Abstract
Purpose
Exercise is important in lung cancer, yet most people do not meet the physical activity guidelines. The aim of this study was to characterise the views and experiences of participants with inoperable lung cancer who completed a home-based rehabilitation program.
Methods
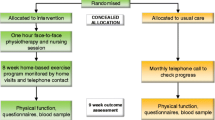
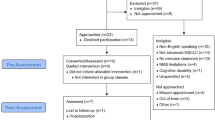
Ninety-two participants were recruited (45 intervention group [IG], 47 usual care). Individual semi-structured interviews were conducted with participants randomised to the IG of a trial of home-based exercise, behaviour change and symptom management. Data were independently coded by two researchers, cross-checked and analysed using content analysis with a summary of arising themes.
Results
Of the IG (25/45), 55% were interviewed: mean (SD) age 67 (13) years; male 52%; disease stage n (%) III = 9 (36), IV = 11 (44); radical treatment intent n (%) 13 (52). The majority of participants reported program benefits, both in the physical domain (reduced sedentary time and improved strength, fitness and function) and the mental domain (motivation to keep healthy, preventing boredom). Support to self-manage symptoms was well received and many participants reported increased confidence in managing their symptoms. Exercise enablers included having expert health professional support; motivation to be stronger and better prepared for future challenges; and having an achievable and familiar program that was monitored. Treatment side-effects, pain from comorbidities and the weather were exercise barriers. For the majority of participants the use of a Fitbit™ activity tracker, text message exercise reminders and an exercise diary helped to promote adherence.
Conclusions
This home-based rehabilitation program was acceptable to most participants with multiple benefits reported including improved fitness, motivation and ability to manage symptoms.

Similar content being viewed by others
References
Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL (2010) American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc 42(7):1409–1426. https://doi.org/10.1249/MSS.0b013e3181e0c112
Cormie P, Atkinson M, Bucci L, Cust A, Eakin E, Hayes S, McCarthy S, Murnane A, Patchell S, Adams D (2018) Clinical Oncology Society of Australia position statement on exercise in cancer care. Med J Aust 209(4):184–187. https://doi.org/10.5694/mja18.00199
Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM (2012) Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst 104(11):815–840. https://doi.org/10.1093/jnci/djs207
Buffart LM, Kalter J, Sweegers MG, Courneya KS, Newton RU, Aaronson NK, Jacobsen PB, May AM, Galvao DA, Chinapaw MJ, Steindorf K, Irwin ML, Stuiver MM, Hayes S, Griffith KA, Lucia A, Mesters I, van Weert E, Knoop H, Goedendorp MM, Mutrie N, Daley AJ, McConnachie A, Bohus M, Thorsen L, Schulz KH, Short CE, James EL, Plotnikoff RC, Arbane G, Schmidt ME, Potthoff K, van Beurden M, Oldenburg HS, Sonke GS, van Harten WH, Garrod R, Schmitz KH, Winters-Stone KM, Velthuis MJ, Taaffe DR, van Mechelen W, Kersten MJ, Nollet F, Wenzel J, Wiskemann J, Verdonck-de Leeuw IM, Brug J (2017) Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev 52:91–104. https://doi.org/10.1016/j.ctrv.2016.11.010
Cramp F, Byron-Daniel J (2012) Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev 11:CD006145. https://doi.org/10.1002/14651858.CD006145.pub3
Fuller JT, Hartland MC, Maloney LT, Davison K (2018) Therapeutic effects of aerobic and resistance exercises for cancer survivors: a systematic review of meta-analyses of clinical trials. Br J Sports Med 52(20):1311. https://doi.org/10.1136/bjsports-2017-098285
Mishra SI, Scherer RW, Snyder C, Geigle PM, Gotay C (2015) The effectiveness of exercise interventions for improving health-related quality of life from diagnosis through active cancer treatment. Oncol Nurs Forum 42(1):E33–E53. https://doi.org/10.1188/15.onf.e33-e53
Mustian KM, Alfano CM, Heckler C, Kleckner AS, Kleckner IR, Leach CR, Mohr D, Palesh OG, Peppone LJ, Piper BF, Scarpato J, Smith T, Sprod LK, Miller SM (2017) Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: a meta-analysis. J Am Med Assoc Oncol 3(7):961–968. https://doi.org/10.1001/jamaoncol.2016.6914
Cavalheri V, Granger C (2017) Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev 6:CD012020. https://doi.org/10.1002/14651858.CD012020.pub2
Crandall K, Maguire R, Campbell A, Kearney N (2014) Exercise intervention for patients surgically treated for non-small cell lung cancer (NSCLC): a systematic review. Surg Oncol 23(1):17–30. https://doi.org/10.1016/j.suronc.2014.01.001
