Abstract
Background
Totally extraperitoneal (TEP) repair and transabdominal preperitoneal (TAPP) repair are the most used laparoscopic techniques for inguinal hernia treatment. However, many studies have shown that laparoscopic hernia repair compared with open hernia repair (OHR) may offer less pain and shorter convalescence. Few studies compared the clinical efficacy between TEP and TAPP technique. The purpose of this study is to provide a comparison between TEP and TAPP for inguinal hernia repair to show the best approach.
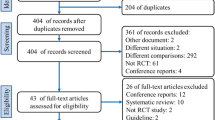
Methods
We performed an indirect comparison between TEP and TAPP techniques by considering only randomized, controlled trials comparing TEP with OHR and TAPP with OHR in a network meta-analysis. We considered the following outcomes: operative time, postoperative complications, hospital stay, postoperative pain, time to return to work, and recurrences.
Results
The two techniques improved some short outcomes (such as time to return to work) with respect to OHR. In the network meta-analysis, TEP and TAPP were equivalent for operative time, postoperative complications, postoperative pain, time to return to work, and recurrences, whereas TAPP was associated with a slightly longer hospital stay compared with TEP.
Conclusions
TEP and TAPP improved clinical outcomes compared with OHR, but the network meta-analysis showed that TEP and TAPP efficacy is equivalent. TAPP was associated with a slightly longer hospital stay compared with TEP.













Similar content being viewed by others
References
Testini M, Lissidini G, Poli E, Gurrado A, Lardo D, Piccinni G (2010) A single-surgeon randomized trial comparing sutures, N-butyl-2-cyanoacrylate and human fibrin glue for mesh fixation during primary inguinal hernia repair. Can J Surg 53:155–160
Vatansever U, Acunas B, Demir M, Karasalihoglu S, Ekuklu G, Ener S, Pala O (2002) Nucleated red blood cell counts and erythropoietin levels in high-risk neonates. Pediatr Int 44:590–595
Tolver MA, Strandfelt P, Rosenberg J, Bisgaard T (2011) Pain characteristics after laparoscopic inguinal hernia repair. Surg Endosc 25:3859–3864
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:188–199
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant AM (2005) Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev 1:CD004703
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Lumley T (2002) Network meta-analysis for indirect treatment comparisons. Stat Med 21:2313–2324
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J 339:b2535
Jansen JP, Fleurence R, Devine B, Itzler R, Barrett A, Hawkins N, Lee K, Boersma C, Annemans L, Cappelleri JC (2011) Interpreting indirect treatment comparisons and network meta-analysis for health-care decision making: report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices. Part 1. Value Health 14:417–428
Sutton A, Abrams K, Jones D, Sheldon T, Song F (2000) Methods for meta-analysis in medical research. Wiley, Chichester
Wallace BC, Schmid CH, Lau J, Trikalinos TA (2009) Meta-analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol 9:80
Bucher HC, Guyatt GH, Griffith LE, Walter SD (1997) The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol 50:683–691
Kouhia ST, Huttunen R, Silvasti SO, Heiskanen JT, Ahtola H, Uotila-Nieminen M, Kiviniemi VV, Hakala T (2009) Lichtenstein hernioplasty versus totally extraperitoneal laparoscopic hernioplasty in treatment of recurrent inguinal hernia: a prospective randomized trial. Ann Surg 249:384–387
Eklund A, Rudberg C, Smedberg S, Enander LK, Leijonmarck CE, Osterberg J, Montgomery A (2006) Short-term results of a randomized clinical trial comparing Lichtenstein open repair with totally extraperitoneal laparoscopic inguinal hernia repair. Br J Surg 93:1060–1068
Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LA, Rudberg CR (2009) Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg 249:33–38
Gokalp A, Inal M, Maralcan G, Baskonus I (2003) A prospective randomized study of Lichtenstein open tension-free versus laparoscopic totally extraperitoneal techniques for inguinal hernia repair. Acta Chir Belg 103:502–506
Colak T, Akca T, Kanik A, Aydin S (2003) Randomized clinical trial comparing laparoscopic totally extraperitoneal approach with open mesh repair in inguinal hernia. Surg Laparo Endo Per 13:191–195
