Abstract
Purpose
Various design concepts have been adopted in cervical disc prostheses, including sliding articulation and standalone configuration. This study aimed to evaluate the biomechanical effects of the standalone U-shaped configuration on the cervical spine.
Methods
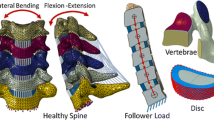
Based on an intact finite element model of C3–C7, a standalone U-shaped implant (DCI) was installed at C5–C6 and compared with a sliding articulation design (Prodisc-C) and an anterior fusion system. The range of motion (ROM), adjacent intradiscal pressure (IDP) and capsular ligament strain were calculated under different spinal motions.
Results
Compared to the intact configuration, the ROM at C5–C6 was reduced by 90 % after fusion, but increased by 70 % in the Prodisc-C model, while the maximum percentage change in the DCI model was 30 % decrease. At the adjacent segments, up to 32 % increase in ROM happened after fusion, while up to 34 % decrease occurred in Prodisc-C model and 17 % decrease in DCI model. The IDP increased by 11.6 % after fusion, but decreased by 5.6 and 6.3 % in the DCI and Prodisc-C model, respectively. The capsular ligament strain increased by 147 % in Prodisc-C and by 13 % in the DCI model. The DCI implant exhibited a high stress distribution.
Conclusions
Spinal fusion resulted in compensatory increase of ROM at the adjacent sites, thereby elevating the IDP. Prodisc-C resulted in hyper-mobility at the operative site that led to an increase of ligament force and strain. The U-shaped implant could maintain the spinal kinematics and impose minimum influence on the adjacent soft tissues, despite the standalone configuration encountering the disadvantages of high stress distribution.







Similar content being viewed by others
References
Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y (2010) Adjacent segment disease and degeneration after anterior cervical decompression and fusion. Neurosurg Quart 20:15–22. doi:10.1097/WNQ.0b013e3181ce0d13
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4:S190–S194
Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J (2007) Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine 7:33–39. doi:10.3171/SPI-07/07/033
Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC (2005) Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine 30:1165–1172
Galbusera F, Bellini CM, Brayda-Bruno M, Fornari M (2008) Biomechanical studies on cervical total disc arthroplasty: a literature review. Clin Biomech 23:1095–1104. doi:10.1016/j.clinbiomech.2008.06.002
Chang U, Kim DH, Lee MC, Willenberg R, Kim S, Lim J (2007) Range of motion change after cervical arthroplasty with ProDisc-C and Prestige artificial discs compared with anterior cervical discectomy and fusion. J Neurosurg Spine 7:40–46
Kotani Y, Cunningham BW, Abumi K, Dmitriev AE, Ito M, Hu N, Shikinami Y, McAfee PC, Minami A (2005) Multidirectional flexibility analysis of cervical artificial disc reconstruction: in vitro human cadaveric spine model. J Neurosurg Spine 2:188–194
Lee S, Im Y, Kim K, Kim Y, Park W, Kim K (2011) Comparison of cervical spine biomechanics after fixed- and mobile-core artificial disc replacement: a finite element analysis. Spine 36:700–708
Anderson PA, Sasso RC, Rouleau JP, Carlson CS, Goffin J (2004) The Bryan Cervical Disc: wear properties and early clinical results. Spine J 4:S303–S309
Wilke HJ, Drumm J, Haussler K, Mack C, Steudel W, Kettler A (2008) Biomechanical effect of different lumbar interspinous implants on flexibility and intradiscal pressure. Eur Spine J 17:1049–1056. doi:10.1007/s00586-008-0657-2
Matgé G, Eif M, Herdmann J, Lowery GL (2009) Dynamic Cervical Implant (DCI™): clinical results from an international multicenter prospective study. Paradigm Spine:1–3
DiAngelo DJ, Foley KT, Morrow BR, Schwab JS, Song J, German JW, Blair E (2004) In vitro biomechanics of cervical disc arthroplasty with the ProDisc-C total disc implant. Neurosurg Focus 17:E7
