Abstract
Objective
Many children with chronic kidney disease (CKD) exhibiting symptoms of poor appetite, gastro-oesophageal reflux and vomiting are reliant on enteral tube feeds (ETF) to achieve adequate nutritional intake. Following a successful renal transplant (RT), some of these symptoms may resolve and ETF then discontinued. There are only a few studies reporting the time taken to transition from ETF to complete oral feeding after transplantation. This study aimed to investigate the time taken to discontinue ETF following RT in children attending a large tertiary nephrology unit.
Methods
A retrospective review of medical and dietetic records between 1 January 2014 and 31 December 2017.
Results
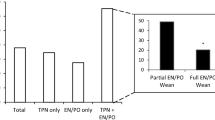
The study included 20 paediatric renal transplant recipients (70% male) aged 1 to 17 years. Seventy percent discontinued ETF at a median of 6 (0–70) weeks post-transplantation. Patients had ETF from a median of 0.45 (0–10.8) years of age, for a median of 3.9 (1.1–10.9) years prior to receiving a transplant. Four (20%) were referred to the Feeding and Eating Disorder team at a median of 20 (2–44) months post-renal transplantation. Mean body mass index (BMI) Z-score of 0.43 at 12 months pre-transplant was found to be significantly associated with shorter duration of ETF post-transplant (r = 0.8, p = 0.001).
Conclusions
Seventy percent of children stopped ETF by a median of 6 weeks post-renal transplant. A good nutritional status pre-transplant may reduce the duration of ETF following transplantation. Four children experienced behavioural feeding issues post-transplant and required further specialist support. Future multi-centre research is required to support these findings to provide a more robust indication of time to achieve full oral feeding.

Graphical abstract

Similar content being viewed by others
References
National Kidney Foundation (NKF) (2002) KDOQI Clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Part 4. Definition and classification of stages of chronic kidney disease [online]. Available at: https://kidneyfoundation.cachefly.net/professionals/KDOQI/guidelines_ckd/p4_class_g1.htm
Plumb L, Casula A, Pyart R, Evans KM, Inward C, Medcalf J, Marks SD (2020) The 21st UK renal registry annual report: a summary of analyses of paediatric data in 2017. Nephron. https://doi.org/10.1159/000504852
Ravelli AM, Ledermann SE, Bisset WM, Trompeter RS, Barratt TM, Milla PJ (1992) Foregut motor function in chronic renal failure. Arch Dis Child 67(11):1343–1347
Abitbol C, Chan JC, Trachtman H, Strauss J, Greifer I (1996) Growth in children with moderate renal insufficiency: measurement, evaluation, and treatment. J Paediatr 129(2):S3–S8
Mak RH, Cheung W, Cone RD, Marks DL (2005) Orexigenic and anorexigenic mechanisms in the control of nutrition in chronic kidney disease. Paediatr Nephrol 20(3):427–431
Rees L, Azocar M, Borzych D, Watson AR, Büscher A, Edefonti A, Bilge I, Askenazi D, Leozappa G, Gonzales C, van Hoeck K, Secker D, Zurowska A, Rönnholm K, Bouts AH, Stewart H, Ariceta G, Ranchin B, Warady BA, Schaefer F, International Paediatric Peritoneal Dialysis Network (IPPN) Registry (2011) Growth in very young children undergoing chronic peritoneal dialysis. J Am Soc Nephrol 22(12):2302–2012
Mak RH, Cheung W, Cone RD, Marks DL (2006) Leptin and inflammation-associated cachexia in chronic kidney disease. Kidney Int 69(5):794–797
Betts PR, Magrath G (1974) Growth pattern and dietary intake of children with chronic renal insufficiency. Br Med J 2(5912):189–193
Karlberg J, Schaefer F, Hennicke M, Wingen AM, Rigden S, Mehls O (1996) Early age-dependent growth impairment in chronic renal failure: European study Group for Nutritional Treatment of chronic renal failure in childhood. Paediatr Nephrol 10(3):283–287
Kidney Disease Outcomes Quality Initiative (KDOQI) (2009) Clinical practice guideline for nutrition in children with CKD: 2008 update. Am J Kidney Dis 53(3 Suppl 2):S1–S124
Zurowska AM, Fischbach M, Watson AR, Edefonti A, Stefanidis CJ, European Paediatric Dialysis Working Group (2013) Clinical practice recommendations for the care of infants with stage 5 chronic kidney disease (CKD5). Paediatr Nephrol 28(9):1739–1748
NHS England (2016) Confidentiality policy. Available from: https://www.england.nhs.uk/wpcontent/uploads/2016/12/confidentiality-policy-v3-1.pdf
General Data Protection Regulation (GDPR) (2018) Guide to the General Data Protection Regulation (GDPR) [online] Information Comissioner’s Office. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/711097/guide-to-the-generaldata-protection-regulation-gdpr-1-0.pdf
