Abstract
Background
The genetic variants of NUDT15 have been verified to induce adverse events (AEs) of thiopurines. Codon 139 variants are frequently observed in Asians, while multiple variants are seen in codon 18 which also cause AEs including the European ancestry. The purpose of this study is to establish a technique capable of the simple genotyping of NUDT15 codon 18 and to evaluate its efficacy.
Methods
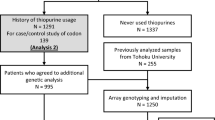
A high-resolution melt (HRM) technique is performed to simply determine genotypes. The accuracy of HRM analysis was evaluated with DNAs from 1245 Japanese patients with inflammatory bowel diseases. Subsequently, another group of 572 patients was analyzed to verify the method. The diplotypes and the frequency of their AEs were estimated on the basis of codon 18 and 139 genotypes.
Results
The HRM analysis enabled the correct identification of the three main genotypes, ref/ref, ref/ins, and ref/V18I, in 1236 of 1241 cases. All rare genotypes including ref/del were identified as the impossible-to-determine group, the proper diagnosis rate was 99.6%. In the verification test using other samples, the diagnosis rate was 99.7%. By estimating diplotypes using both codon 18 and 139 genotypes, 2.74% and 2.13% of Japanese patients with Arg/Arg and Arg/Cys of codon 139 have a lower enzymatic activity of NUDT15 and a higher risk for adverse responses than those estimated by codon 139 genotypes alone.
Conclusions
Our study showed that HRM method enables simple genotyping of complicated codon 18 variants essential to haplotype estimation of the NUDT15.



Similar content being viewed by others
Change history
25 November 2019
The correct name of the last author should be.
Abbreviations
- IBD:
-
Inflammatory bowel disease
- UC:
-
Ulcerative colitis
- CD:
-
Crohn’s disease
- BD:
-
Behçet’s disease
- AZA:
-
Azathiopurine
- 6-MP:
-
6-Mercaptopurine
- AE:
-
Adverse event
- WBC:
-
White blood cell
- HRM:
-
High-resolution melt
References
Jewell DP, Truelove SC. Azathioprine in ulcerative colitis: final report on controlled therapeutic trial. Br Med J. 1974;4:627–30.
Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, et al. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. 2010;362:1383–95.
Panaccione R, Ghosh S, Middleton S, Marquez JR, Scott BB, Flint L, et al. Combination therapy with infliximab and azathioprine is superior to monotherapy with either agent in ulcerative colitis. Gastroenterology. 2014;146:392–400.
Takatsu N, Matsui T, Murakami Y, Ishihara H, Hisabe T, Nagahama T, et al. Adverse reactions to azathioprine cannot be predicted by thiopurine S-methyltransferase genotype in Japanese patients with inflammatory bowel disease. J Gastroenterol Hepatol. 2009;24:1258–64.
Gearry RB, Barclay ML, Burt MJ, Collett JA, Chapman BA. Thiopurine drug adverse effects in a population of New Zealand patients with inflammatory bowel disease. Pharmacoepidemiol Drug Saf. 2004;13:563–7.
Palmieri O, Latiano A, Bossa F, Vecchi M, D'Inca R, Guagnozzi D, et al. Sequential evaluation of thiopurine methyltransferase, inosine triphosphate pyrophosphatase, and HPRT1 genes polymorphisms to explain thiopurines' toxicity and efficacy. Aliment Pharmacol Ther. 2007;26:737–45.
Yang SK, Hong M, Baek J, Choi H, Zhao W, Jung Y, et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat Genet. 2014;46:1017–20.
Kakuta Y, Naito T, Onodera M, Kuroha M, Kimura T, Shiga H, et al. NUDT15 R139C causes thiopurine-induced early severe hair loss and leukopenia in Japanese patients with IBD. Pharmacogenomics J. 2016;16:280–5.
Asada A, Nishida A, Shioya M, Imaeda H, Inatomi O, Bamba S, et al. NUDT15 R139C-related thiopurine leukocytopenia is mediated by 6-thioguanine nucleotide-independent mechanism in Japanese patients with inflammatory bowel disease. J Gastroenterol. 2016;51:22–9.
Tanaka Y, Kato M, Hasegawa D, Urayama KY, Nakadate H, Kondoh K, et al. Susceptibility to 6-MP toxicity conferred by a NUDT15 variant in Japanese children with acute lymphoblastic leukaemia. Br J Haematol. 2015;171:109–15.
Moriyama T, Nishii R, Andreu V, Yang W, Klussmann FA, Zhao X, et al. NUDT15 polymorphisms alter thiopurine metabolism and hematopoietic toxicity. Nat Genet. 2016;48:367–73.
Valerie NC, Hagenkort A, Page BD, Masuyer G, Rehling D, Carter M, et al. NUDT15 hydrolyzes 6-thio-deoxyGTP to mediate the anticancer efficacy of 6-thioguanine. Cancer Res. 2016;76:5501–11.