Kurtz SM, Edidin AA (2006) Spine technology handbook. Elsevier Inc., Burlington
Denozière G, Ku DN (2006) Biomechanical comparison between fusion of two vertebrae and implantation of an artificial intervertebral disc. J Biomech 39:766–775
Drake RL, Vogl AW, Mitchell AWM, Tibbitts R, Richardson P (2008) Gray’s Atlas of Anatomy. Churchill livingstone Elsevier, Philadelphia
Narayan Y, Srirangam K, Frank AP (2000) Geometric and mechanical properties of human cervical spine ligaments. J Biomech Eng 122:623–629
Hong-Wan N, Ee-Chon T, Qing-Hang Z (2004) Biomechanical Effects of C2–C7 intersegmental stability due to laminectomy with unilateral and bilateral facetectomy. Spine 29:1737–1745
Jirkova L, Horak Z (2009) Analysis of influence location of intervertebral implant on the lower cervical spine loading and stability. IFMBE Proceedings 23:1724–1727
Panjabi MM, Crisco JJ, Vasavada A, Oda T, Cholewicki J, Nibu K, Shin E (2001) Mechanical properties of the human cervical spine as shown by three-dimensional load–displacement curves. Spine 26:2692–2700
Moroney SP, Schultz AB, Miller JAA, Andersson GBJ (1988) Load–displacement properties of lower cervical spine motion segments. J Biomech 21:769–779
Finn MA, Brodke DS, Daubs M, Patel A, Bachus KN (2009) Local and global subaxial cervical spine biomechanics after single-level fusion or cervical arthroplasty. Eur Spine J 18:1520–1527. doi:10.1007/s00586-009-1085-7
McNally DS, Shackleford IM, Goodship AE, Mulholland RC (1996) In vivo stress measurement can predict pain on discography. Spine 21:2580–2587
Barrey C, Mosnier T, Jund J, Perrin G, Skalli W (2009) In vitro evaluation of a ball-and-socket cervical disc prosthesis with cranial geometric center. J Neurosurg Spine 11:538–546. doi:10.3171/2009.6.SPINE0949
Liu F, Cheng J, Komistek RD, Mahfouz MR, Sharma A (2007) In vivo evaluation of dynamic characteristics of the normal, fused, and disc replacement cervical spines. Spine 32:2578–2584
Kowalczyk I, Lazaro BCR, Fink M, Rabin D, Duggal N (2011) Analysis of in vivo kinematics of 3 different cervical devices: Bryan disc, ProDisc-C, and Prestige LP disc. J Neurosurg Spine 15:630–635. doi:10.3171/2011.8.SPINE11273
Duggal N, Bertagnoli R, Rabin D, Wharton N, Kowalczyk I (2011) ProDisc-C: an in vivo kinematic study. J Spinal Disord Tech 24:334–339. doi:10.1097/BSD.0b013e3181fbf8aa
Bauman JA, Jaumard NV, Guarino BB, Weisshaar CL, Lipschutz DE, Welch WC, Winkelstein BA (2012) Facet joint contact pressure is not significantly affected by ProDisc cervical disc arthroplasty in sagittal bending: a single-level cadaveric study. Spine J 12:949–959
Womack W, Leahy PD, Patel VV, Puttlitz CM (2011) Finite element modeling of kinematic and load transmission alterations due to cervical intervertebral disc replacement. Spine 36 (Phila Pa 1976):E1126–E1133. doi:10.1097/BRS.0b013e31820e3dd1
Teoh SH (2000) Fatigue of biomaterials: a review. Int J Fatigue 22:825–837
Goel VK, Panjabi MM, Patwardhan AG, Dooris AP, Serhan H (2006) Test protocols for evaluation of spinal implants. J Bone Joint Surg 88:103–109
Acknowledgments
This project was supported by the National Natural Science Foundation of China (Nos. 10925208, 11120101001, 11202017, 11272273 and 81271666), the 111 Project (No. B13003), National Science & Technology Pillar Program (Nos. 2012BAI18B05, 2012BAI18B07) and The Hong Kong Polytechnic university Research Grant (No. G-UA40).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Zhong Jun Mo and Yan Bin Zhao contributed equally to this work.
Rights and permissions
About this article
Cite this article
Mo, Z.J., Zhao, Y.B., Wang, L.Z. et al. Biomechanical effects of cervical arthroplasty with U-shaped disc implant on segmental range of motion and loading of surrounding soft tissue. Eur Spine J 23, 613–621 (2014). https://doi.org/10.1007/s00586-013-3070-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-3070-4