Abstract
Objective
The Family Satisfaction with End-of-Life Care (FAMCARE) has been used widely among caregivers to individuals with cancer. The aim of this study was to evaluate the psychometric properties of this measure using item response theory (IRT).
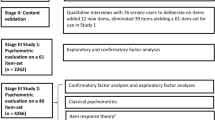
Methods
The analytic sample was comprised of caregivers to 1,983 patients with advanced cancer. Among the patients, 56 % were females, with mean age 59.9 years (s.d. = 11.8), 20 % were non-Hispanic Black. The majority were family members either living with (44 %) or not living with (35 %) the patient. Factor analyses and IRT were used to examine the dimensionality, information, and reliability of the FAMCARE.
Results
Although a bi-factor model fit the data slightly better than did a unidimensional model, the loadings on the group factors were very low. Thus, a unidimensional model appears to provide adequate representation for the item set. The reliability estimates, calculated along the satisfaction (theta) continuum, were adequate (>0.80) for all levels of theta for which subjects had scores. Examination of the category response functions from IRT showed overlap in the lower categories with little unique information provided; moreover, the categories were not observed to be interval. Based on these analyses, a three-response category format was recommended: very satisfied, satisfied, and not satisfied. Most information was provided in the range indicative of either dissatisfaction or high satisfaction.
Conclusions
These analyses support the use of fewer response categories and provide item parameters that form a basis for developing shorter-form scales. Such a revision has the potential to reduce respondent burden.


Similar content being viewed by others
References
Ringdal GI, Jordhoy MS, Kaasa S (2002) Family satisfaction with end-of-life care for cancer patients in a cluster randomized trial. J Pain Symptom Manag 4:53–63
Hearn J, Higginson IJ (1998) Do specialist palliative care teams improve outcomes for cancer patients? A systematic literature review. Palliat Med 12:317–332
Wilkinson EK, Salisbury C, Bosanquet N, Franks PJ, Kite S, Lorentzon M et al (1999) Patient and career preference for, and satisfaction with, specialist models of palliative care: a systematic literature review. Palliat Med 13:197–216
Hudson PL, Trauer T, Graham S, Grande G, Ewing G, Payne S et al (2010) A systematic review of instruments related to family caregivers of palliative care patients. Palliat Med 24:656–668
Andershed B (2006) Relatives in end-of-life care—part 1: a systematic review of the literature the five last years, January 1999–February 2004. J Clin Nurs 151:1158–1169
Milberg A, Strang P, Carlsson M, Borjesson S (2003) Advanced palliative home care: next-of-kin’s perspective. J Palliat Med 6:749–756
Williams AL, McCorkle R (2011) Cancer family caregivers during the palliative, hospice, and bereavement phases: a review of the descriptive psychosocial literature. Palliat Support Care 9:315–325
Dy SM, Shugarman LR, Lorenz KA, Mularski RA, Lynn J (2008) A systematic review of satisfaction with care at the end of life. J Am Geriatr Soc 56:124–129
McCusker J (1984) Development of scales to measure satisfaction and preferences regarding long-term and terminal care. Med Care 22:476–493
Morita T, Chihara S, Kashiwagi T (2002) A scale to measure satisfaction of bereaved family receiving inpatient palliative care. Palliat Med 16:141–150
Kristjanson LJ (1993) Validity and reliability testing of the FAMCARE Scale: measuring family satisfaction with advanced cancer care. Soc Sci Med 36:693–701
Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC et al (2004) Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 170:1795–1801
Ringdal GI, Jordhoy MS, Kaasa S (2003) Measuring quality of palliative care: psychometric properties of the FAMCARE Scale. Qual Life Res 12:167–176
Dudgeon DJ, Knott C, Eichholz M, Gerlach JL, Chapman C, Viola R et al (2008) Palliative Care Integration Project (PCIP) quality improvement strategy evaluation. J Pain Symptom Manag 35:573–582
Follwell M, Burman D, Le LW, Wakimoto K, Seccareccia D, Bryson J et al (2009) Phase II study of an outpatient palliative care intervention in patients with metastatic cancer. J Clin Oncol 27:206–213