Akiyama S, Matsuoka K, Fukuda K, Hamada S, Shimizu M, Nanki K, et al. Long-term effect of NUDT15 R139C on hematologic indices in inflammatory bowel disease patients treated with thiopurine. J Gastroenterol Hepatol. 2019. https://doi.org/10.1111/jgh.14693.
Kakuta Y, Kawai Y, Okamoto D, Takagawa T, Ikeya K, Sakuraba H, et al. NUDT15 codon 139 is the best pharmacogenetic marker for predicting thiopurine-induced severe adverse events in Japanese patients with inflammatory bowel disease: a multicenter study. J Gastroenterol. 2018;53:1065–78.
Ban H, Andoh A, Tanaka A, Tsujikawa T, Sasaki M, Saito Y, et al. Analysis of thiopurine S-methyltransferase genotypes in Japanese patients with inflammatory bowel disease. Intern Med. 2008;47(19):1645–8.
Sato T, Takagawa T, Kakuta Y, Nishio A, Kawai M, Kamikozuru K, et al. NUDT15, FTO, and RUNX1 genetic variants and thiopurine intolerance among Japanese patients with inflammatory bowel diseases. Intest Res. 2017;15:328–37.
Moriyama T, Yang YL, Nishii R, Ariffin H, Liu C, Lin TN, et al. Novel variants in NUDT15 and thiopurine intolerance in children with acute lymphoblastic leukemia from diverse ancestry. Blood. 2017;130:1209–12.
Chao K, Wang X, Cao Q, Qian J, Wu K, Zhu X, et al. Combined detection of NUDT15 variants could highly predict thiopurine-induced leukopenia in Chinese patients with inflammatory bowel disease: a multicenter analysis. Inflamm Bowel Dis. 2017;23:1592–9.
Moriyama T, Nishii R, Lin TN, Kihira K, Toyoda H, Jacob N, et al. The effects of inherited NUDT15 polymorphisms on thiopurine active metabolites in Japanese children with acute lymphoblastic leukemia. Pharmacogenet Genomics. 2017;27:236–9.
Kim HT, Choi R, Won HH, Choe YH, Kang B, Lee K, et al. NUDT15 genotype distributions in the Korean population. Pharmacogenet Genomics. 2017;27:197–200.
Walker GJ, Harrison JW, Heap GA, Voskuil MD, Andersen V, Anderson CA, et al. Association of genetic variants in NUDT15 with thiopurine-induced myelosuppression in patients with inflammatory bowel disease. JAMA. 2019;321:773–85.
Kuriyama S, Yaegashi N, Nagami F, Arai T, Kawaguchi Y, Osumi N, et al. The tohoku medical megabank project: design and mission. J Epidemiol. 2016;26:493–511.
Reed GH, Kent JO, Wittwer CT. High-resolution DNA melting analysis for simple and efficient molecular diagnostics. Pharmacogenomics. 2007;8:597–608.
Yang JJ, Whirl-Carrillo M, Scott SA, Turner AJ, Schwab M, Tanaka Y, et al. Pharmacogene variation consortium gene introduction: NUDT15. Clin Pharmacol Ther. 2019;105:1091–4.
Liew M, Pryor R, Palais R, Meadows C, Erali M, Lyon E, et al. Genotyping of single-nucleotide polymorphisms by high-resolution melting of small amplicons. Clin Chem. 2004;50:1156–64.
Skrzypczak-Zielinska M, Borun P, Milanowska K, Jakubowska-Burek L, Zakerska O, Dobrowolska-Zachwieja A, et al. High-resolution melting analysis of the TPMT gene: a study in the Polish population. Genet Test Mol Biomark. 2013;17:153–9.
Skrzypczak-Zielinska M, Borun P, Bartkowiak-Kaczmarek A, Zakerska-Banaszak O, Walczak M, Dobrowolska A, et al. A simple method for TPMT and ITPA genotyping using multiplex HRMA for patients treated with thiopurine drugs. Mol Diagn Ther. 2016;20:493–9.
Fong WY, Ho CC, Poon WT. Comparison of direct sequencing, real-time PCR-high resolution melt (PCR-HRM) and PCR-restriction fragment length polymorphism (PCR-RFLP) analysis for genotyping of common thiopurine intolerant variant alleles NUDT15 c.415C%3eT and TPMT c.719A%3eG (TPMT*3C). Diagnostics (Basel, Switzerland). 2017;7(2):27.
Tsujimoto S, Osumi T, Uchiyama M, Shirai R, Moriyama T, Nishii R, et al. Diplotype analysis of NUDT15 variants and 6-mercaptopurine sensitivity in pediatric lymphoid neoplasms. Leukemia. 2018;32(12):2710.
Acknowledgments
We would like to thank all of the patients who participated in this study. This research was supported by AMED under Grant Number 18kk0305002 and 19ek0410056 to Y. Kakuta, and 16km0405205h0101 to M. Nagasaki. This work was supported in part by the Tohoku Medical Megabank Project (Special Account for Reconstruction from the Great East Japan Earthquake). Some of the computational resources were provided by the ToMMo supercomputer system.
