Abstract
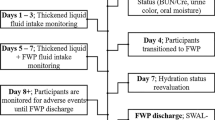
The benefit of water protocols for individuals with thin liquid aspiration remains controversial, with mixed findings from a small number of randomized controlled trials (RCTs). This study aimed to contribute to the evidence of the effectiveness of water protocols with a particular emphasis on health outcomes, especially hydration. An RCT was conducted with patients with known thin liquid aspiration post stroke randomized to receiving thickened liquids only or a water protocol. For the 14 participants in rehabilitation facilities whose data proceeded to analysis, there was no difference in the total amount of beverages consumed between the water protocol group (mean = 1103 ml per day, SD = 215 ml) and the thickened liquids only group (mean = 1103 ml, SD = 247 ml). Participants in the water protocol group drank on average 299 ml (SD 274) of water but offset this by drinking less of the thickened liquids. Their hydration improved over time compared with participants in the thickened liquids only group, but differences between groups were not significant. Twenty-one percent of the total sample was diagnosed with dehydration, and no participants in either group were diagnosed with pneumonia. There were significantly more diagnoses of urinary tract infection in the thickened liquids only group compared to the water protocol group (χ 2 = 5.091, p = 0.024), but no differences between groups with regard to diagnoses of dehydration (χ 2 = 0.884, p = 0.347) or constipation (χ 2 = 0.117, p = 0.733). The findings reinforce evidence about the relative safety of water protocols for patients in rehabilitation post stroke and provide impetus for future research into the potential benefits for hydration status and minimizing adverse health outcomes.



Similar content being viewed by others
References
Martino R, Foley NC, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;30(4):744–8.
Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: ProEd; 1998.
Bulow M, Olsson R, Ekberg O. Videoradiographic analysis of how carbonated thin liquids and thickened liquids affect the physiology of swallowing in subjects with aspiration on thin liquids. Acta Radiol. 2003;44:366–72.
Kuhlemeier KV, Palmer JB, Rosenberg D. Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia. 2001;16:119–22.
Mertz Garcia J, Chambers E, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol. 2005;14:4–13.
Huckabee M, Pelletier C. Management of adult neurogenic dysphagia. San Diego: Singular; 1999.
Hamlet S, Choi J, Zormeier M, Shamsa F, Stachler R, Muz J. Normal adults swallowing of liquid and viscous material: scintigraphic data on bolus transit and oropharyngeal residues. Dysphagia. 1996;11:41–7.
Langmore SE, Terpenning MS, Schork A, Chen Y, Murray J, Lopatin D, Loesche W. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998;13:69–81.
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665–71.
Colodny N. Dysphagic independent feeders’ justifications for noncompliance with recommendations by a speech-language pathologist. Am J Speech Lang Pathol. 2005;14(1):61–70.
Mertz-Garcia J, Chambers E, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol. 2005;14(1):4–13.
King J, Ligman K. Patient noncompliance with swallowing recommendations: reports from speech-language pathologists. Contemp Issues in Commun Sci Disord. 2011;38:53–60.
Clavé P, De Kraa M, Arreola V, Girvent M, Farre R, Palomera E, Serra-Prat M. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24(9):1385–94.
Steele CM, Huckabee M. The influence of orolingual pressure on the timing of pharyngeal pressure events. Dysphagia. 2007;22(1):30–6.
Steele CM, Alsanei WA, Ayanikalath S, Barbon CEA, Chen J, Cichero JAY, Coutts K, Dantas RO, Duivestein J, Giosa L. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2014;30(1):2–26.
Schmidt J, Holas M, Halvorson K, Reding M. Videofluoroscopic evidence of aspiration predicts pneumonia and death but not dehydration following stroke. Dysphagia. 1994;9(1):7–11.
Goulding R, Bakheit A. Evaluation of the benefits of monitoring fluid thickness in the dietary management of dysphagic stroke patients. Clin Rehabil. 2000;14:119–24.
Foley N, Teasell R, Salter K, Kruger E, Martino R. Dysphagia treatment post stroke: a systematic review of randomised controlled trials. Age Ageing. 2008;37(3):258–64.
Cichero JAY. Thickening agents used for dysphagia management: effect on bioavailability of water, medication and feelings of satiety. Nutr J. 2013;12(54):1.
Hill RJ, Dodrill P, Bluck LJ, Davies PS. A novel stable isotope approach for determining the impact of thickening agents on water absorption. Dysphagia. 2010;25(1):1–5.
Sharpe K, Ward L, Cichero JAY, Sopade P, Halley P. Thickened fluids and water absorption in rats and humans. Dysphagia. 2007;22:193–203.
Institute of Medicine of the National Academies. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: National Academies Press; 2004.
National Health and Medical Research Council (2003) Dietary guidelines for Australian adults. A guide to healthy eating. Commonwealth of Australia, Canberra, ACT.
Vivanti AP, Campbell KL, Suter MS, Hannan-Jones MT, Hulcombe JA. Contribution of thickened drinks, food and enteral and parenteral fluids to fluid intake in hospitalised patients with dysphagia. J Hum Nutr Diet. 2009;22(2):148–55.