Health and Care Professions Council (HCPC) (2016) Standards of conduct, performance and ethics [online]. London:HCPC. Available from: https://www.hcpc-uk.org/assets/documents/10004EDFStandardsofconduct,performanceandethics.pdf
Pallant J (2016) SPSS survival manual, 6th edn. Open University Press, Maidenhead
Heumann C, Schomaker M, Shalabh (2016) Introduction to statistics and data analysis. Springer, Switzerland
The Children’s Hospital of Philadelphia Research Institute (CHOPRI) (2019) Paediatric Z-score calculator [online]. Available from: https://zscore.research.chop.edu/
Shaw V (2014) Clinical paediatric dietetics, 4th edn. John Wiley & Sons, Ltd., West Sussex
Scientific Advisory Committee on Nutrition (SACN) (2011) Dietary reference values for energy [online]. TSO, London Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/339317/SACN_Dietary_Reference_Values_for_Energy.pdf
Department of Health (DOH) (1991) Dietary reference values for food energy and nutrients for the United Kingdom. The Stationery Office, Norwich
Must A, Anderson SE (2006) Body mass index in children and adolescents: considerations for population-based applications. Int J Obes 30(4):590–594
Department of Health (DOH) (2009) Using the new UK–World Health Organization 0–4 years growth charts [online]. Department of Health. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215564/dh_127422.pdf
Ledermann S (2005) When should gastrostomy tubes be removed following successful renal transplantation? Paediatr Transplant 9(5):553–554
Kari JA, Gonzalez C, Ledermann SE, Shaw V, Rees L (2000) Outcome and growth of infants with severe chronic renal failure. Kidney Int 57(4):1681–1687
Wong H, Mylrea K, Cameron A, Manion I, Bass J, Feber J, Filler G (2005) Caregiver attitudes towards gastrostomy removal after renal transplantation. Paediatr Transplant 9(5):574–578
Pugh P, Watson AR (2006) Transition from gastrostomy to oral feeding following renal transplantation. Advances in Peritoneal Dialysis Conference on Peritoneal Dialysis 22:153–157
Warady BA, Kriley M, Belden B, Hellerstein S, Alan U (1990) Nutritional and behavioural aspects of nasogastric tube feeding in infants receiving chronic peritoneal dialysis. Advances in Peritoneal Dialysis Conference on Peritoneal Dialysis 6:265–268
Wilken M, Bartmann P, Dovey TM, Bagci S (2018) Characteristics of feeding tube dependency with respect to food aversive behaviour and growth. Appetite 123:1–6
van Arendonk KJ, Boyarsky BJ, Orandi BJ, James NT, Smith JM, Colombani PM, Segev DL (2014) National trends over 25 years in paediatric kidney transplant outcomes. Paediatrics 133(4):594–601
Westerterp-Plantenga MS, Lemmens SG, Westerterp KR (2012) Dietary protein – its role in satiety, energetics, weight loss and health. Br J Nutr 108(Suppl 2):105–112
Wilkin M, Cremer V, Berry J, Bartmann P (2013) Rapid home-based weaning of small children with feeding tube dependency: positive effects on feeding behaviour without deceleration of growth. Arch Dis Child 98(11):856–861
Brown J, Kim C, Lim A, Brown S, Desai H, Volker L, Katz M (2014) Successful gastrostomy tube weaning program using an intensive multidisciplinary team approach. J Paediatr Gastr Nutr 58(6):743–749
Acknowledgements
The authors would like to thank the following: the University of Plymouth as this was submitted as my Masters dissertation, Anne Payne who was my academic supervisor and provided guidance during the write up of my study, Vanessa Shaw for her invaluable guidance and knowledge within this field.
Funding
This project was financially supported by the National Institute for Health Research (NIHR) Biomedical Research Centres based at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This retrospective service evaluation was registered with the NHS Trust clinical audit and service evaluation team. The researcher also completed an ethics form via the Faculty of Health and Human Sciences Health Student Research Ethics Subcommittee at the University of Plymouth as part of their university project. There was no ethical risk as only routinely collected data was used and no additional information was collected outside of the patients’ health records.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PPTX 120 kb)
Rights and permissions
About this article
Cite this article
Khweir, S., McAlister, L. & Marks, S.D. Feeding patterns and outcomes of enterally tube fed paediatric kidney transplant recipients. Pediatr Nephrol 35, 2361–2367 (2020). https://doi.org/10.1007/s00467-020-04618-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04618-z