Abstract
Background
Some pregnant women avoid labor epidural analgesia because of their concerns about risk of cerebral palsy in children. Although it is believed that labor epidural does not contribute to cerebral palsy, to our knowledge no study has been published to specifically address this concern. We carried out a retrospective case–control study to investigate whether labor epidural analgesia is associated with cerebral palsy in children.
Methods
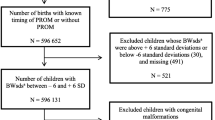
This study used data that were collected and entered into the Geisinger electronic health records between January 2004 and January 2013. During this period, 20,929 children were born at Geisinger hospitals. Among them, 50 children were diagnosed with cerebral palsy, and 20 of those were born vaginally. Each of these 20 cerebral palsy children was matched with up to 5 non-cerebral palsy children born at the same hospitals in the same timeframe using propensity scoring methods. Analgesia was classified as epidural (including epidural or combined spinal and epidural) or non-epidural. Conditional logistic regression was used to compare the percentages of deliveries with each analgesia type between the cerebral palsy and non-cerebral palsy groups.
Results
In the non-cerebral palsy group, the percentage of patients receiving labor epidural analgesia was 72 %, and in the cerebral palsy group the percentage was 45 %. There was no significant difference between non-cerebral palsy and cerebral palsy groups (odds ratio, 0.57; 95 % confidence interval, 0.14–2.24; p = 0.42).
Conclusion
We found no association between the use of labor epidural analgesia and the occurrence of cerebral palsy in children.
Similar content being viewed by others
References
Osterman MJ, Martin JA. Epidural and spinal anesthesia use during labor: 27-state reporting area, 2008. Natl Vital Stat Rep. 2011;59(5):1–13.
Toledo P, Sun J, Peralta F, Grobman WA, Wong CA, Hasnain-Wynia R. A qualitative analysis of parturients’ perspectives on neuraxial labor analgesia. Int J Obstet Anesth. 2013;22(2):119–23.
Pakula AT, Braun NK, Yeargin-Allsopp M. Cerebral palsy: classification and epidemiology. Phys Med Rehabil Clin N Am. 2009;20(3):425–52.
Oskoui M, Coutinho F, Dykeman J, Jette N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55(6):509–19.
Kirby RS, Wingate MS, Van Naarden Braun K, Doernberg NS, Arneson CL, Benedict RE, Mulvihill B, Durkin MS, Fitzgerald RT, Maenner MJ, Patz JA, Yeargin-Allsopp M. Prevalence and functioning of children with cerebral palsy in four areas of the United States in 2006: a report from the Autism and Developmental Disabilities Monitoring Network. Res Dev Disabil. 2011;32(2):462–9.
Dunn PM. Dr. William Little (1810–1894) of London and cerebral palsy. Arch Dis Child Fetal Neonatal Ed. 1995;72(3):F209–10.
Tronnes H, Wilcox AJ, Lie RT, Markestad T, Moster D. Risk of cerebral palsy in relation to pregnancy disorders and preterm birth: a national cohort study. Dev Med Child Neurol. 2014;56(8):779–85.
Janik MD, Newman TB, Cheng YW, Xing G, Gilbert WM, Wu YW. Maternal diagnosis of obesity and risk of cerebral palsy in the child. J Pediatr. 2013;163(5):1307–12.
Strand KM, Heimstad R, Iversen AC, Austgulen R, Lydersen S, Andersen GL, Irgens LM, Vik T. Mediators of the association between pre-eclampsia and cerebral palsy: population based cohort study. BMJ. 2013;9(347):f4089.
Wu YW, Croen LA, Torres AR, Van De Water J, Grether JK, Hsu NN. Interleukin-6 genotype and risk for cerebral palsy in term and near-term infants. Ann Neurol. 2009;66(5):663–70.
Moreno-De-Luca A, Ledbetter DH, Martin CL. Genetic [corrected] insights into the causes and classification of [corrected] cerebral palsies. Lancet Neurol. 2012;11(3):283–92.
Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, Dan B. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005;47(8):571–6.
Hudson AE, Hemmings HC Jr. Are anaesthetics toxic to the brain? Br J Anaesth. 2011;107(1):30–7.
Ing C, DiMaggio C, Whitehouse A, Hegarty MK, Brady J, von Ungern-Sternberg BS, Davidson A, Wood AJ, Li G, Sun LS. Long-term differences in language and cognitive function after childhood exposure to anesthesia. Pediatrics. 2012;130(3):e476–85.
Wilder RT, Flick RP, Sprung J, Katusic SK, Barbaresi WJ, Mickelson C, Gleich SJ, Schroeder DR, Weaver AL, Warner DO. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology. 2009;110(4):796–804.
Block RI, Thomas JJ, Bayman EO, Choi JY, Kimble KK, Todd MM. Are anesthesia and surgery during infancy associated with altered academic performance during childhood? Anesthesiology. 2012;117(3):494–503.
Greenwell EA, Wyshak G, Ringer SA, Johnson LC, Rivkin MJ, Lieberman E. Intrapartum temperature elevation, epidural use, and adverse outcome in term infants. Pediatrics. 2012;129(2):e447–54.
Flick RP, Lee K, Hofer RE, Beinborn CW, Hambel EM, Klein MK, Gunn PW, Wilder RT, Katusic SK, Schroeder DR, Warner DO, Sprung J. Neuraxial labor analgesia for vaginal delivery and its effects on childhood learning disabilities. Anesth Analg. 2011;112(6):1424–31.
Thorngren-Jerneck K, Herbst A. Perinatal factors associated with cerebral palsy in children born in Sweden. Obstet Gynecol. 2006;108(6):1499–505.
Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8(1):110–24.
Dammann O, Leviton A. Brain damage in preterm newborns: might enhancement of developmentally regulated endogenous protection open a door for prevention? Pediatrics. 1999;104(3 pt 1):541–50.
Nelson KB, Willoughby RE. Overview: infection during pregnancy and neurologic outcome in the child. Ment Retard Dev Disabil Res Rev. 2002;8(1):1–2.
Ahlin K, Himmelmann K, Hagberg G, Kacerovsky M, Cobo T, Wennerholm UB. Cerebral palsy and perinatal infection in children born at term. Obstet Gynecol. 2013;122(1):41–9.
Berry SA, Laam LA, Wary AA, Mateer HO, Cassagnol HP, McKinley KE, Nolan RA. ProvenCare perinatal: a model for delivering evidence/guideline-based care for perinatal populations. Jt Comm J Qual Patient Saf. 2011;37(5):229–39.
Pappas A, Kendrick DE, Shankaran S, Stoll BJ, Bell EF, Laptook AR, Walsh MC, Das A, Hale EC, Newman NS, Higgins RD, Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Chorioamnionitis and early childhood outcomes among extremely low-gestational-age neonates. JAMA Pediatr. 2014;168(2):137–47.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
This study received no external funding, and the authors have no conflicts of interest to declare.
About this article
Cite this article
Zhang, L., Graham, J.H., Feng, W. et al. No association of labor epidural analgesia with cerebral palsy in children. J Anesth 30, 1008–1013 (2016). https://doi.org/10.1007/s00540-016-2244-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2244-8