Abstract
Purpose
To investigate if the presence or absence of preoperative endplate Modic changes (MC) is predictive for clinical outcomes in degenerative lumbar spinal stenosis (DLSS) patients undergoing decompression-alone or decompression with instrumented fusion surgery.
Methods
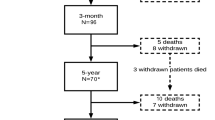
Two hundred five patients were included and categorized into four groups; 102 patients into the decompression-alone group with MCs, 41 patients into the fusion group with MCs, 46 patients into the decompression-alone group without MCs, and 16 patients into the fusion group without MCs. Clinical outcome was quantified with changes in spinal stenosis measure (SSM) symptoms, SSM function, NRS pain, and EQ-5D-3L sum score over time (measured at baseline, 12-, 24-, and 36-month follow-up) and minimal clinically important difference (MCID) in SSM symptoms, SSM function, and NRS pain from baseline to 36-month follow-up. To investigate if possible effects of MCs had been modified or hidden by confounding variables, we used the group LASSO method to search for good prognostic models.
Results
There were no obvious differences in any of the clinical outcome measures between groups at baseline. At 12 months, most patients have improved in all outcomes and maintained improved conditions over time (no significant group differences). Between 70 and 90 percent of the patients maintained a clinically important improvement up to 36 months.
Conclusions
Endplate MCs have no significant influence on clinical outcome parameters in patients with lumbar spinal stenosis compared to patients without MCs, independent of the chosen surgical strategy. All patients benefitted from surgical therapy up to 36-month follow-up.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.




Similar content being viewed by others
Abbreviations
- DLSS:
-
Degenerative lumbar spinal stenosis
- LSOS:
-
Lumbar Stenosis Outcome Study
References
de Roos A, Kressel H, Spritzer C, Dalinka M (1987) MR imaging of marrow changes adjacent to end plates in degenerative lumbar disk disease. AJR Am J Roentgenol 149(3):531–534. https://doi.org/10.2214/ajr.149.3.531
Modic MT, Masaryk TJ, Ross JS, Carter JR (1988) Imaging of degenerative disk disease. Radiology 168(1):177–186. https://doi.org/10.1148/radiology.168.1.3289089
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166(1 Pt 1):193–199. https://doi.org/10.1148/radiology.166.1.3336678
Zhang Y-H, Zhao C-Q, Jiang L-S, Chen X-D, Dai L-Y (2008) Modic changes: a systematic review of the literature. Eur Spine J 17(10):1289–1299. https://doi.org/10.1007/s00586-008-0758-y
Albert HB, Briggs AM, Kent P, Byrhagen A, Hansen C, Kjaergaard K (2011) The prevalence of MRI-defined spinal pathoanatomies and their association with modic changes in individuals seeking care for low back pain. Eur Spine J 20(8):1355–1362. https://doi.org/10.1007/s00586-011-1794-6
Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C (2008) Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J 17(11):1407–1422. https://doi.org/10.1007/s00586-008-0770-2
Mok FPS, Samartzis D, Karppinen J, Fong DYT, Luk KDK, Cheung KMC (2016) Modic changes of the lumbar spine: prevalence, risk factors, and association with disc degeneration and low back pain in a large-scale population-based cohort. Spine J 16(1):32–41. https://doi.org/10.1016/j.spinee.2015.09.060
Rahme R, Moussa R (2008) The modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. Am J Neuroradiol 29(5):838–842
Lang P, Chafetz N, Genant HK, Morris JM (1990) Lumbar spinal fusion. Assessment of functional stability with magnetic resonance imaging. Spine (Phila Pa 1976) 15(6):581–588
Braithwaite I, White J, Saifuddin A, Renton P, Taylor BA (1998) Vertebral end-plate (Modic) changes on lumbar spine MRI: correlation with pain reproduction at lumbar discography. Eur Spine J 7(5):363–368
Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Jensen TS, Manniche C (2012) Is the development of Modic changes associated with clinical symptoms? A 14-month cohort study with MRI. Eur Spine J 21(11):2271–2279. https://doi.org/10.1007/s00586-012-2309-9
Albert HB, Sorensen JS, Christensen BS, Manniche C (2013) Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J 22(4):697–707. https://doi.org/10.1007/s00586-013-2675-y
Albert HB, Manniche C, Sorensen JS, Deleuran BW (2008) Antibiotic treatment in patients with low-back pain associated with Modic changes Type 1 (bone oedema): a pilot study. Br J Sports Med 42(12):969–973. https://doi.org/10.1136/bjsm.2008.050369