Members of MENDEL study group [name and affiliation] are: Tetsuya Takagawa and Shiro Nakamura [Division of Internal Medicine, Department of Inflammatory Bowel Disease, Hyogo College of Medicine, Nishinomiya, Japan], Kentaro Ikeya and Hiroyuki Hanai [Centre for Gastroenterology and Inflammatory Bowel Disease Research, Hamamatsu South Hospital, Hamamatsu, Japan], Hirotake Sakuraba [Department of Gastroenterology and Hematology, Hirosaki University Graduate School of Medicine, Hirosaki, Japan], Atsushi Nishida and Akira Andoh [Department of Gastroenterology, Shiga University of Medical Science, Otsu, Japan], Shoko Nakagawa and Makoto Sasaki[Division of Gastroenterology, Department of Internal Medicine, Aichi Medical University School of Medicine, Aichi, Japan], Miki Miura and Tadakazu Hisamatsu [The Third Department of Internal Medicine, Kyorin University School of Medicine, Mitaka, Japan], Takahiko Toyonaga and Taku Kobayashi [Center for Advanced IBD Research and Treatment, Kitasato University Kitasato Institute Hospital, Tokyo, Japan], Kei Onodera and Hiroshi Nakase [Department of Gastroenterology and Hepatology, Sapporo Medical University School of Medicine, Sapporo, Japan], Masaru Shinozaki [Department of Surgery, IMSUT Hospital, the Institute of Medical Science, the University of Tokyo, Tokyo, Japan], Yoh Ishiguro [Department of Gastroenterology and Hematology, Hirosaki National Hospital, Hirosaki, Japan], Shinta Mizuno and Makoto Naganuma [Division of Gastroenterology and Hepatology, Department of Internal Medicine, Keio University School of Medicine, Tokyo, Japan], Masahiro Takahara and Sakiko Hiraoka [Department of Gastroenterology and Hepatology, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama, Japan], Shunichi Yanai and Takayuki Matsumoto[Division of Gastroenterology, Department of Internal Medicine, School of Medicine, Iwate Medical University, Morioka, Japan], Ryota Hokari [Division of Gastroenterology and Hepatology, Department of Internal Medicine, National Defense Medical College, Tokorozawa, Japan], Tomoo Nakagawa[Department of Gastroenterology, Graduate School of Medicine, Chiba University, Chiba, Japan], Hiroshi Araki [Division of Endscopy, Gifu University Hospital, Gifu, Japan], Satoshi Motoya [IBD Center, Sapporo-Kosei General Hospital, Sapporo, Japan], Shunji Ishihara and Naoki Oshima [Department of Internal Medicine II, Shimane University Faculty of Medicine, Shimane, Japan.], Takehiko Katsurada [Department of Gastroenterology and Hepatology, Graduate School of Medicine, Hokkaido University, Sapporo, Japan.], Yu Sasaki [Department of Gastroenterology, Yamagata University Faculty of Medicine, Yamagata, Japan.], Takafumi Otsuka [Division of Gastroenterology, Department of Internal Medicine, Kobe University Graduate School of Medicine, Hyogo, Japan.], Mikihiro Fujiya [Department of Medicine, Division of Gastroenterology and Hematology/Oncology, Asahikawa Medical University, Asahikawa, Japan.], Motoyuki Onodera [Department of Gastroenterology, Iwate Prefectural Isawa Hospital, Iwate, Japan.], Masakazu Nagahori and Katsuyoshi Matsuoka [Department of Gastroenterology and Hepatology, Tokyo Medical and Dental University, Tokyo, Japan.], Katsuhiro Arai [Division of Gastroenterology, National Center for Child Health and Development, Setagaya, Tokyo, Japan.], Yuichiro Sato [Department of Gastroenterology, Osaki Citizen Hospital, Osaki, Japan.], Mitsunori Noguchi [Noguchi Clinic, Sendai, Japan], Minoru Matsuura [Department of Gastroenterology and Hepatology, Graduate School of Medicine, Kyoto University, Japan.], Tomoaki Ishikawa, Hiroki Nakajima and Hiroshi Terasaki [LSI Medience Corporation, Japan], Yukiko Abe [G&G Science Co., Ltd.] and Mai Kato [MENDEL study secretariat].
Author information
Authors and Affiliations
Consortia
Contributions
YI, Y. Kakuta, DO and Y. Kinouchi designed the study. YI, Y. Kakuta, T. Naito, Y. Kawai, and MN acquired data. YI, Y. Kakuta, DO, T. Nakano, RI, RM, MK, HS, Y. Kanazawa, TK, and KN recruited patients. HK and NM managed the biobank samples. YI, Y. Kakuta, DO, Y. Kawai, KT and MN analyzed data. YI, Y. Kakuta, DO, Y. Kinouchi, YS and AM drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no disclosures to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the MENDEL study group are listed in acknowledgements section.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kakuta, Y., Izumiyama, Y., Okamoto, D. et al. High-resolution melt analysis enables simple genotyping of complicated polymorphisms of codon 18 rendering the NUDT15 diplotype. J Gastroenterol 55, 67–77 (2020). https://doi.org/10.1007/s00535-019-01638-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-019-01638-x