Abstract
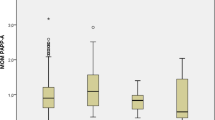
Small for gestational age preterm are at increased risk for future metabolic syndrome. Early indication for the disrupted metabolism may be found in the perinatal period. We aimed to evaluate whether small for gestational age preterm infants are at increased risk for hypertriglyceridemia when treated with lipid emulsions, and to investigate the association between triglyceride levels and morbidity. Small for gestational age infants ≤ 34 weeks’ gestation age born during 2013–2016 were matched and compared with appropriate for gestational age counterparts. Triglyceride concentration > 250 mg/dL during treatment with parenteral nutrition was considered high. The study included 71 pairs of preterm infants. Hypertriglyceridemia was documented among 22.5% of the small for gestational age infants vs. 5.6% of the appropriate for gestational age infants (p = 0.007). Mean triglyceride levels were 194.4 ± 192.3 mg/dL and 99.9 ± 82.8 mg/dL, respectively (p < 0.001). Small for gestational age was predictive of hypertriglyceridemia (OR = 6.41; 95% CI 1.8–22.9). No significant association was found between triglyceride levels and morbidities in multivariate analysis.
Conclusion: Small for gestational age preterm infants receiving lipid emulsions might be at a higher risk for hypertriglyceridemia. Routine monitoring of triglyceride levels will enable identification of the necessity for a slower increase in lipid emulsion therapy.
What is Known: • Moderate and very preterm infants are routinely treated with lipid emulsions. • Small for gestational age (SGA) infants may have different metabolism, as they demonstrate higher risk for metabolic syndrome. | |
What is New: • • SGA infants had a higher mean triglyceride level and more commonly had early hypertriglyceridemia (triglycerides > 250 mg/dL) compared with appropriate for gestational age infants treated with the same intravenous lipid dose. Small for gestational age was predictive of hypertriglyceridemia. • No significant association was found between triglyceride levels and morbidities in multivariate analysis. |

Similar content being viewed by others
Abbreviations
- AGA:
-
Appropriate-for-gestational-age
- BPD:
-
Bronchopulmonary dysplasia
- BW:
-
Birth weight
- CO:
-
ClinOleic
- EUGR:
-
Extrauterine growth retardation
- GA:
-
Gestational age
- IUGR:
-
Intrauterine growth restriction
- IVH:
-
Intraventricular hemorrhage
- NEC:
-
Necrotizing enterocolitis
- NICU:
-
Neonatal intensive care unit
- PDA:
-
Patent ductus arteriosus
- PVL:
-
Periventricular leukomalacia
- ROP:
-
Retinopathy of prematurity
- SGA:
-
Small for gestational age
- TG:
-
Triglycerides
- TPN:
-
Total parenteral nutrition
References
Lapillonne A, Mis NF, Goulet O, van den Akker CHP, Wu J, Koletzko B, Braegger C, Bronsky J, Cai W, Campoy C, Carnielli V, Darmaun D, Decsi T, Domellöf M, Embleton N, Fewtrell M, Mis NF, Franz A, Goulet O, Hartman C, Hill S, Hojsak I, Iacobelli S, Jochum F, Joosten K, Kolaček S, Koletzko B, Ksiazyk J, Lapillonne A, Lohner S, Mesotten D, Mihályi K, Mihatsch WA, Mimouni F, Mølgaard C, Moltu SJ, Nomayo A, Picaud JC, Prell C, Puntis J, Riskin A, De Pipaon MS, Senterre T, Shamir R, Simchowitz V, Szitanyi P, Tabbers MM, Van Den Akker CHB, Van Goudoever JB, Van Kempen A, Verbruggen S, Wu J, Yan W (2018) ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition. Lipids Clin Nutr. https://doi.org/10.1016/j.clnu.2018.06.946
Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R 1. Guidelines on paediatric parenteral nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), supported by the European Society of Paedia. J Pediatr Gastroenterol Nutr 41 Suppl 2(2005):S1–S87. https://doi.org/10.1097/01.mpg.0000181841.07090.f4