Granger CL, McDonald CF, Parry SM, Oliveira CC, Denehy L (2013) Functional capacity, physical activity and muscle strength assessment of individuals with non-small cell lung cancer: a systematic review of instruments and their measurement properties. BioMed Central Cancer 13. https://doi.org/10.1186/1471-2407-13-135
Bade BC, Brooks MC, Nietert SB, Ulmer A, Thomas DD, Nietert PJ, Scott JB, Silvestri GA (2018) Assessing the correlation between physical activity and quality of life in advanced lung cancer. Integr Cancer Ther 17(1):73–79. https://doi.org/10.1177/1534735416684016
Granger CL, McDonald CF, Irving L, Clark RA, Gough K, Murnane A, Mileshkin L, Krishnasamy M, Denehy L (2014) Low physical activity levels and functional decline in individuals with lung cancer. Lung Cancer 83(2):292–299. https://doi.org/10.1016/j.lungcan.2013.11.014
Licker M, Karenovics W, Diaper J, Fresard I, Triponez F, Ellenberger C, Schorer R, Kayser B, Bridevaux PO (2017) Short-term preoperative high-intensity interval training in patients awaiting lung Cancer surgery: a randomized controlled trial. J Thorac Oncol 12(2):323–333. https://doi.org/10.1016/j.jtho.2016.09.125
Solheim TS, Laird BJA, Balstad TR, Stene GB, Bye A, Johns N, Pettersen CH, Fallon M, Fayers P, Fearon K, Kaasa S (2017) A randomized phase II feasibility trial of a multimodal intervention for the management of cachexia in lung and pancreatic cancer. J Cachexia Sarcopenia Muscle 8(5):778–788. https://doi.org/10.1002/jcsm.12201
Cooley ME (2000) Symptoms in adults with lung cancer. A systematic research review. J Pain Symptom Manag 19(2):137–153
Chambers SK, Dunn J, Occhipinti S, Hughes S, Baade P, Sinclair S, Aitken J, Youl P, O’Connell DL (2012) A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BioMed Central Cancer 12:184. https://doi.org/10.1186/1471-2407-12-184
Granger CL, Connolly B, Denehy L, Hart N, Antippa P, Lin KY, Parry SM (2017) Understanding factors influencing physical activity and exercise in lung cancer: a systematic review. Support Care Cancer 25(3):983–999. https://doi.org/10.1007/s00520-016-3484-8
Albrecht TA, Taylor AG (2012) Physical activity in patients with advanced-stage cancer: a systematic review of the literature. Clin J Oncol Nurs 16(3):293–300. https://doi.org/10.1188/12.cjon.293-300
Beaton R, Pagdin-Friesen W, Robertson C, Vigar C, Watson H, Harris SR (2009) Effects of exercise intervention on persons with metastatic cancer: a systematic review. Physiother Can 61(3):141–153. https://doi.org/10.3138/physio.61.3.141
Salakari MR, Surakka T, Nurminen R, Pylkkanen L (2015) Effects of rehabilitation among patients with advances cancer: a systematic review. Acta Oncol 54(5):618–628. https://doi.org/10.3109/0284186x.2014.996661
Heywood R, McCarthy AL, Skinner TL (2017) Safety and feasibility of exercise interventions in patients with advanced cancer: a systematic review. Support Care Cancer 25(10):3031–3050. https://doi.org/10.1007/s00520-017-3827-0
Kartolo A, Cheng S, Petrella T (2016) Motivation and preferences of exercise programmes in patients with inoperable metastatic lung cancer: a need assessment. Support Care Cancer 24(1):129–137. https://doi.org/10.1007/s00520-015-2767-9
Lowe SS, Watanabe SM, Baracos VE, Courneya KS (2010) Physical activity interests and preferences in palliative cancer patients. Support Care Cancer 18:1469–1475. https://doi.org/10.1007/s00520-009-0770-8
Karvinen KH, Vallance J, Walker PR (2016) Newly diagnosed lung cancer patients' preferences for and beliefs about physical activity prior to chemotherapy. Psychol Health Med 21(5):593–600. https://doi.org/10.1080/13548506.2016.1139739
Cheville AL, Rhudy L, Basford JR, Griffin JM, Flores AM (2017) How receptive are patients with late stage cancer to rehabilitation services and what are the sources of their resistance? Arch Phys Med Rehabil 98(2):203–210. https://doi.org/10.1016/j.apmr.2016.08.459
Edbrooke L, Aranda S, Granger CL, McDonald CF, Krishnasamy M, Mileshkin L, Irving L, Braat S, Clark RA, Gordon I, Denehy L (2017) Benefits of home-based multidisciplinary exercise and supportive care in inoperable non-small cell lung cancer - protocol for a phase II randomised controlled trial. BioMed Central Cancer 17(1):663. https://doi.org/10.1186/s12885-017-3651-4
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19(6):349–357. https://doi.org/10.1093/intqhc/mzm042
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A (2005) A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J 173(5):489–495. https://doi.org/10.1503/cmaj.050051
