Abstract
Objective
The objective of this study was to develop a simple tool for the assessment of possible dental treatment needs (DTN) for non-dental professionals (Mini Dental Assessment, MDA). To keep the assessment universal, we aimed to base it on the patient’s history and a simple chewing efficiency test (CET) as the dental status is a known determinant for chewing efficiency.
Materials & methods
The assessment was developed using data from 169 patients from two sites (University Hospital Giessen, St. Bonifatius Hospital Lingen, both Germany). In all patients, a dental examination was performed, the denture status was evaluated (based on the California Dental Association criteria; CDA criteria), and the DTN was determined. In addition, the time since the patient’s last visit to a dentist (TLVD) and denture age (DA) were assessed. Furthermore, a CET was carried out and the comminution score was determined (CETS).
Results
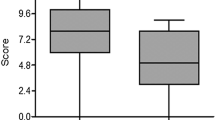
In total, 108 patients required dental treatment. The mean value (±SD) was 2.9 ± 0.9 score points for the DTN, 2.5 ± 3.8 years for the TLVD, and 10.8 ± 8.9 years for the DA. There was a significant correlation (Spearman, P < .05) between the DTN and degree of comminution (3.4 ± 1.8). Based on the results of the statistical analysis, the intended assessment tool was developed using the variables CETS, TLVD, and DA weighed by their respective regression coefficients (10:3:1). Subsequently, the resulting MDA score (51.32 ± 28.14) was calculated. A sensitivity/specificity analysis was conducted and a receiver operating characteristic curve was calculated (SPSS 17.0, area under curve 0.805; 95 % CI 0.738–0.873).
Conclusion
It can be concluded that the dental status of elderly patients is reflected in the outcome of the MDA. However, ongoing validation is needed.
Trial registration
DRKS00003219.



Similar content being viewed by others
References
Brodeur JM, Laurin D, Vallee R, Lachapelle D (1993) Nutrient intake and gastrointestinal disorders related to masticatory performance in the edentulous elderly. J Prosthet Dent 70(5):468–473
Chauncey HH, Muench ME, Kapur KK, Wayler AH (1984) The effect of the loss of teeth on diet and nutrition. Int Dent J 34(2):98–104
Dormenval V, Mojon P, Budtz-Jorgensen E (1999) Associations between self-assessed masticatory ability, nutritional status, prosthetic status and salivary flow rate in hospitalized elders. Oral Dis 5(1):32–38
Mojon P, Budtz-Jorgensen E, Rapin CH (1999) Relationship between oral health and nutrition in very old people. Age Ageing 28(5):463–468
Sahyoun NR, Krall E (2003) Low dietary quality among older adults with self-perceived ill-fitting dentures. J Am Diet Assoc 103(11):1494–1499
Sheiham A, Steele JG, Marcenes W, Lowe C, Finch S, Bates CJ, Prentice A, Walls AW (2001) The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res 80(2):408–413
Soini H, Routasalo P, Lauri S, Ainamo A (2003) Oral and nutritional status in frail elderly. Spec Care Dentist 23(6):209–215
Nitschke I, Majdani M, Sobotta BA, Reiber T, Hopfenmuller W (2010) Dental care of frail older people and those caring for them. J Clin Nurs 19(13–14):1882–1890
Lindqvist L, Seleskog B, Wardh I, von Bultzingslowen I (2013) Oral care perspectives of professionals in nursing homes for the elderly. Int J Dent Hyg 11(4):298–305
Mojon P, MacEntee MI (1992) Discrepancy between need for prosthodontic treatment and complaints in an elderly edentulous population. Community Dent Oral Epidemiol 20(1):48–52
Guigoz Y, Vellas BJ (1997) Malnutrition in the elderly: the mini nutritional assessment (MNA). Ther Umsch 54(6):345–350
Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Bush LA, Horenkamp N, Morley JE, Spiro A 3rd (1996) D-E-N-T-A-L: a rapid self-administered screening instrument to promote referrals for further evaluation in older adults. J Am Geriatr Soc 44(8):979–981
Slade GD, Spencer AJ (1994) Development and evaluation of the oral health impact profile. Community Dent Health 11(1):3–11
Leao A, Sheiham A (1996) The development of a socio-dental measure of dental impacts on daily living. Community Dent Health 13(1):22–26
Schimmel M, Christou P, Herrmann F, Muller F (2007) A two-colour chewing gum test for masticatory efficiency: development of different assessment methods. J Oral Rehabil 34(9):671–678
Atchison KA, Dolan TA (1990) Development of the geriatric oral health assessment index. J Dent Educ 54(11):680–687
Manly RS, Braley LC (1950) Masticatory performance and efficiency. J Dent Res 29(4):448–462
