Abstract
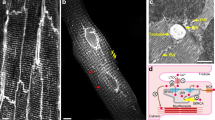
The couplons of the cardiomyocyte form nanospaces within the cell that place the L-type calcium channel (Cav1.2), situated on the plasmalemma, in opposition to the type 2 ryanodine receptor (RyR2), situated on the sarcoplasmic reticulum. These two molecules, which form the basis of excitation–contraction coupling, are separated by a very limited space, which allows a few Ca2+ ions passing through Cav1.2 to activate the RyR2 at concentration levels that would be deleterious to the whole cell. The limited space also allows Ca2+ inactivation of Cav1.2. We have found that not all couplons are the same and that their properties are likely determined by their molecular partners which, in turn, determine their excitability. In particular, there are a class of couplons that lie outside the RyR2-Cav1.2 dyad; in this case, the RyR2 is close to caveolin-3 rather than Cav1.2. These extra-dyadic couplons are probably controlled by the multitude of molecules associated with caveolin-3 and may modulate contractile force under situations such as stress. It has long been assumed that like the skeletal muscle, the RyR2 in the couplon are arranged in a structured array with the RyR2 interacting with each other via domain 6 of the RyR2 molecule. This arrangement was thought to provide local control of RyR2 excitability. Using 3D electron tomography of the couplon, we show that the RyR2 in the couplon do not form an ordered pattern, but are scattered throughout it. Relatively few are in a checkerboard pattern—many RyR2 sit edge-to-edge, a configuration which might preclude their controlling each other's excitability. The discovery of this structure makes many models of cardiac couplon function moot and is a current avenue of further research



Similar content being viewed by others
References
Adachi-Akahane S, Cleemann L, Morad M (1996) Cross-signaling between L-type Ca2+ channels and ryanodine receptors in rat ventricular myocytes. J Gen Physiol 108(5):435–454
Asghari P, Schulson M, Scriven DR, Martens G, Moore ED (2009) Axial tubules of rat ventricular myocytes form multiple junctions with the sarcoplasmic reticulum. Biophys J 96(11):4651–4660
Baddeley D, Jayasinghe ID, Lam L, Rossberger S, Cannell MB, Soeller C (2009) Optical single-channel resolution imaging of the ryanodine receptor distribution in rat cardiac myocytes. Proc Natl Acad Sci USA 106(52):22275–22280
Brochet DX, Yang D, Di Maio A, Lederer WJ, Franzini-Armstrong C, Cheng H (2005) Ca2+ blinks: rapid nanoscopic store calcium signaling. Proc Natl Acad Sci USA 102(8):3099–3104
Brochet DX, Xie W, Yang D, Cheng H, Lederer WJ (2011) Quarky calcium release in the heart. Circ Res 108(2):210–218
Cannell MB, Cheng H, Lederer WJ (1994) Spatial non-uniformities in [Ca2+]i during excitation-contraction coupling in cardiac myocytes. Biophys J 67(5):1942–1956
Cannell MB, Cheng H, Lederer WJ (1995) The control of calcium release in heart muscle. Science 268(5213):1045–1049
Carl SL, Felix K, Caswell AH, Brandt NR, Ball WJ Jr, Vaghy PL, Meissner G, Ferguson DG (1995) Immunolocalization of sarcolemmal dihydropyridine receptor and sarcoplasmic reticular triadin and ryanodine receptor in rabbit ventricle and atrium. J Cell Biol 129(3):672–682
Champion HC, Georgakopoulos D, Takimoto E, Isoda T, Wang Y, Kass DA (2004) Modulation of in vivo cardiac function by myocyte-specific nitric oxide synthase-3. Circ Res 94(5):657–663
Cheng H, Lederer WJ, Cannell MB (1993) Calcium sparks: elementary events underlying excitation–contraction coupling in heart muscle. Science 262(5134):740–744