Vlaardingerbroek H, Vermeulen MJ, Rook D, Van Den Akker CHP, Dorst K, Wattimena JL, Vermes A, Schierbeek H, Van Goudoever JB (2013) Safety and efficacy of early parenteral lipid and high-dose amino acid administration to very low birth weight infants. J Pediatr 163:638–644.e5. https://doi.org/10.1016/j.jpeds.2013.03.059
Vayssière C, Sentilhes L, Ego A, Bernard C, Cambourieu D, Flamant C, Gascoin G, Gaudineau A, Grangé G, Houfflin-Debarge V, Langer B, Malan V, Marcorelles P, Nizard J, Perrotin F, Salomon L, Senat M-V, Serry A, Tessier V, Truffert P, Tsatsaris V, Arnaud C, Carbonne B (2015) Fetal growth restriction and intra-uterine growth restriction: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol 193:10–18. https://doi.org/10.1016/J.EJOGRB.2015.06.021
Sharma D, Shastri S, Sharma P (2016) Intrauterine growth restriction: antenatal and postnatal aspects. Clin Med Insights Pediatr 10:67–83. https://doi.org/10.4137/CMPed.S40070
De Boo HA, Harding JE (2006) The developmental origins of adult disease (Barker) hypothesis. Aust New Zeal J Obstet Gynaecol. https://doi.org/10.1111/j.1479-828X.2006.00506.x
Choi GY, Tosh DN, Garg A, Mansano R, Ross MG, Desai M (2007) Gender-specific programmed hepatic lipid dysregulation in intrauterine growth-restricted offspring. Am J Obstet Gynecol 196:477.e1–477.e7. https://doi.org/10.1016/j.ajog.2007.02.024
Katragadda T, Rajesh SM, Shetty S, Baliga S (2017) Comparison of cord blood lipid profile in preterm small for gestational age and appropriate for gestational age newborns. J Clin Diagn Res 11:SC05–SC07. https://doi.org/10.7860/JCDR/2017/24247.9197
Milenković S, Jankovic B, Mirković L, Jovandaric MZ, Milenković D, Otašević B (2017) Lipids and adipokines in cord blood and at 72 h in discordant dichorionic twins. Fetal Pediatr Pathol 36:106–122. https://doi.org/10.1080/15513815.2016.1242675
Ophir E, Oettinger M, Nisimov J, Hirsch Y, Fait V, Dourleshter G, Shnaider O, Snitkovsky T, Bornstein J (2004) Cord blood lipids concentrations and their relation to body size at birth: possible link between intrauterine life and adult diseases. Am J Perinatol 21:35–40
De Jong M, Cranendonk A, Van Weissenbruch MM (2015) Components of the metabolic syndrome in early childhood in very-low-birth-weight infants and term small and appropriate for gestational age infants. Pediatr Res 78:457–461. https://doi.org/10.1038/pr.2015.118
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon E-S (2005) Birth weight standards in the live-born population in Israel. Isr Med Assoc J 7:311–314 http://www.ncbi.nlm.nih.gov/pubmed/15909464 (accessed December 1, 2018)
Parry G, Tucker J, Tarnow-Mordi W (2003) CRIB II: an update of the clinical risk index for babies score. Lancet. 361:1789–1791. https://doi.org/10.1016/S0140-6736(03)13397-1
Sinclair R, Schindler T, Lui K, Bolisetty S (2018) Hypertriglyceridaemia in extremely preterm infants receiving parenteral lipid emulsions. BMC Pediatr 18:1–7. https://doi.org/10.1186/s12887-018-1325-2
Holtrop P, Swails T, Riggs T (2015) Hypertriglyceridemia in extremely low birth weight infants receiving lipid emulsions. J Neonatal-Perinatal Med 8:133–136. https://doi.org/10.3233/NPM-15814099
Brans YW, Andrew DS, Carrillo DW, Dutton EB, Menchaca EM, Puelo-Scheppke BA (1990) Tolerance of fat emulsions in very low birthweight neonates: effect of birthweight on plasma lipid concentrations. Am J Perinatol 7:114–117. https://doi.org/10.1055/s-2007-999459
Hossain MA, Islam MN, Shahidullah M, Akhter H (2006) Serum triglyceride level in IUGR babies and its comparison with preterm AGA and term normal babies. Mymensingh Med J 15:180–182 http://www.ncbi.nlm.nih.gov/pubmed/16878101
