Abstract
Purpose
Analyze the modifications in the “safe zones” of T4–L4 vertebral bodies relative to aorta according to patient positioning, as well as in the relationship between the aorta and the vertebrae.
Methods
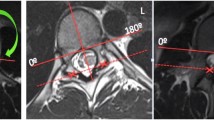
Patients with adolescent idiopathic scoliosis who underwent surgical treatment during 2017 were included. Preoperative whole spine MRI in supine, prone, and LD positions was performed. The safe zone right (SZR) was defined as the angle formed between X-axis (0º) and a line connecting the origin and the edge of the aorta, and the safe zone left (SZL) was the angle between the edge of the aorta to 180º (X-axis).
Results
A total of 21 patients were studied, median age was 15.2 years, and 71.4% were female. The mean SZR lied from 0°–86.1º at T4 to 0°–76.9º at L4 in supine, from 0°–84.05º at T4 to 0º–78.5º at L4 in prone, and from 0° to 91.75º at T4 to 0°–80.4º at L4 in LD. While the mean SZL was located from 155.4º–180º at T4 to 107.9º–180º at L4 in supine, from 134°–180° at T4 to 103.9°–180° at L4 in prone, and from 143.8º–180º at T4 to 106º–180º at L4 in LD. Statistically significant differences were found almost at all levels when comparing supine versus prone and LD.
Conclusions
Patient positioning during spinal surgery significantly modifies T4–L4 vertebral safe zones relative to aorta. These variations should be taken into account when analyzing an MRI performed in supine if the patient is undergoing surgery in a different position, to avoid vascular-related injuries.







Similar content being viewed by others
References
Fantini GA, Pappou IP, Girardi FP, Sandhu HS, Cammisa FP Jr (2007) Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine 32(24):2751–2758. https://doi.org/10.1097/BRS.0b013e31815a996e
Lavigne F, Mascard E, Laurian C, Dubousset J, Wicart P (2009) Delayed-iatrogenic injury of the thoracic aorta by an anterior spinal instrumentation. Eur Spine J Official Publicat Eur Spine Soc Eur Spinal Deform Soc, Eur Sect Cerv Spine Res Soc 18(2):265–268. https://doi.org/10.1007/s00586-009-0974-0
Uribe JS, Deukmedjian AR (2015) Visceral, vascular, and wound complications following over 13,000 lateral interbody fusions: a survey study and literature review. Eur Spine J 24(3):386–396
Szolar DH, Preidler KW, Steiner H, Riepl T, Flaschka G, Stiskal M, Norman D (1996) Vascular complications in lumbar disk surgery: report of four cases. Neuroradiology 38(6):521–525
Hicks JM, Singla A, Shen FH, Arlet V (2010) Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine 35(11):E465–E470
Moore KL (2010) The thoracic and abdominal aorta. In: Moore KL (ed) Clinacally Oriented Anatomy, 6thd edn. Williams & Wilkins, Baltimor, pp 167–313
Sucato DJ, Duchene C (2003) The position of the aorta relative to the spine: a comparison of patients with and without idiopathic scoliosis. J Bone Joint Surg Am 85(8):1461–1469
Milbrandt TA, Sucato DJ (2007) The position of the aorta relative to the spine in patients with left thoracic scoliosis: a comparison with normal patients. Spine 32(12):E348–E353
Chiu CK, Lee KJ, Chung WH, Chandren JR, Chan C, Kwan MK (2019) Does the Severity of the curve in Lenke 1 and 2 adolescent idiopathic scoliosis patients affect the distance and position of the aorta from vertebra? Spine 44(11):785–792. https://doi.org/10.1097/BRS.0000000000002945
Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y (2005) Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spin Disord Techniq 18(6):522–526
Şarlak AY, Tosun B, Atmaca H, Sarisoy HT, Buluç L (2009) Evaluation of thoracic pedicle screw placement in adolescent idiopathic scoliosis. Eur Spine J 18(12):1892–1897
Jiang H, Qiu X, Wang W, Zhu Z, Qian B, Guo J, Qiu Y (2012) The position of the aorta changes with altered body position in single right thoracic adolescent idiopathic scoliosis: a magnetic resonance imaging study. Spine 37(17):E1054–E1061