Cheng H, Cannell MB, Lederer WJ (1995) Partial inhibition of Ca2+ current by methoxyverapamil (D600) reveals spatial nonuniformities in [Ca2+]i during excitation–contraction coupling in cardiac myocytes. Circ Res 76(2):236–241
Cheng H, Lederer MR, Lederer WJ, Cannell MB (1996) Calcium sparks and [Ca2+]i waves in cardiac myocytes. Am J Physiol 270(1 Pt 1):C148–C159
Chopra N, Yang T, Asghari P, Moore ED, Huke S, Akin B, Cattolica RA, Perez CF, Hlaing T, Knollmann-Ritschel BE, Jones LR, Pessah IN, Allen PD, Franzini-Armstrong C, Knollmann BC (2009) Ablation of triadin causes loss of cardiac Ca2+ release units, impaired excitation–contraction coupling, and cardiac arrhythmias. Proc Natl Acad Sci USA 106(18):7636–7641
Fabiato A (1983) Calcium-induced release of calcium from the cardiac sarcoplasmic reticulum. Am J Physiol 245(1):C1–C14
Fabiato A (1985) Time and calcium dependence of activation and inactivation of calcium-induced release of calcium from the sarcoplasmic reticulum of a skinned canine cardiac Purkinje cell. J Gen Physiol 85(2):247–289
Ferguson DG, Schwartz HW, Franzini-Armstrong C (1984) Subunit structure of junctional feet in triads of skeletal muscle: a freeze-drying, rotary-shadowing study. J Cell Biol 99(5):1735–1742
Franzini-Armstrong C, Protasi F, Ramesh V (1999) Shape, size, and distribution of Ca2+ release units and couplons in skeletal and cardiac muscles. Biophys J 77(3):1528–1539
Gomez AM, Valdivia HH, Cheng H, Lederer MR, Santana LF, Cannell MB, McCune SA, Altschuld RA, Lederer WJ (1997) Defective excitation–contraction coupling in experimental cardiac hypertrophy and heart failure. Science 276(5313):800–806
Gyorke I, Gyorke S (1998) Regulation of the cardiac ryanodine receptor channel by luminal Ca2+ involves luminal Ca2+ sensing sites. Biophys J 75(6):2801–2810
Hayashi T, Martone ME, Yu Z, Thor A, Doi M, Holst MJ, Ellisman MH, Hoshijima M (2009) Three-dimensional electron microscopy reveals new details of membrane systems for Ca2+ signaling in the heart. J Cell Sci 122(Pt 7):1005–1013
Larbig R, Torres N, Bridge JH, Goldhaber JI, Philipson KD (2010) Activation of reverse Na+–Ca2+ exchange by the Na+ current augments the cardiac Ca2+ transient: evidence from NCX knockout mice. J Physiol 588(Pt 17):3267–3276
Laver DR, Honen BN (2008) Luminal Mg2+, a key factor controlling RYR2-mediated Ca2+ release: cytoplasmic and luminal regulation modeled in a tetrameric channel. J Gen Physiol 132(4):429–446
Lopez-Lopez JR, Shacklock PS, Balke CW, Wier WG (1994) Local, stochastic release of Ca2+ in voltage-clamped rat heart cells: visualization with confocal microscopy. J Physiol 480(Pt 1):21–29
Mackenzie L, Bootman MD, Berridge MJ, Lipp P (2001) Predetermined recruitment of calcium release sites underlies excitation–contraction coupling in rat atrial myocytes. J Physiol 530(Pt 3):417–429
Marx SO, Ondrias K, Marks AR (1998) Coupled gating between individual skeletal muscle Ca2+ release channels (ryanodine receptors). Science 281(5378):818–821
Marx SO, Reiken S, Hisamatsu Y, Gaburjakova M, Gaburjakova J, Yang YM, Rosemblit N, Marks AR (2001) Phosphorylation-dependent regulation of ryanodine receptors: a novel role for leucine/isoleucine zippers. J Cell Biol 153(4):699–708
McCall E, Ginsburg KS, Bassani RA, Shannon TR, Qi M, Samarel AM, Bers DM (1998) Ca flux, contractility, and excitation–contraction coupling in hypertrophic rat ventricular myocytes. Am J Physiol 274(4 Pt 2):H1348–H1360
Mejia-Alvarez R, Kettlun C, Rios E, Stern M, Fill M (1999) Unitary Ca2+ current through cardiac ryanodine receptor channels under quasi-physiological ionic conditions. J Gen Physiol 113(2):177–186
