Abstract
Background
Because the most suitable management of subclinical Cushing syndrome (SCS, which involves hypersecretion of cortisol without clinically evident disease) still is undefined, the current study aimed to compare retrospectively the outcome for a cohort of patients treated by medical therapy or laparoscopic adrenalectomy (LA).
Methods
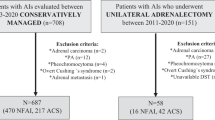
Over a 12-year period, 47 patients with SCS have been treated by means of LA (19 patients, group A) or medical therapy (28 patients, group B). Group A consisted of 15 women and 4 men with a mean age of 54.8 years. Eight patients had a left adrenal mass, whereas nine had a right adrenal mass, and one patient had bilateral lesion. Group B was composed of 18 women and 10 men with a mean age of 57.8 years. Of these patients, 14 had a left adrenal lesion, 12 had a right adrenal lesion, and 1 had bilateral lesion. The patients were followed up for a mean 4 years (range, 1–11 years) by both an endocrinologist and a surgeon.
Results
In group A, hypertension improved for 66.3% of the patients; body mass index (BMI) decreased for 47.4%; and hyperlipidemia based on high-density lypoproteins (HDL) cholesterol, total cholesterol ratio, and triglyceridemic concentration improved for 63.2% of the patients. No changes in bone parameters were seen after surgery in SCS patients with osteoporosis. Some patients in group B, during their long-term medical therapy, experienced worsening hypertension (14.2%), hyperlipidemia (17.8%), and diabetes mellitus (8%).
Conclusions
This retrospective study focused on a cohort of patients with SCS. Their medium long-term follow-up evaluation showed that LA is better than medical therapy for treating this condition, especially by reducing the cardiovascular risk (hypertension-hyperlipidemia).





Similar content being viewed by others
References
Aron DC (2001) The adrenal incidentaloma: disease of modern technology and public health problem. Rev End Metab Disord 2:335–342
Guerrieri M, De Sanctis A, Crosta F, Arnaldi G, Boscaro M, Lezoche G, Campagnacci R (2007) Adrenal incidentaloma: surg update. J Endocrinol Invest 30:200–204
National Institute of Health (NIH) (2002) NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consensus and State-of-the-Science Statements 19:1–23
Reincke M (2000) Subclinical Cushing’s syndrome. Endocrinol Metab Clin North Am 29:43–56
Sippel RS, Chen H (2004) Subclinical Cushing’s syndrome in adrenal incidentalomas. Surg Clin North Am 84:875–885
Terzolo M, Reimondo G, Bovio (2004) Subclinical Cushing’s syndrome. Pituitary 7:217–224
Fujii H, Kamide K, Miyake O, Abe T, Nagai M, Nakahama H, Horio T, Takiuchi S, Okuyama A, Yutami C, Kawano Y (2005) Primary aldosteronism combined with preclinical Cushing’s syndrome in an elderly patient. Circ J 69:1425–1427
Toniato A, Merante-Boschin I, Opocher G, Pelizzo MR, Schiavi F, Ballotta S (2009) Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Ann Surg 249:388–391
Reincke M, Nieke J, Krestin G, Saeger J, Allolio B, Winkelmann W (2007) Preclinical Cushing’s syndrome in adrenal “incidentalomas”: comparison with adrenal Cushing’s syndrome. J Clin Endocrinol Metab 75:826–832
Pivonello R, De Martino MC, De Leo M, Tauchemanová L, Fagiano A, Lombardi G, Colao A (2007) Cushing’s syndrome: aftermath of the cure. Arq Bras Endocrinol Metab 51/8:1381–1391
Tessier DJ, Iglesias R, Chapman WC, Kercher K, Matthews BD, Gorden DL, Brunt LM (2009) Previously unreported high-grade complications of adrenalectomy. Surg Endosc 23(1):97–102
Ogilvie J, Duh Q (2005) New approaches to the minimally invasive treatment of adrenal lesions. Cancer J 11:64–72
Kwock K, Ng C, Chung Yau L (2003) Applicability and outcome of laparoscopic adrenalectomy. Asian J Surg 26:71–75
Jaap H, Bonjer H, Sorm V, Berends FJ, Kazemier E, Steyerberg EW, Van. De Harder W, Bruining HA (2000) Endoscopic retroperitoneal adrenalectomy lessons from 111 consecutive cases. Ann Surg 232:796–803
Gagner M, Pomp A, Heniford BT, Pharand D, Lacroix A (1997) Laparoscopic adrenalectomy lessons learned from 100 consecutive procedures. Ann Surg 226:238–247
Bjornsson B, Birgisson G, Oddsdottir M (2008) Laparoscopic adrenalectomies: a nationwide single-surgeon experience. Surg Endosc 22:622–626
Lezoche E, Guerrieri M, Crosta F, De Sanctis A, Baldarelli M, Lezoche G, Campagnacci R (2008) Perioperative results of 214 laparoscopic adrenalectomy by anterior transperitoneal approach. Surg Endosc 22:522–526
Thompson SK, Hayman VA, Ludlam WH, Deveney WC, Loriaux DL, Sheppard BC (2007) Improved quality of life after bilateral laparoscopic adrenalectomy for Cushing’s disease: 10 years of experience. Ann Surg 245:790–794
Sanjai Bhat H, Balagopal Nair T, Sukumar S, Saheed CSM, Mathew G, Ginil Kumar P (2007) Laparoscopic adrenalectomy is feasible for large adrenal masses >6 cm. Asian J Surg 30:52–56
Perretta S, Campagnacci R, Guerrieri M, Paganini AM, De Sanctis A, Lezoche E (2005) Submesocolic access in laparoscopic left adrenalectomy. Surg Endosc 19:977–980
Guerrieri M, Crosta F, De Sanctis A, Baldarelli M, Lezoche G, Campagnacci R (2008) Electrothermal bipolar vessel system (EBVS) use in laparoscopic adrenalectomy: a prospective study. Surg Endosc 22:141–145
Lezoche E, Guerrieri M, Crosta F, Baldarelli M, Lezoche G, Campagnacci R (2008) Flank approach vs anterior submesocolic access in left laparoscopic adrenalectomy: a prospective randomized study. Surg Endosc 22:237–238
Disclosures
Mario Guerrieri, Roberto Campagnacci, Andrea Patrizi, Chiara Romiti, Giorgio Arnaldi, and Marco Boscaro, have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guerrieri, M., Campagnacci, R., Patrizi, A. et al. Primary adrenal hypercortisolism: minimally invasive surgical treatment or medical therapy? A retrospective study with long-term follow-up evaluation. Surg Endosc 24, 2542–2546 (2010). https://doi.org/10.1007/s00464-010-1000-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1000-7