Abstract
Background
Patients with lesions in the posterosuperior (PS) segments of the liver have been considered poor candidates for laparoscopic liver resection (LLR). This study aims to compare short-term outcomes of LLR and open liver resections (OLR) in the PS segments.
Methods
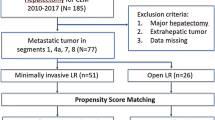
This multicenter study consisted of all patients who underwent LLR in the PS segments and all patients who underwent OLR in the PS segments between October 2011 and July 2016. Laparoscopic cases were case-matched with those who had an identical open procedure during the same period based on tumor location (same segment) and the Brisbane classification of the resection. Demographics, comorbid factors, perioperative outcomes, short-term outcomes, necessity of adjuvant chemotherapy, and the interval between surgery and initiation of adjuvant chemotherapy were compared between the two groups. Data were retrieved from a prospectively maintained electronic database.
Results
Both groups were comparable for age, sex, ASA score, maximum tumor diameter, and number of patients with additional liver resections outside the posterior segments. Operative time was similar in both groups (median 140 min; p = 0.92). Blood loss was less in the LLR-group (median: 150 vs. 300 ml in OLR-group). Median hospital stay was 6 days in both groups. There was no significant difference in postoperative complications (OLR-group: 31.4% vs. LLR-group: 25.7%; p = 0.60). There was no significant difference in R0 resections (LLR: 97.2 vs. 100% in OLR; p = 1.00). Tumor-free margins were less in the LLR group (LLR: 5 vs. 9.5 mm in OLR; p = 0.012). Patients undergoing LLR were treated with chemotherapy sooner compared to those undergoing OLR (41 vs. 56 days, p = 0.02).
Conclusion
This study suggests that laparoscopic parenchymal preserving liver resections in the PS segments can be performed with comparable short-term outcomes as similar OLR. The shorter interval to chemotherapy might provide long-term oncologic benefits in patients who underwent LLR.

Similar content being viewed by others
References
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker C-G, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey J-N, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, Mcmasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS (2009) The international position on laparoscopic liver surgery: the Louisville statement. Ann Surg 250:825–830
Cherqui D, Husson E, Hammoud R, Malassagne B, Stephan F, Bensaid S, Rotman N, Fagniez P-L (2000) Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 232:753–762
Dagher I, Belli G, Fantini C, Laurent A, Tayar C, Lainas P, Tranchart H, Franco D, Cherqui D (2010) Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg 211:16–23
Vigano L, Tayar C, Laurent A, Cherqui D (2009) Laparoscopic liver resection: a systematic review. J Hepato-Biliary-Pancreat Surg 16:410–421
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection—2,804 patients. Ann Surg 250:831–841
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246:385–392
Buell JF, Thomas MT, Rudich S, Marvin M, Nagubandi R, Ravindra KV, Brock G, McMasters KM (2008) Experience with more than 500 minimally invasive hepatic procedures. Ann Surg 248:475–486
Chen HY, Juan CC, Ker CG (2008) Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol 15:800–806
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629
Dulucq JL, Wintringer P, Sabilini C, Berticelli J, Mahajna A (2005) Laparoscopic liver resections: a single center experience. Surg Endosc 19:886–891
Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL (2003) Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg 138:763–769
D’Hondt M, Yoshihara E, Vansteenkiste F, Steelant PJ, Van Ooteghem B, Pottel H, Devriendt D, Van Rooy F (2016) Laparoscopic parenchymal preserving hepatic resections in semiprone position for tumors located in the posterosuperior segments. Langenbecks Arch Surg 401:255–262
Troisi RI, Montalti R, Van Limmen JG, Cavaniglia D, Reyntjens K, Rogiers X, De Hemptinne B (2014) Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB 16:75–82
von Heesen M, Schuld J, Sperling J, Grünhage F, Lammert F, Richter S, Schilling M, Kollmar O (2012) Parenchyma-preserving hepatic resection for colorectal liver metastases. Langenbecks Arch Surg 397:383–395
Gold JS, Are C, Kornprat P, Jarnagin WR, Gönen M, Fong Y, Dematteo RP, Blumgart LH, D’Angelica M (2008) Increased use of parenchymal-sparing surgery for bilateral liver metastases from colorectal cancer is associated with improved mortality without change in oncologic outcome: trends in treatment over time in 440 patients. Ann Surg 247:109–117
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C (2016) Parenchymal-sparing hepatectomy in colorectal liver metastasis improves salvageability and survival. Ann Surg 263:146–152
Montalti R, Tomassini F, Laurent S, Smeets P, Man M, Geboes K, Libbrecht L, Troisi R (2015) Impact of surgical margins on overall and recurrence-free survival in parenchymal-sparing laparoscopic liver resections of colorectal metastases. Surg Endosc 29(9):2736–2747
Abu Hilal M, Lodge P (2008) Pushing back the frontiers of resectability in liver cancer surgery. Eur J Surg Oncol 34:272–280
Tuttle TM, Curley SA, Roh MS (1997) Repeat hepatic resection as effective treatment for recurrent colorectal liver metastases. Ann Surg Oncol 4:125–130
