Abstract
Purpose
Many patients are hospitalised during the final phase of life, even though most prefer to receive care at home until the end. This study aimed to explore the reasons and characteristics of hospitalisation in the final 3 months of life for patients who died non-suddenly, with a comparison between cancer patients and non-cancer patients.
Methods
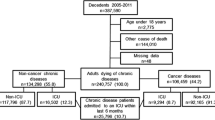
This study used a nationwide retrospective cross-sectional survey among Dutch general practitioners.
Results
Of the 317 hospitalised patients, 65 % had cancer. Most common reasons for hospitalisation in the final 3 months of life were respiratory symptoms (31 %), digestive symptoms (17 %), and cardiovascular symptoms (17 %). Seventy-three percent of patients experienced an acute episode before hospitalisation, and for 46 % of patients, their own GP initiated the hospitalisation. Compared to non-cancer patients, cancer patients were significantly more likely to be aged less than 80 (81 versus 46 %), were more likely to be hospitalised because of digestive symptoms (22 versus 7 %), were less likely to have a curative treatment goal before the last hospitalisation (6 versus 22 %) and were less likely to die in hospital (22 versus 49 %).
Conclusions
Respiratory problems were the most common reasons for hospitalisation in the group of patients as a whole. Digestive problems were a frequent reason for hospitalisation in cancer patients and cardiovascular symptoms in non-cancer patients. Hospitalisation can therefore be anticipated by monitoring these relatively common symptoms. Also, timely communication with the patient is recommended about their preferences for hospital or home treatment in the case of an acute episode.
Similar content being viewed by others
References
Abarshi E, Echteld M, Van den Bock L, Donker G, Deliens L, Onwuteaka-Philipsen B (2010) Transitions between care settings at the end of life in the Netherlands: results from a nationwide study. Palliat Med 24(2):166–174. doi:10.1177/0269216309351381
Van den Block L, Deschepper R, Drieskens K, Bauwens S, Bilsen J, Bossuyt N, Deliens L (2007) Hospitalisations at the end of life: using a sentinel surveillance network to study hospital use and associated patient, disease and healthcare factors. BMC Health Serv Res 7:69. doi:10.1186/1472-6963-7-69
Gomes B, Higginson IJ, Calanzani N, Cohen J, Deliens L, Daveson BA et al (2012) Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol 23(8):2006–2015. doi:10.1093/annonc/mdr602
Stajduhar KI, Allan DE, Cohen SR, Heyland DK (2008) Preferences for location of death of seriously ill hospitalized patients: perspectives from Canadian patients and their family caregivers. Palliat Med 22(1):85–88. doi:10.1177/0269216307084612
Choi J, Miyashita M, Hirai K, Sato K, Morita T, Tsuneto S, Shima Y (2010) Preference of place for end-of-life cancer care and death among bereaved Japanese families who experienced home hospice care and death of a loved one. Support Care Cancer 18(11):1445–1453. doi:10.1007/s00520-009-0767-3
Lawson B, Burge FI, Critchley P, McIntyre P (2006) Factors associated with multiple transitions in care during the end of life following enrollment in a comprehensive palliative care program. BMC Palliat Care 5:4. doi:10.1186/1472-684X-5-4
De Korte-Verhoef MC, Pasman HR, Schweitzer BP, Francke AL, Onwuteaka-Philipsen BD, Deliens L (2012) End-of-life hospital referrals by out-of-hours general practitioners: a retrospective chart study. BMC Fam Pract 13(1):89. doi:10.1186/1471-2296-13-89
Barbera L, Paszat L, Qiu F (2008) End-of-life care in lung cancer patients in Ontario: aggressiveness of care in the population and a description of hospital admissions. J Pain Symptom Manage Mar 35(3):267–274. doi:10.1016/j.jpainsymman.2007.04.019
Hanratty B, Holmes L, Lowson E, Grande G, Addington-Hall J, Payne S et al (2012) Older adults' experiences of transitions between care settings at the end of life in England: a qualitative interview study. J Pain Symptom Manage Jul 44(1):74–83. doi:10.1016/j.jpainsymman.2011.08.006
Lynn J, Adamson DM (2003) Living well at the end of life; adapting health care to serious chronic illness in old age. RAND, Santa Monica