Protasi F, Franzini-Armstrong C, Flucher BE (1997) Coordinated incorporation of skeletal muscle dihydropyridine receptors and ryanodine receptors in peripheral couplings of BC3H1 cells. J Cell Biol 137(4):859–870
Rios E, Stern MD (1997) Calcium in close quarters: microdomain feedback in excitation–contraction coupling and other cell biological phenomena. Annu Rev Biophys Biomol Struct 26:47–82. doi:10.1146/annurev.biophys.26.1.47
Schulson MN, Scriven DRL, Fletcher PA, Moore EDW (2011) Couplons in rat atria form distinct subgroups defined by their molecular partners. J Cell Science 124:1167–1174
Scott JD, Pawson T (2009) Cell signaling in space and time: where proteins come together and when they're apart. Science 326(5957):1220–1224. doi:10.1126/science.1175668
Scriven DR, Dan P, Moore ED (2000) Distribution of proteins implicated in excitation–contraction coupling in rat ventricular myocytes. Biophys J 79(5):2682–2691
Scriven DRL, Klimek A, Asghari P, Bellve K, Moore EDW (2005) Caveolin-3 is adjacent to a group of extra-dyadic ryanodine receptors. Biophys J 89:1893–1901
Scriven DR, Asghari P, Schulson MN, Moore ED (2010) Analysis of Cav1.2 and ryanodine receptor clusters in rat ventricular myocytes. Biophys J 99(12):3923–3929
Sher AA, Noble PJ, Hinch R, Gavaghan DJ, Noble D (2008) The role of the Na+/Ca2+ exchangers in Ca2+ dynamics in ventricular myocytes. Prog Biophys Mol Biol 96(1–3):377–398
Shorofsky SR, Aggarwal R, Corretti M, Baffa JM, Strum JM, Al-Seikhan BA, Kobayashi YM, Jones LR, Wier WG, Balke CW (1999) Cellular mechanisms of altered contractility in the hypertrophied heart: big hearts, big sparks. Circ Res 84(4):424–434
Stern MD (1992) Theory of excitation–contraction coupling in cardiac muscle. Biophys J 63(2):497–517
Stern MD, Pizarro G, Rios E (1997) Local control model of excitation–contraction coupling in skeletal muscle. J Gen Physiol 110(4):415–440
Sun XH, Protasi F, Takahashi M, Takeshima H, Ferguson DG, Franzini-Armstrong C (1995) Molecular architecture of membranes involved in excitation–contraction coupling of cardiac muscle. J Cell Biol 129(3):659–671
Takimoto E, Champion HC, Belardi D, Moslehi J, Mongillo M, Mergia E, Montrose DC, Isoda T, Aufiero K, Zaccolo M, Dostmann WR, Smith CJ, Kass DA (2005) cGMP catabolism by phosphodiesterase 5A regulates cardiac adrenergic stimulation by NOS3-dependent mechanism. Circ Res 96(1):100–109
Thomas NL, Maxwell C, Mukherjee S, Williams AJ (2010) Ryanodine receptor mutations in arrhythmia: the continuing mystery of channel dysfunction. FEBS Lett 584(10):2153–2160
Wang SQ, Stern MD, Rios E, Cheng H (2004) The quantal nature of Ca2+ sparks and in situ operation of the ryanodine receptor array in cardiac cells. Proc Natl Acad Sci USA 101(11):3979–3984
Xiao RP, Avdonin P, Zhou YY, Cheng H, Akhter SA, Eschenhagen T, Lefkowitz RJ, Koch WJ, Lakatta EG (1999) Coupling of beta2-adrenoceptor to Gi proteins and its physiological relevance in murine cardiac myocytes. Circ Res 84(1):43–52
Xie W, Brochet DX, Wei S, Wang X, Cheng H (2010) Deciphering ryanodine receptor array operation in cardiac myocytes. J Gen Physiol 136(2):129–133
Acknowledgments
This work was supported by grants from the Canadian Institutes of Health Research (MOP12875) and the Natural Scientific and Engineering Research Council of Canada to EDWM.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Handling Editor: Geoffrey O. Wasteneys
Rights and permissions
About this article
Cite this article
Asghari, P., Scriven, D.R.L., Hoskins, J. et al. The structure and functioning of the couplon in the mammalian cardiomyocyte. Protoplasma 249 (Suppl 1), 31–38 (2012). https://doi.org/10.1007/s00709-011-0347-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00709-011-0347-5