Onwuegbuzie AJ, Collins KM (2007) A typology of mixed methods sampling designs in social science research. Qual Rep 12(2):281–316
Philip J, Smith WB, Craft P, Lickiss N (1998) Concurrent validity of the modified Edmonton Symptom Assessment System with the Rotterdam Symptom Checklist and the Brief Pain Inventory. Support Care Cancer 6(6):539–541
Burke L, Miller M (2001) Phone interviewing as a means of data collection: lessons learned and practical recommendations. Forum: Qualitative Social Research 2 (2, Art. 7)
Hsieh H, Shanon S (2005) Three approaches to qualitative content analysis. Qual Health Res 15(9):1277–1288. https://doi.org/10.1177/1049732305276687
Bowen G (2008) Naturalistic inquiry and the saturation concept: a research note. Qual Res 8(1):137–152
Colinet B (2005) A new simplified comorbidity score as a prognostic factor in non-small-cell lung cancer patients: description and comparison with the Charlson’s index. Br J Cancer 93(10):1098–1105
Bandura A (1977) Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 84(2):191–215
Hoffman AJ, Brintnall RA (2017) A home-based exercise intervention for non-small cell lung cancer patients post-thoracotomy. Semin Oncol Nurs 33(1):106–117. https://doi.org/10.1016/j.soncn.2016.11.011
Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, Pitta F, Sewell L, Raskin J, Bourbeau J, Crouch R, Franssen FM, Casaburi R, Vercoulen JH, Vogiatzis I, Gosselink R, Clini EM, Effing TW, Maltais F, van der Palen J, Troosters T, Janssen DJ, Collins E, Garcia-Aymerich J, Brooks D, Fahy BF, Puhan MA, Hoogendoorn M, Garrod R, Schols AM, Carlin B, Benzo R, Meek P, Morgan M, Rutten-van Molken MP, Ries AL, Make B, Goldstein RS, Dowson CA, Brozek JL, Donner CF, Wouters EF (2013) An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 188(8):e13–e64. https://doi.org/10.1164/rccm.201309-1634ST
Adamsen L, Stage M, Laursen J, Rorth M, Quist M (2012) Exercise and relaxation intervention for patients with advanced lung cancer: a qualitative feasibility study. Scand J Med Sci Sports 22(6):804–815. https://doi.org/10.1111/j.1600-0838.2011.01323.x
Cheville AL, Dose AM, Basford JR, Rhudy LM (2012) Insights into the reluctance of patients with late-stage cancer to adopt exercise as a means to reduce their symptoms and improve their function. J Pain Symptom Manag 44(1):84–94. https://doi.org/10.1016/j.jpainsymman.2011.08.009
Lowe SS, Danielson B, Beaumont C, Watanabe SM, Courneya KS (2016) Physical activity interests and preferences of cancer patients with brain metastases: a cross-sectional survey. BioMed Central Palliative Care 15(1):7. https://doi.org/10.1186/s12904-016-0083-x
Leach HJ, Devonish JA, Bebb DG, Krenz KA, Culos-Reed SN (2015) Exercise preferences, levels and quality of life in lung cancer survivors. Support Care Cancer 23(11):3239–3247. https://doi.org/10.1007/s00520-015-2717-6
Groen WG, Kuijpers W, Oldenburg HS, Wouters MW, Aaronson NK, van Harten WH (2017) Supporting lung cancer patients with an interactive patient portal: feasibility study. JMIR Cancer 3(2):e10. https://doi.org/10.2196/cancer.7443
Huang CC, Kuo HP, Lin YE, Chen SC (2017) Effects of a web-based health education program on quality of life and symptom distress of initially diagnosed advanced non-small cell lung cancer patients: a randomized controlled trial. J Cancer Educ 34:41–49. https://doi.org/10.1007/s13187-017-1263-y
Tsai LL, McNamara RJ, Moddel C, Alison JA, McKenzie DK, McKeough ZJ (2017) Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR Study. Respirology (Carlton, Vic) 22(4):699–707. https://doi.org/10.1111/resp.12966
Acknowledgements
The authors would like to thank all participants who were interviewed for the study. In addition, we would like to thank Dr. Selina Parry, Ms. Lucy Bucci and Ms. Jennifer Jones for the research assistance they provided in developing the interview schedule and conducting the interviews.
Funding
This research was funded through a National Health and Medical Research Council project grant (APP1060484). Lara Edbrooke is the recipient of a Victorian Government Olivia Newton John Cancer Wellness and Research Centre Supportive Care PhD scholarship, through the Victorian Cancer Agency (ONJ16010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed were in accordance with the ethical standards of the Peter MacCallum Cancer Centre ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Edbrooke, L., Denehy, L., Granger, C.L. et al. Home-based rehabilitation in inoperable non-small cell lung cancer—the patient experience. Support Care Cancer 28, 99–112 (2020). https://doi.org/10.1007/s00520-019-04783-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04783-4