Abstract
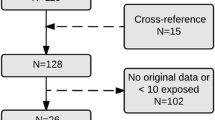
Aripiprazole has become one of the most commonly prescribed psychotropics, making a more comprehensive understanding of its reproductive safety profile a priority. The goal of the current analysis was to determine the risk of major malformations in infants exposed during the first trimester of pregnancy to aripiprazole compared to infants whose mothers had psychiatric diagnoses but did not use an atypical antipsychotic during pregnancy. The National Pregnancy Registry for Atypical Antipsychotics is a prospective pharmacovigilance program in which pregnant women are enrolled and interviewed during pregnancy and the postpartum period. Medical records are assessed to confirm presence or absence of major malformations. Pregnant women ages 18–45 with psychiatric diagnoses are enrolled. As of April 2020, N = 848 women who had delivered infants were eligible for analyses. A total of 158 women with first trimester exposure to aripiprazole were compared to 690 controls. For 163 infants born to women in the exposed group, seven major malformations were confirmed (4.29%), compared to fourteen of the 690 unexposed infants (1.99%). The unadjusted odds ratio for major malformations between aripiprazole-exposed and unexposed infants was 2.21 (95% confidence interval [CI] = (0.88, 5.57) The adjusted odds ratio for major malformations was 1.35 (95% confidence interval [CI] = (0.43, 4.20). After adjustment for confounding variables, the risk of major malformations after first trimester exposure to aripiprazole was not significant compared to controls. While these results are reassuring, they are limited by relatively small numbers of participants. Future analyses with larger numbers are expected to provide more of a complete and precise reproductive safety profile regarding aripiprazole use during pregnancy. Trial registration: clinicaltrials.gov NCT01246765


Similar content being viewed by others
Data availability
Data is not available. The data that has been used is confidential.
Change history
22 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00737-021-01133-4
References
Bellet F, Beyens MN, Bernard N, Beghin D, Elefant E, Vial T (2015) Exposure to aripiprazole during embryogenesis: a prospective multicenter cohort study. Pharmacoepidemiol Drug Saf 24(4):368–380
Centers for Disease Control and Prevention (CDC) (2008) Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978–2005. MMWR Morb Mortal Wkly Rep 57(1):1–5
Citrome L, Kalsekar I, Guo Z, Laubmeier K, Hebden T (2013) Diagnoses associated with use of atypical antipsychotics in a commercial health plan: a claims database analysis. Clin Ther 35(12):1867–1875
Cohen L (2015) Establishment of the National Pregnancy Registry for Atypical Antipsychotics. J Clin Psychiatry 76:986–989
Cohen LS, Viguera AC, McInerney KA, et al (2015) Reproductive safety of second-generation antipsychotics: current data from the Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. Am J Psychiatry. appiajp201515040506
Coughlin CG, Blackwell KA, Bartley C, Hay M, Yonkers KA, Bloch MH (2015) Obstetric and neonatal outcomes after antipsychotic medication exposure in pregnancy. Obstet Gynecol 125(5):1224–1235
Cuomo A, Goracci A, Fagiolini A (2018) Aripiprazole use during pregnancy, peripartum and lactation. A systematic literature search and review to inform clinical practice. J Affect Disord 228:229–237
Damkier P, Videbech P (2018) The safety of second-generation antipsychotics during pregnancy: a clinically focused review. CNS Drugs 32:351–366
Einarson A, Boskovic R (2009) Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract 15(3):183–192
Ennis ZN, Damkier P (2015) Pregnancy exposure to olanzapine, quetiapine, risperidone, aripiprazole and risk of congenital malformations. A systematic review. Basic Clin Pharmacol Toxicol 116(4):315–320
