Abstract
Objective
This prospective randomized clinical trial was conducted to determine whether the application of a platelet-rich fibrin (PRF) palatal bandage after harvesting free gingival grafts (FGG) would improve healing of donor sites and decrease pain scores and patient discomfort.
Materials and methods
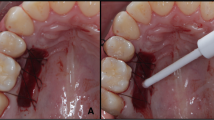
Twenty-four patients received FGG to augment keratinized tissue dimensions. The application of a PRF bandage was decided randomly (n = 12 in each group). Patients reported their pain levels for the first 7 days of healing using the visual analog scale (VAS), 101-point numerical rating scale (NRS-101), and 4-point verbal rating scale (VRS-4). The patients’ pre-operative anxiety levels were measured using three anxiety scales. The healing of the donor sites was evaluated and compared to preoperative records. Data were assessed and recorded before surgery and at 1, 2, 3, 4, and 8 weeks postoperatively.
Results
Dental anxiety and state-trait anxiety were evaluated at baseline and correlated to the postoperative pain scores. There were no significant differences in anxiety levels between the two groups; yet, they could potentially influence the outcome of any surgery and were included as covariates. The patients in the PRF group reported significantly lower pain scores and their pain levels returned to baseline levels earlier, compared to the control group.
Conclusions
PRF palatal bandages significantly reduced postoperative pain and discomfort and facilitated wound healing after harvesting FGG.
Clinical relevance
The study provided evaluation of patient-centered outcomes, which is timely, significant, and could benefit both periodontists and patients.





Similar content being viewed by others
References
Del Pizzo M, Modica F, Bethaz N, Priotto P, Romagnoli R (2002) The connective tissue graft: a comparative clinical evaluation of wound healing at the palatal donor site. J Clin Periodontol 29:848–854
Wessel JR, Tatakis DN (2008) Patient outcomes following subepithelial connective tissue graft and free gingival graft procedures. J Periodontol 79:425–430
Silva CO, Ribeiro EDP, Sallum AW, Tatakis DN (2010) Free gingival grafts: graft shrinkage and donor-site healing in smokers and non-smokers. J Periodontol 81:692–701
Tomar N, Singh R, Jain G, Kaushik M, Dureja D (2016) Enhancement of healing of donor hard palate site using platelet-rich fibrin. J Curr Res Sci Med 2:132
Choukroun J, Adda F, Schoeffer C, Vervelle A (2001) PRF: an opportunity in perio-implantology (in French). Implantodontie 42:55–62
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 101:e56–e60
Dohan Ehrenfest DM, Del Corso M, Diss A, Mouhyi J, Charrier JB (2010) Three-dimensional architecture and cell composition of a Choukroun’s platelet-rich fibrin clot and membrane. J Periodontol 81:546–555
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 101:e45-e50
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e51–e55
Dohan Ehrenfest DM, de Peppo P, Doglioli, Sammartino G (2009) Slow release of growth factors and thrombospondin-1 in Choukroun’s platelet-rich fibrin (PRF): a gold standard to achieve for all surgical platelet concentrates technologies. Growth Factors 27:63–69
Gamal AY, Abdel Ghaffar KA, Alghezwy OA (2016) Crevicular fluid growth factors release profile following the use of platelet-rich fibrin and plasma rich growth factors in treating periodontal intrabony defects: a randomized clinical trial. J Periodontol 87:654–662
Jain V, Triveni MG, Kumar AT, Mehta DS (2012) Role of platelet-rich-fibrin in enhancing palatal wound healing after free graft. Contemp Clin Dent 3:S240
Sclafani AP (2009) Applications of platelet-rich fibrin matrix in facial plastic surgery. Facial Plastic Surgery 25:270–276
Mazor Z, Horowitz RA, Del Corso M, Prasad HS, Rohrer MD, Dohan Ehrenfest DM (2009) Sinus floor augmentation with simultaneous implant placement using Choukroun’s platelet-rich fibrin as the sole grafting material: a radiologic and histologic study at 6 months. J Periodontol 80:2056–2064
Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D (2009) Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: a 6-month study. J Periodontol 80:244–252
Ghanaati S, Booms P, Orlowska A (2014) Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol 40:679–689
Schulz KF, Altman Moher DG (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med 7:e1000251
World Medical Association Inc (2016) WMA declaration of Helsinki - ethical principles for medical research involving human subjects. Access date: February 2016; Available from: http://www.wma.net/en/30publications/10policies/b3/
Bahammam MA (2016) Validity and reliability of an Arabic version of the state-trait anxiety inventory in a Saudi dental setting. Saudi Med J 37:668–674