Andersson B, Hallen M, Leveau P, Bergenfelz A, Westerdahl J (2003) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: a prospective randomized controlled trial. Surgery 133:464–472
Pawanindra L, Kajla RK, Chander J, Saha R, Ramteke VK (2003) Randomized controlled study of laparoscopic total extraperitoneal versus open Lichtenstein inguinal hernia repair. Surg Endosc 17:850–856
Suter M, Martinet O (2002) Postoperative pulmonary dysfunction after bilateral inguinal hernia repair: a prospective randomized study comparing the Stoppa procedure with laparoscopic total extraperitoneal repair (TEPP). Surg Laparosc Endosc Percutan Tech 12:420–425
Bringman S, Ramel S, Heikkinen TJ, Englund T, Westman B, Anderberg B (2003) Tension-free inguinal hernia repair: TEP versus mesh-plug versus Lichtenstein: a prospective randomized controlled trial. Ann Surg 237:142–147
Khoury N (1998) A randomized prospective controlled trial of laparoscopic extraperitoneal hernia repair and mesh-plug hernioplasty: a study of 315 cases. J Laparoendosc Adv Surg Technol A 8:367–372
Hallen M, Bergenfelz A, Westerdahl J (2008) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: long-term follow-up of a randomized controlled trial. Surgery 143:313–317
Mahon D, Decadt B, Rhodes M (2003) Prospective randomized trial of laparoscopic (transabdominal preperitoneal) vs. open (mesh) repair for bilateral and recurrent inguinal hernia. Surg Endosc 17:1386–1390
Sarli L, Iusco DR, Sansebastiano G, Costi R (2001) Simultaneous repair of bilateral inguinal hernias: a prospective, randomized study of open, tension-free versus laparoscopic approach. Surg Laparosc Endosc Percutan Tech 11:262–267
Picchio M, Lombardi A, Zolovkins A, Mihelsons M, La Torre G (1999) Tension-free laparoscopic and open hernia repair: randomized controlled trial of early results. World J Surg 23:1004–1009
Beets GL, Dirksen CD, Go PM, Geisler FE, Baeten CG, Kootstra G (1999) Open or laparoscopic preperitoneal mesh repair for recurrent inguinal hernia? A randomized controlled trial. Surg Endosc 13:323–327
Heikkinen TJ, Haukipuro K, Hulkko A (1998) A cost and outcome comparison between laparoscopic and Lichtenstein hernia operations in a day-case unit. A randomized prospective study. Surg Endosc 12:1199–1203
Butters M, Redecke J, Koninger J (2007) Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs. Br J Surg 94:562–565
Douek M, Smith G, Oshowo A, Stoker DL, Wellwood JM (2003) Prospective randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: five-year follow-up. Br Med J 326:1012–1013
Hamza Y, Gabr E, Hammadi H, Khalil R (2010) Four-arm randomized trial comparing laparoscopic and open hernia repairs. Int J Surg 8:25–28
Pokorny H, Klingler A, Schmid T, Fortelny R, Hollinsky C, Kawji R, Steiner E, Pernthaler H, Függer R, Scheyer M (2008) Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized multicenter trial. Hernia 12:385–389
Gunal O, Ozer S, Gurleyik E, Bahcebasi T (2007) Does the approach to the groin make a difference in hernia repair? Hernia 11:429–434
Dedemadi G, Sgourakis G, Karaliotas C, Christofides T, Kouraklis G (2006) Comparison of laparoscopic and open tension-free repair of recurrent inguinal hernias: a prospective randomized study. Surg Endosc 20:1099–1104
Heikkinen T, Bringman S, Ohtonen P, Kunelius P, Haukipuro K, Hulkko A (2004) Five-year outcome of laparoscopic and Lichtenstein hernioplasties. Surg Endosc 18:518–522
Bringman S, Blomqvist P (2005) Intestinal obstruction after inguinal and femoral hernia repair: a study of 33,275 operations during 1992–2000 in Sweden. Hernia 9:178–183
Song F, Loke YK, Walsh T, Glenny AM, Eastwood AJ, Altman DG (2009) Methodological problems in the use of indirect comparisons for evaluating healthcare interventions: survey of published systematic reviews. Br Med J 338:b1147
Disclosures
The authors have no conflict of interest to declare. This study was funded with structural funds of the authors’ institutions, which are public institutions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bracale, U., Melillo, P., Pignata, G. et al. Which is the best laparoscopic approach for inguinal hernia repair: TEP or TAPP? A systematic review of the literature with a network meta-analysis. Surg Endosc 26, 3355–3366 (2012). https://doi.org/10.1007/s00464-012-2382-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2382-5