Food and Drug Administration HHS (2014) Content and format of labeling for human prescription drug and biological products; requirements for pregnancy and lactation labeling. Final rule. Fed Regist 79(233):72063
Gjerden P, Bramness JG, Tvete IF, Slordal L (2017) The antipsychotic agent quetiapine is increasingly not used as such: dispensed prescriptions in Norway 2004-2015. Eur J Clin Pharmacol 73(9):1173–1179
Habermann F, Fritzsche J, Fuhlbruck F et al (2013) Atypical antipsychotic drugs and pregnancy outcome: a prospective, cohort study. J Clin Psychopharmacol 33(4):453–462
Halfdanarson O, Zoega H, Aagaard L, et al (2017) International trends in antipsychotic use: a study in 16 countries, 2005-2014. Eur Neuropsychopharmacol
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Huybrechts KF, Hernandez-Diaz S, Patorno E et al (2016) Antipsychotic use in pregnancy and the risk for congenital malformations. JAMA Psychiatry 73(9):938–946
Insel TR, Fenton WS (2005) Psychiatric epidemiology: it’s not just about counting anymore. Arch Gen Psychiatry 62(6):590–592
Kessler RC, Chiu WT, Demler O, Walters EE (2005) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62(6):617–627
Kulkarni J, Worsley R, Gilbert H, Gavrilidis E, van Rheenen TE, Wang W, McCauley K, Fitzgerald P (2014) A prospective cohort study of antipsychotic medications in pregnancy: the first 147 pregnancies and 100 one year old babies. PLoS One 9(5):e94788–e94788
L’Italien GJ, Casey DE, Kan HJ, Carson WH, Marcus RN (2007) Comparison of metabolic syndrome incidence among schizophrenia patients treated with aripiprazole versus olanzapine or placebo. J Clin Psychiatry. 68(10):1510–1516
Maglione M, Maher AR, Hu J, et al (2011) Off-label use of atypical antipsychotics: an update
McKenna K, Koren G, Tetelbaum M, Wilton L, Shakir S, Diav-Citrin O, Levinson A, Zipursky RB, Einarson A (2005) Pregnancy outcome of women using atypical antipsychotic drugs: a prospective comparative study. J Clin Psychiatry. 66(4):444–449
Park Y, Huybrechts KF, Cohen JM, et al (2017) Antipsychotic medication use among publicly insured pregnant women in the United States. Psychiatr Serv appips201600408
Paulus W (2013) Is the use of aripiprazole safe during first trimester of pregnancy? Reprod Toxicol 37:87
Pringsheim T, Gardner DM (2014) Dispensed prescriptions for quetiapine and other second-generation antipsychotics in Canada from 2005 to 2012: a descriptive study. CMAJ Open 2(4):E225–E232
Tosato S, Albert U, Tomassi S, Iasevoli F, Carmassi C, Ferrari S, Nanni MG, Nivoli A, Volpe U, Atti AR, Fiorillo A (2017) A systematized review of atypical antipsychotics in pregnant women: balancing between risks of untreated illness and risks of drug-related adverse effects. J Clin Psychiatry 78(5):e477–e489
Viguera AC, Nonacs R, Cohen LS, Tondo L, Murray A, Baldessarini RJ (2000) Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry 157(2):179–184
Viguera AC, Whitfield T, Baldessarini RJ et al (2007) Risk of recurrence in women with bipolar disorder during pregnancy: prospective study of mood stabilizer discontinuation. Am J Psychiatry 164(12):1817–1824 quiz 1923
Acknowledgements
We thank and recognize Peter Gaccione, MA, for his contributions to data management and for his statistical programing for the National Pregnancy Registry.
Code availability
Code is not available. The code and data that have been used are confidential.
Funding
Current Sponsors of the NPRAA: Alkermes, Inc. (2016–present); Johnson and Johnson/Jannsen Pharmaceuticals, Inc. (2019–present) Janssen Pharmaceutica (2019–present); Otsuka America Pharmaceutical, Inc. (2008–present); Sunovion Pharmaceuticals, Inc. (2011–present); SAGE Therapeutics (2019–present); Teva Pharmaceuticals (2018–present); Aurobindo Pharma (2020–present); Past Sponsors of the NPRAA: Forest/Actavis Pharmaceuticals (2016–2018) AstraZeneca Pharmaceuticals (2009–2014, declined to sponsor: 2014–present); Ortho-McNeil-Janssen Pharmaceuticals, Inc. (2009–2014, declined to sponsor: 2015–present); Pfizer, Inc. (2009–2011, declined to sponsor: 2012–present).