Whelan K. Inadequate fluid intakes in dysphagic acute stroke. Clin Nutr. 2001;20(5):423–8.
Patch CS, Mason S, Curcio-Borg F, Tapsell LC. Thickened fluids: factors affecting wastage. Adv Speech Lang Pathol. 2003;5:73–7.
Murray J, Miller M, Doeltgen S, Scholten I. Intake of thickened liquids by hospitalized adults with dysphagia after stroke. Int J Speech Lang Pathol. 2014;16(5):486–94.
Finestone HM, Foley NC, Woodbury MG, Greene-Finestone L. Quantifying fluid intake in dysphagic stroke patients: a preliminary comparison of oral and non-oral strategies. Arch Phys Med Rehabil. 2001;82:1744–6.
Panther K. The Frazier free water protocol. Perspect Swallowing Swallowing Disord (Dysphagia). 2005;14(1):4–9.
Carlaw C, Finlayson H, Beggs K, Visser T, Marcoux C, Coney D, Steele CM. Outcomes of a pilot water protocol project in a rehabilitation setting. Dysphagia. 2012;27:297–306.
Karagiannis M, Chivers L, Karagiannis T. Effects of oral intake of water in patients with oropharyngeal dysphagia. BMC Geriatrics. 2011;11(9):1.
Garon BR, Engle M, Ormiston C. A randomized control study to determine the effects of unlimited oral intake of water in patients with identified aspiration. J Neurol Rehabil. 1997;11:139–48.
State University of New York at Buffalo. Guide for the uniform data set for medical rehabilitation (Adult FIM). version 4.0 edn. Buffalo: State University of New York; 1993.
Perry A, Skeat J (2004) AusTOMs for Speech Pathology. Melbourne: La Trobe University, ISBN 1-920948-54-6.
Hughes TAT, Wiles CM. Clinical measurement of swallowing in health and in neurogenic dysphagia. Q J Med. 1996;89:109–16.
Chalmers JM, King PL, Spencer AJ, Wright FA, Carter KD. The oral health assessment tool—validity and reliability. Aust Dent J. 2005;50:191–9.
Rosenbek J, Robbins J, Roecker E, Coyle J, Wood J. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Atherton M, Bellis-Smith N, Cichero J, Suter M. Texture-modified foods and thickened fluids as used for individuals with dysphagia: Australian standardised labels and definitions. Nutr Diet. 2007;64(2 Supp):s53–76.
Panther K (2003) The Frazier Rehab Institute Water Protocol. http://www.kentuckyonehealth.org/frazier-water-protocol. Accessed 29 Jan 2014.
South Australian Dental Service (2004) Oral health protocols for residential aged care facilities. http://www.sadental.sa.gov.au/.
Chidester JC, Spangler AA. Fluid intake in the institutionalized elderly. J Am Diet Assoc. 1997;97(1):23–30.
Rowat A, Graham C, Dennis M. Dehydration in hospital-admitted stroke patients: detection, frequency, and association. Stroke. 2012;43(3):857–9.
Leibovitz A, Baumoehl Y, Lubart E, Yaina A, Platinovitz N, Segal R. Dehydration among long-term care elderly patients with oropharyngeal dysphagia. Gerontology. 2007;53(4):179–83.
IBM Corp. (2013) IBM SPSS Statistics for Windows, Version 22.0. IBM Corp., Armonk.
National Stroke Foundation (2010) National Stroke Audit Rehabilitation Services 2010. Melbourne.
Kleim JA, Jones TA. Principles of experience-dependent neuroplasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51:S225.
Robbins J, Butler S, Daniels SK, Gross R, Langmore SE, Lazarus CL, Martin-Harris B, McCabe D, Musson N, Rosenbek JC. Swallowing and dysphagia rehabilitation: translating principles of neural plasticity into clinically oriented evidence. J Speech Lang Hear Res. 2008;51(1):S276–300.
Murray J, Doeltgen S, Miller M, Scholten I. A survey of thickened fluid prescribing and monitoring practices of Australian health professionals. J Eval Clin Pract. 2014;20(5):596–600.
Smithard DG, O’Neill PA, England RE, Park CL, Wyatt R, Martin DF, Morris J. The natural history of dysphagia following a stroke. Dysphagia. 1997;12(4):188–93.
Acknowledgments
The authors gratefully acknowledge the staff of the participating rehabilitation centres for their invaluable assistance during the data collection process.
Funding
This research was supported by the Royal Adelaide Hospital/Institute of Medical and Veterinary Science Clinical Research Grant for Allied Health, Nursing and Pharmacy [January 2009] and a Clinical Research Development Grant awarded to the first author by the National Stroke Foundation, Australia [dated 15th December 2011].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None declared.
Rights and permissions
About this article
Cite this article
Murray, J., Doeltgen, S., Miller, M. et al. Does a Water Protocol Improve the Hydration and Health Status of Individuals with Thin Liquid Aspiration Following Stroke? A Randomized Controlled Trial. Dysphagia 31, 424–433 (2016). https://doi.org/10.1007/s00455-016-9694-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9694-x