Spielberger CD, Gorsuch RL, Lushene RE (1970) Manual for the state-trait anxiety inventory
Bahammam MA, Hassan MH (2014) Validity and reliability of an Arabic version of the modified dental anxiety scale in Saudi adults. Saudi Med J 35:1384–1389
Humphris Morrison GMT, Lindsay SJ (1995) The modified dental anxiety scale: validation and United Kingdom norms. Community Dent Health 12:143–150
Sullivan HC (1968) Free autogenous gingival grafts. I. Principles of successful grafting. Periodontics 6:121–129
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 101:e37–e44
Houde RW (1982) Methods for measuring clinical pain in humans. Acta Anaesthesiol Scand 74:25–29
Jensen MP, Karoly P, Braver S (1986) The measurement of clinical pain intensity: a comparison of six methods. Pain 27:117–126
Dohan Ehrenfest DM, Rasmusson L, Albrektsson T (2009) Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol 27:158–167
Chang YC, Zhao JH (2011) Effects of platelet-rich fibrin on human periodontal ligament fibroblasts and application for periodontal infrabony defects. Aust Dent J 56:365–371
Naik B, Karunakar P, Jayadev M, Marshal VR (2013) Role of platelet rich fibrin in wound healing: a critical review. J Conserv Dent 16:284–293
Del Corso M, Vervelle A, Simonpieri A et al (2012) Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: periodontal and dentoalveolar surgery. Curr Pharm Biotechnol 13:1207–1230
He L, Lin Y, Hu X, Zhang Y, Wu H A comparative study of platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) on the effect of proliferation and differentiation of rat osteoblasts in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:707–713
Soileau KM, Brannon RB (2006) A histologic evaluation of various stages of palatal healing following subepithelial connective tissue grafting procedures: a comparison of eight cases. J Periodontol 77:1267–1273
Yen CA, Griffin TJ, Cheung WS, Chen J (2007) Effects of platelet concentrate on palatal wound healing after connective tissue graft harvesting. J Periodontol 78:601–610
Farnoush A (1978) Techniques for the protection and coverage of the donor sites in free soft tissue grafts. J Periodontol 49:403–405
Bahammam MA, Linjawi AI (2014) Knowledge, attitude, and barriers towards the use of evidence based practice among senior dental and medical students in western Saudi Arabia. Saudi Med J 35:1250–1256
Malvania EA, Ajithkrishnan CG (2011) Prevalence and socio-demographic correlates of dental anxiety among a group of adult patients attending a dental institution in Vadodara city, Gujarat, India. Indian J Dent Res 22:179–180
Anilkumar K, Geetha A, Umasudhakar TR, Vijayalakshmi R, Pameela E (2009) Platelet-rich-fibrin: a novel root coverage approach. J Indian Soc Periodontol 13:50–54
Femminella B, Iaconi MC, Di Tullio M (2016) Clinical comparison of platelet-rich fibrin and a gelatin sponge in the management of palatal wounds after epithelialized free gingival graft harvest: a randomized clinical trial. J Periodontol 87:103–113
Choukroun J, Ghanaati S (2017) Reduction of relative centrifugation force within injectable platelet-rich-fibrin (PRF) concentrates advances patients’ own inflammatory cells, platelets and growth factors: the first introduction to the low speed centrifugation concept. Eur J Trauma Emerg Surg
Acknowledgments
Maha A. Bahammam would like to thank the deanship of Scientific Research for technical and financial support. I also want to thank Dr. Eman Y. Elfirt at faculty of dentistry, King Abdulaziz University for conducting the post-surgical care during the follow-up visits.
Funding
This study was funesentative clinical esentative clinical esentative clinical anship of Scientific Research (DSR), King Abdulaziz University, Jeddah, Kingdom of Saudi Arabia (Grant No. 285-254-1434).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the King Abdulaziz University ethical committee, was carried out in accordance with the tenets of the Declaration of Helsinki [17, 18], and was registered at clinicaltrials.gov with the registration number NCT02797899.
Conflict of interest
Maha A. Bahammam declares that she has no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care of human beings were followed.
Informed consent
For this type of study, formal consent is not required.
Electronic supplementary material
ESM 1
(DOC 217 kb)
Rights and permissions
About this article
Cite this article
Bahammam, M.A. Effect of platelet-rich fibrin palatal bandage on pain scores and wound healing after free gingival graft: a randomized controlled clinical trial. Clin Oral Invest 22, 3179–3188 (2018). https://doi.org/10.1007/s00784-018-2397-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2397-y