Murray SA, Kendall M, Boyd K, Sheikh A (2005) Illness trajectories and palliative care. BMJ 330(7498):1007–1011
WONCA International Classification Committee (2005) ICPC-2-R:International classification of primary care, 2nd edn. Oxford University Press, Oxford
Hingstman L, Kenes RJ (2012) Cijfers uit de registratie van huisartsen, peiling 2011. (Numbers of the registration of General Practitioners 2011) Utrecht, NIVEL
Nivel http://www.nivel.nl/databank. Accessed 23 Sept 2013
WHO http://www.who.int/cancer/palliative/definition/en/. Accessed 2 Jul 2013
Abel J, Rich A, Griffin T, Purdy S (2009) End-of-life care in hospital: a descriptive study of all inpatient deaths in 1 year. Palliat Med 23(7):616–622. doi:10.1177/0269216309106460
Gott M, Frey R, Robinson J, Boyd M, O'Callaghan A, Richards N, Snow B (2013) The nature of, and reasons for, 'inappropriate' hospitalisations among patients with palliative care needs: a qualitative exploration of the views of generalist palliative care providers. Palliat Med 27(8):747–756
Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG (2012) Potentially avoidable hospitalizations of dually eligible Medicare and Medicaid beneficiaries from nursing facility and home- and community-based services waiver programs. J Am Geriatr Soc 60(5):821–829. doi:10.1111/j.1532-5415.2012.03920.x
De Roo ML, Leemans K, Claessen SJJ, Cohen J, Pasman HRW, Deliens L, Francke AL (2013) Quality indicators for palliative care: update of a systematic review. J Pain Symptom Manage. doi:10.1016/j.jpainsymman.2012.09.013
NHS National Institute for Health and Clinical Exellence (2011) Information for adults who use NHS end of life care services and their families and carers; NICE quality standard
Wowchuk SM, Wilson EA, Embleton L, Garcia M, Harlos M, Chochinov HM (2009) The palliative medication kit: an effective way of extending care in the home for patients nearing death. J Palliat Med 12(9):797–803. doi:10.1089=jpm.2009.0048
Schweitzer BP, Blankenstein N, Deliens L, van der Horst H (2009) Out-of-hours palliative care provided by GP co-operatives: availability, content and effect of transferred information. BMC Palliat Care 8:17. doi:10.1186/1472-684X-8-17
Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S et al (2007) Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 55(7):993–1000. doi:10.1111/j.1532-5415.2007.01234.x
Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Trice E et al (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300(14):1665–1673. doi:10.1001/jama.300.14.1665
Abarshi EA, Echteld MA, Van den Block L, Donker GA, Deliens L, Onwuteaka-Philipsen BD (2011) Recognising patients who will die in the near future: a nationwide study via the Dutch Sentinel Network of GPs. Br J Gen Pract 61(587):e371–e378. doi:10.3399/bjgp11X578052
Thoonsen B, Groot M, Engels Y, Prins J, Verhagen S, Galesloot C et al (2011) Early identification of and proactive palliative care for patients in general practice, incentive and methods of a randomized controlled trial. BMC Fam Pract 12:123. doi:10.1186/1471-2296-12-123.:123–12
Claessen SJ, Francke AL, Engels Y, Deliens L (2013) How do GPs identify a need for palliative care in their patients? An interview study. BMC Fam Pract 14(1):42. doi:10.1186/1471-2296-14-42
Acknowledgments
This study is funded by ZonMw, the Netherlands Organization for Health Research and Development. We thank the GPs for taking time to fill in the questionnaire.
Conflict of interest statement
The authors declare that there were no conflicts of interest in preparing this study and they have full control of all primary data. We allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ethics
A study protocol was approved by the Ethics Board of the VU University Medical Center Amsterdam.
Rights and permissions
About this article
Cite this article
De Korte-Verhoef, M.C., Pasman, H.R.W., Schweitzer, B.P.M. et al. Reasons for hospitalisation at the end of life: differences between cancer and non-cancer patients. Support Care Cancer 22, 645–652 (2014). https://doi.org/10.1007/s00520-013-2019-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-2019-9