(1):41. https://doi.org/10.1186/s10194-016-0642-9
Graue AM, Jokstad A, Assmus J, Skeie MS (2016) Prevalence among adolescents in Bergen, Western Norway, of temporomandibular disorders according to the DC/TMD criteria and examination protocol. Acta Odontol Scand 74(6):449–455. https://doi.org/10.1080/00016357.2016.1191086
Aravena PC, Arias R, Aravena-Torres R, Seguel-Galdames F (2016) Prevalencia de trastornos temporomandibulares en adolescentes del Sur de Chile, año 2015. Rev Clin Periodoncia Implantol Rehabil Oral 9(3):244–252. https://doi.org/10.1016/j.piro.2016.09.005
Nguyen MS, Jagomägi T, Nguyen T, Saag M, Voog-Oras Ü (2017) Symptoms and signs of temporomandibular disorders among elderly Vietnamese. Proc Singapore Healthc 26(4):211–216. https://doi.org/10.1177/2010105817694907
Bertoli FMP, Bruzamolin CD, Pizzatto E, Losso EM, Brancher JA, de Souza JF (2018) Prevalence of diagnosed temporomandibular disorders: a cross-sectional study in Brazilian adolescents. PLoS One 13(2):e0192254. https://doi.org/10.1371/journal.pone.0192254
de Melo Júnior PC, Aroucha JMCNL, Arnaud M, Lima MGS, Gomes SGF, Ximenes R, Rosenblatt A, Caldas AF Jr (2019) Prevalence of TMD and level of chronic pain in a group of Brazilian adolescents. PLoS One 14(2):e0205874. https://doi.org/10.1371/journal.pone.0205874
Wieckiewicz M, Grychowska N, Nahajowski M, Hnitecka S, Kempiak K, Charemska K, Balicz A, Chirkowska A, Zietek M, Winocur E (2019) Prevalence and overlaps of headaches and pain-related temporomandibular disorders among the polish urban population. J Oral Facial Pain Headache 34(1):31–19. https://doi.org/10.11607/ofph.2386
Nilsson IM, List T, Drangsholt M (2006) The reliability and validity of self-reported temporomandibular disorder pain in adolescents. J Orofac Pain 20(2):138–144
Hirsch C, John MT, Stang A (2008) Association between generalized joint hypermobility and signs and diagnoses of temporomandibular disorders. Eur J Oral Sci 116(6):525–530. https://doi.org/10.1111/j.1600-0722.2008.00581.x
Balke Z, Rammelsberg P, Leckel M, Schmitter M (2010) Prevalence of temporomandibular disorders: samples taken from attendees of medical health-care centers in the Islamic Republic of Iran. J Orofac Pain 24(4):361–366
Hirsch C, Hoffmann J, Türp JC (2012) Are temporomandibular disorder symptoms and diagnoses associated with pubertal development in adolescents? An epidemiological study. J Orofac Orthop 73(1):6–18. https://doi.org/10.1007/s00056-011-0056-x
Paduano S, Bucci R, Rongo R, Silva R, Michelotti A (2018) Prevalence of temporomandibular disorders and oral parafunctions in adolescents from public schools in Southern Italy. Cranio 38(6):370–375. https://doi.org/10.1080/08869634.2018.1556893
Sandoval I, Ibarra N, Flores G, Marinkovic K, Díaz W, Romo F (2015) Prevalencia de trastornos temporomandibulares según los CDI/TTM, en un grupo de adultos mayores de Santiago, Chile. Int J Odontostomat 9(1):73–78. https://doi.org/10.4067/S0718-381X2015000100011
Loster JE, Osiewicz MA, Groch M, Ryniewicz W, Wieczorek A (2015) The prevalence of TMD in polish young adults. J Prosthodont 26(4):284–288. https://doi.org/10.1111/jopr.12414
Murrieta J, Alvarado E, Valdez M, Orozco L, Meza J, Juárez ML (2016) Prevalence of temporomandibular joint disorders in a Mexican elderly group. J Oral Res 5(1):13–18. https://doi.org/10.17126/joralres.2016.004
Guerrero L, Coronado L, Maulén M, Meeder W, Henríquez C, Lovera M (2017) Prevalencia de trastornos temporomandibulares en la población adulta beneficiaria de Atención Primaria en Salud del Servicio de Salud Valparaíso, San Antonio. Av Odontoestomatol 33(3):113–120
Svensson P, Graven-Nielsen T (2001) Craniofacial muscle pain: review of mechanisms and clinical manifestations. J Orofac Pain 15(2):117–145
Kosminsky M, Lucena LBS, Siqueira JTT, Pereira FJ Jr, Góes PSA (2004) Adaptação cultural do questionário research diagnostic criteria for temporomandibular disorders: Axis II para o português. J Bras Clin Odontol Integr 8(43):51–61
Góes PSA, Fernandes LMA, Lucena LBS (2006) Validação de instrumentos de coleta de dados. In: Antunes JLF, Peres MA (eds) Fundamentos de odontologia - Epidemiologia da saúde bucal. Guanabara Koogan, Rio de Janeiro, pp 390–397
Casanova-Rosado JF, Medina-Solís CE, Vallejos-Sánchez AA, Casanova-Rosado AJ, Hernández-Prado B, Ávila-Burgos L (2006) Prevalence and associated factors for temporomandibular disorders in a group of Mexican adolescents and youth adults. Clin Oral Investig 10(1):42–49. https://doi.org/10.1007/s00784-005-0021-4
Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F (2011) Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112(4):453–462. https://doi.org/10.1016/j.tripleo.2011.04.021
Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH (1996) Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofac Orthop 109(3):249–262. https://doi.org/10.1016/s0889-5406(96)70148-8
Alrashdan MS, Nuseir A, AL-Omiri MK (2019) Prevalence and correlations of temporomandibular disorders in Northern Jordan using diagnostic criteria axis I. J Investig Clin Dent 10(2):e12390. https://doi.org/10.1111/jicd.12390
Ribeiro RF, Tallents RH, Katzberg RW, Murphy WC, Moss ME, Magalhaes AC, Tavano O (1996) The prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6 to 25 years. J Orofac Pain 11(1):37–47
Larheim TA, Westesson P, Sano T (2001) Temporomandibular joint disk displacement: comparison in asymptomatic volunteers and patients. Radiology 218(2):428–432. https://doi.org/10.1148/radiology.218.2.r01fe11428
Liu F, Steinkeler A (2013) Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin N Am 57(3):465–479. https://doi.org/10.1016/j.cden.2013.04.006
Pupo YM, Quirino Pantoja LL, Veiga FF, Stechman-Neto J, Zwir LF, Farago PV, De Luca CG, Porporatti AL (2016) Diagnostic validity of clinical protocols to assess temporomandibular disk displacement disorders: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 122(5):572–586. https://doi.org/10.1016/j.oooo.2016.07.004
Lobbezoo F, Visscher CM, Naeije M (2010) Some remarks on the RDC/TMD validation project: report of an IADR/Toronto-2008 workshop discussion. J Oral Rehabil 37(10):779–783. https://doi.org/10.1111/j.1365-2842.2010.02091.x
Tuijt M, Parsa A, Koutris M, Berkhout E, Koolstra JH, Lobbezoo F (2018) Human jaw joint hypermobility: diagnosis and biomechanical modelling. J Oral Rehabil 45(10):783–789. https://doi.org/10.1111/joor.12689
Pantoja LLQ, de Toledo IP, Pupo YM, Porporatti AL, De Luca CG, Zwir LF, Guerra ENS (2019) Prevalence of degenerative joint disease of the temporomandibular joint: a systematic review. Clin Oral Investig 23(5):2475–2488. https://doi.org/10.1007/s00784-018-2664-y
Manfredini D, Guarda-Nardini L (2008) Agreement between research diagnostic criteria for temporomandibular disorders and magnetic resonance diagnoses of temporomandibular disc displacement in a patient population. Int J Oral Maxillofac Surg 37(7):612–616. https://doi.org/10.1016/j.ijom.2008.04.003
Christidis N, Ndanshau EL, Sandberg A, Tsilingaridis G (2019) Prevalence and treatment strategies regarding temporomandibular disorders in children and adolescents-a systematic review. J Oral Rehabil 46(3):291–301. https://doi.org/10.1111/joor.12759
Dyrbye LN, Thomas MR, Shanafelt TD (2006) Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med 81(4):354–373. https://doi.org/10.1097/00001888-200604000-00009
Adams DF (2017) The embedded counseling model: an application to dental students. J Dent Educ 81(1):29–35
Lövgren A, Österlund C, Ilgunas A, Lampa E, Hellström F (2018) A high prevalence of TMD is related to somatic awareness and pain intensity among healthy dental students. Acta Odontol Scand 76(6):387–393. https://doi.org/10.1080/00016357.2018.1440322
Durham J, Steele JG, Wassell RW, Exley C (2010) Living with uncertainty: temporomandibular disorders. J Dent Res 89(8):827–830. https://doi.org/10.1177/0022034510368648
Naeije M, te Veldhuis AH, te Veldhuis EC, Visscher CM, Lobbezoo F (2013) Disc displacement within the human temporomandibular joint: a systematic review of a “noisy annoyance.”. J Oral Rehabil 40(2):139–158. https://doi.org/10.1111/joor.12016
Acknowledgments
The authors thank the librarian MSc Maria Gorete Monteguti Savi for the instructions regarding the search strategy of this review and the researchers.
Funding
The authors of this study Lígia Figueiredo Valesan [grant number 88882.437769], Cecília Doebber Da-Cas [grant number 88882.437764] and Ana Cristina Scremin Denardin [grant number 88882.437761] are funded by Coordination for the Improvement of Higher Education Personnel (CAPES), Brasília, DF,Brazil - Finance Code 001.
Author information
Authors and Affiliations
Contributions
The idea for the article was performed by Dr. Beatriz Dulcineia Mendes de Souza, and the design was performed by Dr. Beatriz Dulcineia Mendes de Souza and Lígia Figueiredo Valesan. Material preparation, literature search, data collection, and analysis were performed by Lígia Figueiredo Valesan, Cecília Doebber Da-Cas, Jéssica Conti Réus, and Ana Cristina Scremin Denardin. The first draft of the manuscript was written by Lígia Figueiredo Valesan, and all authors critically reviewed the manuscript. All authors read and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valesan, L.F., Da-Cas, C.D., Réus, J.C. et al. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Invest 25, 441–453 (2021). https://doi.org/10.1007/s00784-020-03710-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03710-w