Cao P, Chen Z, Zheng Y, Wang Y, Jiang L, Yang Y, Zhuang C, Liang Y, Zheng T, Gong Y, Zhang X, Wu W, Qiu S (2014) Comparison of simple discectomy and instrumented posterior lumbar interbody fusion for treatment of lumbar disc herniation combined with Modic endplate changes. Chin Med J (Engl) 127(15):2789–2794
Ghodsi SM, Rouhani R, Abdollahzade S, Khadivi M, Faghih Jouibari M (2015) Frequency of vertebral endplate modic changes in patients with unstable lumbar spine and its effect on surgical outcome. Asian Spine J 9(5):737–740. https://doi.org/10.4184/asj.2015.9.5.737
Kwon YM, Chin DK, Jin BH, Kim KS, Cho YE, Kuh SU (2009) Long term efficacy of posterior lumbar interbody fusion with standard cages alone in lumbar disc diseases combined with modic changes. J Korean Neurosurg Soc 46(4):322–327. https://doi.org/10.3340/jkns.2009.46.4.322
Rauschning W (1993) Pathoanatomy of lumbar disc degeneration and stenosis. Acta Orthop Scand Suppl 251:3–12
Hayashi T, Daubs MD, Suzuki A, Scott TP, Phan KH, Ruangchainikom M, Takahashi S, Shiba K, Wang JC (2015) Motion characteristics and related factors of Modic changes in the lumbar spine. J Neurosurg Spine 22(5):511–517. https://doi.org/10.3171/2014.10.SPINE14496
Ohtori S, Yamashita M, Yamauchi K, Inoue G, Koshi T, Suzuki M, Orita S, Eguchi Y, Ochiai N, Kishida S, Takaso M, Aoki Y, Ishikawa T, Arai G, Miyagi M, Kamoda H, Nakamura J, Takahashi K (2010) Low back pain after lumbar discectomy in patients showing endplate modic type 1 change. Spine (Phila Pa 1976) 35(13):E596–600. https://doi.org/10.1097/brs.0b013e3181cd2cb8
Ulrich NH, Burgstaller JM, Gravestock I, Pichierri G, Wertli MM, Steurer J, Farshad M, Porchet F (2019) Outcome of unilateral versus standard open midline approach for bilateral decompression in lumbar spinal stenosis: is “over the top” really better? A Swiss prospective multicenter cohort study. J Neurosurg Spine. https://doi.org/10.3171/2019.2.spine181309
Ulrich NH, Burgstaller JM, Pichierri G, Wertli MM, Farshad M, Porchet F, Steurer J, Held U, Grp LS (2017) Decompression surgery alone versus decompression plus fusion in symptomatic lumbar spinal stenosis. Spine 42(18):E1077–E1086. https://doi.org/10.1097/Brs.0000000000002068
Burgstaller JM, Wertli MM, Steurer J, Kessels AG, Held U, Gramke H-F, Group LS (2017) The influence of pre-and postoperative fear avoidance beliefs on postoperative pain and disability in patients with lumbar spinal stenosis: analysis of the lumbar spinal outcome study (LSOS) data. Spine 42(7):E425–E432
Steurer J, Nydegger A, Held U, Brunner F, Hodler J, Porchet F, Min K, Mannion AF, Michel B, Collaboration LR (2010) LumbSten: the lumbar spinal stenosis outcome study. Bmc Musculoskel Dis. https://doi.org/10.1186/1471-2474-11-254
Stucki G, Liang MH, Fossel AH, Katz JN (1995) Relative responsiveness of condition-specific and generic health status measures in degenerative lumbar spinal stenosis. J Clin Epidemiol 48(11):1369–1378
Stucki G, Daltroy L, Liang MH, Lipson SJ, Fossel AH, Katz JN (1996) Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine (Phila Pa 1976) 21(7):796–803
Hinz A, Klaiberg A, Brahler E, Konig HH (2006) The quality of life questionnaire EQ-5D: modelling and norm values for the general population. Psychother Psychosom Med Psychol 56(2):42–48. https://doi.org/10.1055/s-2005-867061
Ostelo RWJG, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, Bouter LM, de Vet HC (2008) Interpreting change scores for pain and functional status in low back pain—towards international consensus regarding minimal important change. Spine 33(1):90–94
Yang Y, Zou H (2015) A fast unified algorithm for solving group-lasso penalize learning problems. Stat Comput 25(6):1129–1141. https://doi.org/10.1007/s11222-014-9498-5
Acknowledgements
The authors thank the Baugarten Foundation, the Helmut Horten Foundation, the Pfizer-Foundation for geriatrics and research in geriatrics, the Symphasis Charitable Foundation, and the OPO Foundation for their support.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ulrich, N.H., Burgstaller, J.M., Gravestock, I. et al. The influence of endplate (Modic) changes on clinical outcomes in lumbar spinal stenosis surgery: a Swiss prospective multicenter cohort study. Eur Spine J 29, 2205–2214 (2020). https://doi.org/10.1007/s00586-020-06364-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06364-0