Kim S, Lee SC, Kim DS-M, Kim SJ, Kim C (2017) Cord and maternal sera from small neonates share dysfunctional lipoproteins with proatherogenic properties: evidence for Barker’s hypothesis. S J Clin Lipidol 11:1318–1328. https://doi.org/10.1016/j.jacl.2017.08.020
Kaser S, Ebenbichler CF, Wolf HJ, Sandhofer A, Stanzl U, Ritsch A, Patsch JR (2001) Lipoprotein profile and cholesteryl ester transfer protein in neonates. Metabolism. https://doi.org/10.1053/meta.2001.23307
Economides DL, Crook D, Nicolaides KH (1990) Hypertriglyceridemia and hypoxemia in small-for-gestational-age fetuses. Am J Obstet Gynecol 162:382–386. https://doi.org/10.1016/0002-9378(90)90391-J
Jones JN, Gercel-Taylor C, Taylor DD (1999) Altered cord serum lipid levels associated with small for gestational age infants. Obstet Gynecol 93:527–531. https://doi.org/10.1016/s0029-7844(98)00489-x
Sohi G, Marchand K, Revesz A, Arany E, Hardy DB (2011) Maternal protein restriction elevates cholesterol in adult rat offspring due to repressive changes in histone modifications at the Cholesterol 7 α- hydroxylase promoter. Mol Endocrinol 25:785–798. https://doi.org/10.1210/me.2010-0395
Park JH, Stoffers DA, Nicholls RD, Simmons RA (2008) Development of type 2 diabetes following intrauterine growth retardation in rats is associated with progressive epigenetic silencing of Pdx1. J Clin Invest 118:2316–2324. https://doi.org/10.1172/JCI33655
Calkins K, Devaskar SU (2011) Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care 41:158–176. https://doi.org/10.1016/j.cppeds.2011.01.001
Rinaudo P, Wang E (2012) Fetal programming and metabolic syndrome. Annu Rev Physiol 74:107–130. https://doi.org/10.1146/annurev-physiol-020911-153245
Ramasamy I (2014) Recent advances in physiological lipoprotein metabolism. Clin Chem Lab Med 52:1695–1727. https://doi.org/10.1515/cclm-2013-0358
Chyzhyk V, Brown AS (2019) Familial chylomicronemia syndrome: a rare but devastating autosomal recessive disorder characterized by refractory hypertriglyceridemia and recurrent pancreatitis. Trends Cardiovasc Med. https://doi.org/10.1016/j.tcm.2019.03.001
Zhu W-F, Zhu J-F, Liang L, Shen Z, Wang Y-M (2016) Maternal undernutrition leads to elevated hepatic triglycerides in male rat offspring due to increased expression of lipoprotein lipase. Mol Med Rep 13:4487–4493. https://doi.org/10.3892/mmr.2016.5040
Gauster M, Hiden U, Blaschitz A, Frank S, Lang U, Alvino G, Cetin I, Desoye G, Wadsack C (2007) Dysregulation of placental endothelial lipase and lipoprotein lipase in intrauterine growth-restricted pregnancies. J Clin Endocrinol Metab 92:2256–2263. https://doi.org/10.1210/jc.2006-2403
Author information
Authors and Affiliations
Contributions
S.R—study design, acquisition of data, analysis and interpretation of data, and drafting the manuscript.
O.L—study design, acquisition of data, analysis and interpretation of data, and drafting the manuscript.
L.L—clinical input and revision the manuscript.
I.SE—data analysis and revision the manuscript.
I.M—clinical input and revision of manuscript.
C.R—clinical input and revision of manuscript.
A.MM—analysis and interpretation of data, and revision of manuscript.
T.S—study conception and design, analysis and interpretation of data, and revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Editorial Responsibility: Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Rabinowicz, S., Levkovitz, O., Leibovitch, L. et al. Increased risk for early hypertriglyceridemia in small for gestational age preterm infants. Eur J Pediatr 179, 1873–1879 (2020). https://doi.org/10.1007/s00431-020-03764-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03764-8