Author information
Authors and Affiliations
Contributions
All authors contributed to this manuscript. Doctors Lee Cohen, Adele Viguera, and Marlene Freeman designed the study. Dr. Sonia Hernández-Díaz guided statistical analysis. Dr. Lina Góez-Mogollón designed the statistical code used for data analysis. Dr. David Chitayat is the blinded dysmorphologist for determining major malformations. The following authors were responsible for recruiting participants, guiding implementation, and collecting data from participants and hospitals: Phoebe Caplin, Taylor Church, Sara McElheny, and Amanda Young.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the institutional review board of Massachusetts General Brigham (IRB reference # 2008P001861).
For all participants, informed consent was obtained prior to data collection. Consent was obtained using Massachusetts Brigham IRB approved materials.
Consent for publication
All authors agree to publish the manuscript in the Archives of Women’s Mental Health.
Conflict of interest
LSC: National Pregnancy Registry for Atypical Antipsychotics: Alkermes Biopharmaceuticals; Aurobindo Pharma; Janssen Pharmaceutica; Otsuka Pharmaceuticals; Sunovion Pharmaceuticals, Inc.; Teva Pharmaceuticals; Sage Therapeutics, Inc. Other Research Support: Brain & Behavior Research Foundation; JayMac Pharmaceuticals; National Institute on Aging; National Institutes of Health; National Institute of Mental Health; SAGE Therapeutics; Takeda/Lundbeck Pharmaceuticals Advisory/Consulting: Alkermes Biopharmaceuticals (through MGH Clinical Trials Network Initiative); JDS Therapeutics LLC; Praxis Precision Medicines, Inc. (through MGH Clinical Trials Network Initiative) Honoraria: None Royalty/patent, other income: None.
ACV: Research Support: National Pregnancy Registry for Atypical Antipsychotics: Alkermes Biopharmaceuticals; Aurobindo Pharma; Janssen Pharmaceutica; Otsuka Pharmaceuticals;Sunovion Pharmaceuticals, Inc.; Teva Pharmaceuticals; Sage Therapeutics, Inc. Other Research Support: None; Advisory/Consulting: Up-to-Date; Speaking/Honoraria: None;Royalty/patent, other income: None.
MPF: National Pregnancy Registry for Atypical Antipsychotics: Alkermes Biopharmaceuticals; Aurobindo Pharma; Janssen Pharmaceutica; Otsuka Pharmaceuticals; Sunovion Pharmaceuticals, Inc.; Teva Pharmaceuticals; Sage Therapeutics, Inc. Other research support: JayMac Pharmaceuticals LLC, SAGE Therapeutics; As an employee of MGH, Dr. Freeman works with the MGH CTNI, which has had research funding from multiple pharmaceutical companies and NIMH. Advisory/Consulting: Advisory Boards: Eliem, Sage; Independent Data Safety and Monitoring Committee: Janssen (Johnson& Johnson), Novartis; Steering Committee for Educational Activities: Medscape; educational activities: WebMD. Speaking/Honoraria: None; Royalty/patent, other income: None.
SHD: Consulting fees (e.g. advisory boards): Roche and UCB, and her institution received funding from Takeda for unrelated project; epidemiologist for the North American Antiepileptic Drugs pregnancy registry and advisor for the Antipsychotics Pregnancy Registry, which are funded by multiple companies; The Pharmacoepidemiology Program at the Harvard T.H. Chan School of Public Health is partially supported by training grants from Pfizer, UCB, Bayer and Asisa.
LGM, AZS, SAM, TRC, AVY, PSC, DC: Nothing to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Figures 1 and 2 must be switched.
Rights and permissions
About this article
Cite this article
Freeman, M.P., Viguera, A.C., Góez-Mogollón, L. et al. Reproductive safety of aripiprazole: data from the Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. Arch Womens Ment Health 24, 659–667 (2021). https://doi.org/10.1007/s00737-021-01115-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-021-01115-6