Kristjanson LJ (1989) Quality of terminal care: salient indicators identified by families. J Palliat Care 5:21–30
Kristjanson LJ (1986) Indicators of quality of palliative care from a family perspective. J Palliat Care 1:8–17
Johnsen AT, Ross L, Petersen MA, Lund L, Groenvold M (2012) The relatives’ perspective on advanced cancer care in Denmark. A cross-sectional survey. Support Care Cancer 20:3179–3188
Carter GL, Lewin TJ, Gianacas L, Clover K, Adams C (2011) Caregiver satisfaction with out-patient oncology services: utility of the FAMCARE instrument and development of the FAMCARE-6. Support Care Cancer 19:565–572
Rodriguez KL, Bayliss NK, Jaffe E, Zickmund S, Sevick MA (2010) Factor analysis and internal consistency evaluation of the FAMCARE scale for use in the long-term care setting. Palliat Support Care 8:169–176
Aoun S, Bird S, Kristjanson LJ, Currow D (2010) Reliability testing of the FAMCARE-2 scale: measuring family career satisfaction with palliative care. Palliat Med 24:674–681
Lo C, Burman D, Hales S, Swami N, Rodin G, Zimmermann C (2009) The FAMCARE-Patient scale: measuring satisfaction with care of outpatients with advanced cancer. Eur J Cancer 45:3182–3188
Lord FM, Novick MB (1968) Statistical theories of mental test scores: with contributions by A. Birnbaum. Addison-Wesley Publishing Company, Reading
Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, Thissen D, Revicki DA, Weiss DJ, Hambleton RK, Liu H, Gershon R, Reise SP, Lai JS, Cella D, PROMIS Cooperative Group (2007) Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med Care 45(Suppl 1):S22–S31
Samejima F (1969) Estimation of latent ability using a response pattern of graded scores. Psychometricka Monograph Supplement 17. William Byrd, Richmond
Teresi J, Kleinman M, Ocepek-Welikson K (2000) Modern psychometric methods for detection of differential item functioning: application to cognitive assessment measures. Stat Med 19:1651–1683
Reise SP, Moore TM, Haviland MG (2010) Bifactor models and rotations: exploring the extent to which multidimensional data yield univocal scale scores. J Pers Assess 92:544–559
Schmid L, Leiman J (1957) The development of hierarchical factor solutions. Psychometrika 22:53–61
Rizopoulus D (2009) ltm: Latent Trait Models under IRT. http://cran.rproject.org/web/packages/ltm/index.html
Muthén LK, Muthén BO (1998–2010) M-PLUS users guide, sixth edition. Muthén and Muthén, Los Angeles
Sijtsma K (2009) On the use, the misuse, and the very limited usefulness of Cronbach’s alpha. Psychometrika 74:107–120
McDonald RP (2009) Test theory: a unified treatment. L. Erlbaum Associates, Mahwah
McDonald RP (1970) Theoretical foundations of principal factor analysis and alpha factor analysis. Br J Math Stat Psychol 23:1–21
Revelle W, Zinbarg RE (2009) Coefficient alpha, beta, omega, and the GLB: comments on Sitsma. Psychometrika 74:145–154
Cai L, Thissen D, du Toit SHC (2011) IRTPRO: flexible, multidimensional, multiple categorical IRT modeling [computer software]. Scientific Software International, Chicago
Fullam F, Garman AN, Johnson TJ, Hedberg EC (2009) The use of patient satisfaction surveys and alternative coding procedures to predict malpractice risk. Med Care 47:553–559
Acknowledgments
This project was funded by the National Cancer Institute, Grant #: 5R01CA116227-05. Support for these analyses was provided by the Claude Pepper Older Americans Independence Center: National Institute on Aging, P30, AG028741.
Conflict of Interest
The authors do not have a financial relationship with the sponsoring organization. The authors have full control of the primary data and can provide the data for a full review if requested.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 379 kb)
Rights and permissions
About this article
Cite this article
Teresi, J.A., Ornstein, K., Ocepek-Welikson, K. et al. Performance of the Family Satisfaction with the End-of-Life Care (FAMCARE) measure in an ethnically diverse cohort: psychometric analyses using item response theory. Support Care Cancer 22, 399–408 (2014). https://doi.org/10.1007/s00520-013-1988-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1988-z