van der Bilt A, Fontijn-Tekamp FA (2004) Comparison of single and multiple sieve methods for the determination of masticatory performance. Arch Oral Biol 49(3):193–198
Nowjack-Raymer RE, Sheiham A (2007) Numbers of natural teeth, diet, and nutritional status in US adults. J Dent Res 86(12):1171–1175
Osterberg T, Tsuga K, Rothenberg E, Carlsson GE, Steen B (2002) Masticatory ability in 80-year-old subjects and its relation to intake of energy, nutrients and food items. Gerodontology 19(2):95–101
Tatematsu M, Mori T, Kawaguchi T, Takeuchi K, Hattori M, Morita I, Nakagaki H, Kato K, Murakami T, Tuboi S, Hayashizaki J, Murakami H, Yamamoto M, Ito Y (2004) Masticatory performance in 80-year-old individuals. Gerodontology 21(2):112–119
Wöstmann B, Michel K, Brinkert B, Melchheier-Weskott A, Rehmann P, Balkenhol M (2008) Influence of denture improvement on the nutritional status and quality of life of geriatric patients. J Dent 36(10):816–821
Wilkins CH, Roe CM, Morris JC (2010) A brief clinical tool to assess physical function: the mini-physical performance test. Arch Gerontol Geriatr 50(1):96–100
Tanaka M, Yamamoto H, Kita T, Yokode M (2008) Early prediction of the need for non-routine discharge planning for the elderly. Arch Gerontol Geriatr 47(1):1–7
Romero-Ortuno R (2013) The frailty instrument for primary care of the survey of health, ageing and retirement in Europe predicts mortality similarly to a frailty index based on comprehensive geriatric assessment. Geriatr Gerontol Int 13(2):497–504
O’Connor MN, Gallagher P, Byrne S, O’Mahony D (2012) Adverse drug reactions in older patients during hospitalisation: are they predictable? Age Ageing 41(6):771–776
Quality evaluation for dental care: guidelines for the assessment of clinical quality and professional performance (1977). Los Angeles: CDA
Ryge G, Snyder M (1973) Evaluating the clinical quality of restorations. J Am Dent Assoc 87(2):369–377
Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW (2002) The relationship between oral health status and body mass index among older people: a national survey of older people in Great Britain. Br Dent J 192(12):703–706
Wöstmann B, Brinkert B, Melchheier-Weskott A, Zenginel M, Rehmann P (2011) Chewing efficiency screening test for non-dental-professionals. J Dent Res 90 (Spec Iss A) 1598 (www.iadr.org)
Petersen PE, Kandelman D, Arpin S, Ogawa H (2010) Global oral health of older people—call for public health action. Community Dent Health 27(4 Suppl 2):257–267
Chu KY, Yang NP, Chou P, Chi LY, Chiu HJ (2013) Dental prosthetic treatment needs of inpatients with schizophrenia in Taiwan: a cross-sectional study. BMC Oral Health 13:8
Nguyen C (2001) Auswirkung der Qualität des Zahnersatzes und der Kaueffizienz auf den Ernährungszustand geriatrischer Patienten und die Entwicklung eines Kaufunktionstests. Justus-Liebig-University, Giessen
Stone AA, Schwartz JE, Broderick JE, Deaton A (2010) A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci U S A 107(22):9985–9990
Rehmann P, Orbach K, Ferger P, Wöstmann B (2013) Treatment outcomes with removable partial dentures: a retrospective analysis. Int J Prosthodont 26(2):147–150
Akeel R, Nilner M, Nilner K (1992) Masticatory efficiency in individuals with natural dentition. Swed Dent J 16(5):191–198
Pera P, Bucca C, Borro P, Bernocco C, De LA, Carossa S (2002) Influence of mastication on gastric emptying. J Dent Res 81(3):179–181
Mowlana F, Heath MR, Van der Bilt A, Van der Glas HW (1994) Assessment of chewing efficiency: a comparison of particle size distribution determined using optical scanning and sieving of almonds. J Oral Rehabil 21(5):545–551
Sato S, Fueki K, Sato H, Sueda S, Shiozaki T, Kato M, Ohyama T (2003) Validity and reliability of a newly developed method for evaluating masticatory function using discriminant analysis. J Oral Rehabil 30(2):146–151
Acknowledgments
We gratefully acknowledge the kind support from Dr. J. Herrmann and Dr. J. Riehl for the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The authors did not receive any external funding; the study is solely based on the departmental budgets of the authors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The authors confirm that all related trials for this intervention are registered.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wöstmann, B., Seelbach, M., Seelbach, P. et al. Mini dental assessment: a simple screening test for non-dental staff. Clin Oral Invest 21, 1457–1464 (2017). https://doi.org/10.1007/s00784-016-1906-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1906-0