Abstract
Objectives
The purpose of this retrospective study was to evaluate and compare the effects of fast- and slow-setting calcium silicate–based materials (CSMs) used for root-end filling on the outcome of endodontic microsurgery.
Materials and methods
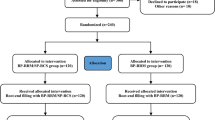
We searched a clinical database for patients who had received endodontic microsurgery between 2001 and 2016. Included cases were divided into two groups according to the type of CSM used for root-end filling: slow-setting CSM (SCSM) and fast-setting CSM (FCSM). The cases in two groups were subjected to 1:1 nearest neighbor propensity score matching for the following variables: age, sex, tooth type, quality of canal filling, lesion type, and postoperative restoration. For each matched case, the outcome was determined as success or failure according to clinical and radiographic evaluations performed at least 1 year after surgery. Multivariate logistic regression analysis was performed to identify prognostic factors and estimate their effects.
Results
In total, 304 cases of endodontic microsurgery (179 SCSM and 125 FCSM) were identified, and 1:1 propensity score matching finally included 122 cases from each group. After matching, all covariates were associated with an absolute standardized difference of < 0.1. The overall success rates were 85.2% and 93.4% for the SCSM and FCSM groups, respectively (p = 0.062). Age, tooth type, lesion type, and CSM type were significantly associated with the outcome of endodontic microsurgery (p < 0.05).
Conclusions
Within the limitations, the outcome of endodontic microsurgery using FCSMs was comparable with that of SCSMs. The findings suggest that the type of CSM used for root-end filling, particularly in terms of the initial setting time, could affect the outcome of endodontic microsurgery.
Clinical relevance
FCSMs could be considered for use as root-end filling materials in endodontic microsurgery, particularly in complicated clinical situations which require rapid initial setting of the materials.

Similar content being viewed by others
References
Parirokh M, Torabinejad M (2010) Mineral trioxide aggregate: a comprehensive literature review—part I: chemical, physical, and antibacterial properties. J Endod 36:16–27
Torabinejad M, Parirokh M (2010) Mineral trioxide aggregate: a comprehensive literature review—part II: leakage and biocompatibility investigations. J Endod 36:190–202
Parirokh M, Torabinejad M (2010) Mineral trioxide aggregate: a comprehensive literature review—part III: clinical applications, drawbacks, and mechanism of action. J Endod 36:400–413
Tsesis I, Rosen E, Taschieri S, Telishevsky Strauss Y, Ceresoli V, Del Fabbro M (2013) Outcomes of surgical endodontic treatment performed by a modern technique: an updated meta-analysis of the literature. J Endod 39:332–339
Montellano AM, Schwartz SA, Beeson TJ (2006) Contamination of tooth-colored mineral trioxide aggregate used as a root-end filling material: a bacterial leakage study. J Endod 32:452–455
Nekoofar MH, Stone DF, Dummer PM (2010) The effect of blood contamination on the compressive strength and surface microstructure of mineral trioxide aggregate. Int Endod J 43:782–791
Nekoofar MH, Oloomi K, Sheykhrezae MS, Tabor R, Stone DF, Dummer PM (2010) An evaluation of the effect of blood and human serum on the surface microhardness and surface microstructure of mineral trioxide aggregate. Int Endod J 43:849–858
Kim Y, Kim S, Shin YS, Jung IY, Lee SJ (2012) Failure of setting of mineral trioxide aggregate in the presence of fetal bovine serum and its prevention. J Endod 38:536–540
Parirokh M, Torabinejad M, Dummer PMH (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview—part I: vital pulp therapy. Int Endod J 51:177–205
Torabinejad M, Parirokh M, Dummer PMH (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview—part II: other clinical applications and complications. Int Endod J 51:284–317
Choi Y, Park SJ, Lee SH, Hwang YC, Yu MK, Min KS (2013) Biological effects and washout resistance of a newly developed fast-setting pozzolan cement. J Endod 39:467–472
Jang GY, Park SJ, Heo SM, Yu MK, Lee KW, Min KS (2013) Washout resistance of fast-setting pozzolan cement under various root canal irrigants. Restor Dent Endod 38:248–252
Souza LC, Yadlapati M, Dorn SO, Silva R, Letra A (2015) Analysis of radiopacity, pH and cytotoxicity of a new bioceramic material. J Appl Oral Sci 23:383–389