Huitema GC, Cornips EM, Castelijns MH et al (2007) The position of the aorta relative to the spine: is it mobile or not? Spine 32(12):1259–1264
Plataniotis N, Evangelopoulos DS, Katzouraki G, Pneumaticos S (2019) The effect of patient positioning on the relative position of the aorta to the thoracic spine. Euro Spine J Official Publicat Euro Spine Soc Euro Spinal Deform Soc Euro Sect Cerv Spine Res Soc 28(3):477–483. https://doi.org/10.1007/s00586-018-5812-9
Sucato DJ, Kassab F, Dempsey M (2004) Analysis of screw placement relative to the aorta and spinal canal following anterior instrumentation for thoracic idiopathic scoliosis. Spine 29(5):554–559. https://doi.org/10.1097/01.brs.0000106495.91477.92
Takeshita K, Maruyama T, Ono T, Ogihara S, Chikuda H, Shoda N, Nakamura K (2010) New parameters to represent the position of the aorta relative to the spine for pedicle screw placement. Eur Spine J 19(5):815–820
Qiao J, Zhu F, Xu L, Zhu Z, Qian B, Liu Z, Qiu Y (2012) Comparison of the aorta impingement risks between thoracolumbar/lumbar curves with different convexities in adolescent idiopathic scoliosis: a computed tomography study. Eur Spine J 21(10):2043–2049
Liu J, Shen J, Zhang J, Li S, Zhao H, Qiu G, Wang Y (2012) The position of the aorta relative to the spine for pedicle screw placement in the correction of idiopathic scoliosis. Clinical Spine Surgery 25(4):E103–E107
Bekki H, Harimaya K, Matsumoto Y, Hayashida M, Okada S, Doi T, Iwamoto Y (2016) The position of the aorta relative to the vertebrae in patients with lenke type 1 adolescent idiopathic scoliosis. Spine 41(7):585–590
Egea-Gámez RM, Wilson-MacDonald J, Murray D, González-Díaz R (2020) Definition of safe zone in vertebral body in relation to anterior instrumentation. Spine Deform. https://doi.org/10.1007/s43390-020-00100-w
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83:1169–1181
Bullmann V, Fallenberg EM, Meier N, Fischbach R, Lerner T, Schulte TL, Liljenqvist UR (2006) The position of the aorta relative to the spine before and after anterior instrumentation in right thoracic scoliosis. Spine 31(15):1706–1713
Vaccaro AR, Kepler CK, Rihn JA, Suzuki H, Ratliff JK, Harrop JS, Albert TJ (2012) Anatomical relationships of the anterior blood vessels to the lower lumbar intervertebral discs. J Bone Joint Surg 94(12):1088–1094
Takeshita K, Maruyama T, Nakao Y, Ono T, Taniguchi Y, Chikuda H, Nakamura K (2010) Aorta movement in patients with scoliosis after posterior surgery. Spine 35(26):E1571–E1576
Chan C, Kwan MK (2018) Zonal differences in risk and pattern of pedicle screw perforations in adolescent idiopathic scoliosis (AIS): a computerized tomography (CT) review of 1986 screws. Eur Spine J Official Publicat Euro Spine Soc Euro Spinal Deform Soc Euro Sect Cerv Spine Res Soc 27(2):340–349. https://doi.org/10.1007/s00586-017-5350-x
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
I and the other authors have NO financial relationship(s) with a commercial interest producing healthcare goods or services.
Ethical approval
This study was carried out in accordance with the World Medical Association Declaration of Helsinki (JBJS 79A:1089-98, 1997).
Informed consent
Patients confidentiality was protected according to the U.S. Health Insurance Portability and Accountability Act (HIPAA).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Egea-Gámez, R.M., Galán-Olleros, M., Rodríguez del Real, T. et al. Variations in the position of the aorta and vertebral safe zones in supine, prone, and lateral decubitus for adolescent idiopathic scoliosis. Eur Spine J 30, 1950–1958 (2021). https://doi.org/10.1007/s00586-021-06813-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06813-4