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256(6):959–964
Cho JY, Han H-S, Yoon Y-S, Shin S-H (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144:32–38
Di Fabio F, Samim M, Di Gioia P, Godeseth R, Pearce NW, Abu Hilal M (2014) Laparoscopic major hepatectomies: clinical outcomes and classification. World J Surg 38:3169–3174
Gumbs AA, Gayet B (2008) Video: the lateral laparoscopic approach to lesions in the posterior segments. J Gastrointest Surg 12(7):1154
Ikeda T, Yonemura Y, Ueda N, Kabashima A, Shirabe K, Taketomi A, Yoshizumi T, Uchiyama H, Harada N, Ijichi H, Kakeji Y, Morita M, Tsujitani S, Maehara Y (2011) Pure laparoscopic right hepatectomy in the semiprone position using the intrahepatic Glissonian approach and a modified hanging maneuver to minimize intraoperative bleeding. Surg Today 41:1592–1598
Ikeda T, Mano Y, Morita K, Hashimoto N, Kayashima H, Masuda A, Ikegami T, Yoshizumi T, Shirabe K, Maehara Y (2013) Pure laparoscopic hepatectomy in semiprone position for right hepatic major resection. Hepato-Biliary-Pancreat Sci 20:145–150
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, Hasegawa Y, Katagiri T, Takagi C, Itano O, Kaneko H, Wakabayashi G (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepato-biliary-pancreat Sci 21:745–753
Xiang L, Xiao L, Li J, Chen J, Fan Y, Zheng S (2015) Safety and feasibility of laparoscopic hepatectomy for hepatocellular carcinoma in the posterosuperior liver segments. World J Surg 39:1202–1209
Chan FK, Cheng KC, Yeung YP (2014) Laparoscopic liver resection: lessons learnt after 100 cases. Hong Kong Med J 20:386–392
Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D (2009) The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg 250:772–782
Chang S, Laurent A, Tayar C, Karoui M, Cherqui D (2007) Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg 94:58–63
Lesurtel M, Cherqui D, Laurent A, Tayar C, Fagniez PL (2003) Laparoscopic versus open left lateral hepatic lobectomy: a case-control study. J Am Coll Surg 196:236–242
Wakabayashi G, Cherqui D, Geller DA, Han HS, Kaneko H, Buell JF (2014) Laparoscopic hepatectomy is theoretically better than open hepatectomy: preparing for the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepato-biliary-pancreat Sci 21:723–731
Makabe K, Nitta H, Takahara T, Hasegawa Y, Kanno S, Nishizuka S, Sasaki A, Wakabayashi G (2014) Efficacy of occlusion of hepatic artery and risk of carbon dioxide gas embolism during laparoscopic hepatectomy in a pig model. J Hepato-biliary-pancreat Sci 21:592–598
Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B (2009) Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 250:849–855
Iwahashi S, Shimada M, Utsunomiya T, Imura S, Morine Y, Ikemoto T, Arakawa Y, Mori H, Kanamoto M, Yamada S (2014) Laparoscopic hepatic resection for metastatic liver tumor of colorectal cancer: comparative analysis of short- and long-term results. Surg Endosc 28:80–84
Cheung TT, Poon RT, Yuen WK, Chok KS, Tsang SH, Yau T, Chan SC, Lo CM (2013) Outcome of laparoscopic versus open hepatectomy for colorectal liver metastases. ANZ J Surg 83:847–852
Guerron AD, Aliyev S, Agcaoglu O, Aksoy E, Taskin HE, Aucejo F, Miller C, Fung J, Berber E (2013) Laparoscopic versus open resection of colorectal liver metastasis. Surg Endosc 27:1138–1143
Montalti R, Berardi G, Laurent S, Sebastiani S, Ferdinande L, Libbrecht LJ, Smeets P, Brescia A, Rogiers X, de Hemptinne B, Geboes K, Troisi RI (2014) Laparoscopic liver resection compared to open approach in patients with colorectal liver metastases improves further resectability: oncological outcomes of a case-control matched-pairs analysis. Eur J Surg Oncol 40:536–544
Hammond JS, Muirhead W, Zaitoun AM, Cameron IC, Lobo DN (2012) Comparison of liver parenchymal ablation and tissue necrosis in a cadaveric bovine model using the Harmonic Scalpel, the LigaSure, the Cavitron Ultrasonic Surgical Aspirator and the Aquamantys devices. HPB 14:828–832
Viganò L, Procopio F, Cimino MM, Donadon M, Gatti A, Costa G, Del Fabbro D, Torzilli G (2016) Is tumor detachment from vascular structures equivalent to R0 resection in surgery for colorectal liver metastases? Ann Surg Oncol 23(4):1352–1360
Tohme S, Goswami J, Han K, Chidi AP, Geller DA, Reddy S, Gleisner A, Tsung A (2015) Minimally invasive resection of colorectal cancer liver metastases leads to an earlier initiation of chemotherapy compared to open surgery. J Gastrointest Surg 19:2199–2206
Malietzis G, Mughal A, Currie AC, Anyamene N, Kennedy RH, Athanasiou T, Jenkins J (2015) Factors implicated for delay of adjuvant chemotherapy in colorectal cancer: a meta-analysis of observational studies. Ann Surg Oncol 22:3793–3802
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mathieu D’Hondt, Esther Tamby, Isabelle Boscart, Simon Turcotte, Isabelle Parmentier, Hans Pottel, Réal Lapointe, Sander Ovaere, Franky Vansteenkiste, and Franck Vandenbroucke-Menu have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
D’Hondt, M., Tamby, E., Boscart, I. et al. Laparoscopic versus open parenchymal preserving liver resections in the posterosuperior segments: a case-matched study. Surg Endosc 32, 1478–1485 (2018). https://doi.org/10.1007/s00464-017-5835-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5835-z