Song M, Yue W, Kim S, Kim W, Kim Y, Kim JW, Kim E (2016) The effect of human blood on the setting and surface micro-hardness of calcium silicate cements. Clin Oral Investig 20:1997–2005
Kim SY, Kim HC, Shin SJ, Kim E (2018) Comparison of gap volume after retrofilling using 4 different filling materials: evaluation by micro-computed tomography. J Endod 44:635–638
Jang Y, Song M, Yoo IS, Song Y, Roh BD, Kim E (2015) A randomized controlled study of the use of ProRoot mineral trioxide aggregate and Endocem as direct pulp capping materials: 3-month versus 1-year outcomes. J Endod 41:1201–1206
Kang CM, Sun Y, Song JS, Pang NS, Roh BD, Lee CY, Shin Y (2017) A randomized controlled trial of various MTA materials for partial pulpotomy in permanent teeth. J Dent 60:8–13
Kang CM, Kim SH, Shin Y, Lee HS, Lee JH, Kim GT, Song JS (2015) A randomized controlled trial of ProRoot MTA, OrthoMTA and RetroMTA for pulpotomy in primary molars. Oral Dis 21:785–791
Song M, Kim SG, Lee SJ, Kim B, Kim E (2013) Prognostic factors of clinical outcomes in endodontic microsurgery: a prospective study. J Endod 39:1491–1497
Song M, Jung IY, Lee SJ, Lee CY, Kim E (2011) Prognostic factors for clinical outcomes in endodontic microsurgery: a retrospective study. J Endod 37:927–933
Rud J, Andreasen JO, Jensen JE (1972) Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg 1:195–214
Molven O, Halse A, Grung B (1987) Observer strategy and the radiographic classification of healing after endodontic surgery. Int J Oral Maxillofac Surg 16:432–439
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Zhou W, Zheng Q, Tan X, Song D, Zhang L, Huang D (2017) Comparison of mineral trioxide aggregate and iRoot BP plus root repair material as root-end filling materials in endodontic microsurgery: a prospective randomized controlled study. J Endod 43:1–6
Jang Y, Lee SJ, Yoon TC, Roh BD, Kim E (2016) Survival rate of teeth with a C-shaped canal after intentional replantation: a study of 41 cases for up to 11 years. J Endod 42:1320–1325
Rubinstein RA, Kim S (2002) Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod 28:378–383
Song M, Nam T, Shin SJ, Kim E (2014) Comparison of clinical outcomes of endodontic microsurgery: 1 year versus long-term follow-up. J Endod 40:490–494
Song M, Kang M, Kang DR, Jung HI, Kim E (2018) Comparison of the effect of endodontic-periodontal combined lesion on the outcome of endodontic microsurgery with that of isolated endodontic lesion: survival analysis using propensity score analysis. Clin Oral Investig 22:1717–1724
Wang ZH, Zhang MM, Wang J, Jiang L, Liang YH (2017) Outcomes of endodontic microsurgery using a microscope and mineral trioxide aggregate: a prospective cohort study. J Endod 43:694–698
Kim S, Kratchman S (2006) Modern endodontic surgery concepts and practice: a review. J Endod 32:601–623
Kim S, Jung H, Kim S, Shin SJ, Kim E (2016) The influence of an isthmus on the outcomes of surgically treated molars: a retrospective study. J Endod 42:1029–1034
Giacomino CM, Ray JJ, Wealleans JA (2018) Targeted endodontic microsurgery: a novel approach to anatomically challenging scenarios using 3-dimensional-printed guides and trephine burs-a report of 3 cases. J Endod 44:671–677
Ahn SY, Kim NH, Kim S, Karabucak B, Kim E (2018) Computer-aided design/computer-aided manufacturing-guided endodontic surgery: guided osteotomy and apex localization in a mandibular molar with a thick buccal bone plate. J Endod 44:665–670
Chang SW, Bae WJ, Yi JK, Lee S, Lee DW, Kum KY, Kim EC (2015) Odontoblastic differentiation, inflammatory response, and angiogenic potential of 4 calcium silicate-based cements: micromega MTA, ProRoot MTA, RetroMTA, and experimental calcium silicate cement. J Endod 41:1524–1529
Funding
This study was funded by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2018R1D1A1A09081906).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Approval for this project was obtained from the Yonsei University Committee for Research on Human Subjects (2004-4).
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, D., Lee, H., Chung, M. et al. Effects of fast- and slow-setting calcium silicate–based root-end filling materials on the outcome of endodontic microsurgery: a retrospective study up to 6 years. Clin Oral Invest 24, 247–255 (2020). https://doi.org/10.1007/s00784-019-02937-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02937-6