Abstract
Leptospirosis is a life-threatening zoonotic disease and it has been hypothesized that the innate immune system fails to control the infection through ill-characterized mechanisms. The aim of this observational study was to better evaluate the activation processes of monocytes at the early stage of the disease. Blood samples were taken from healthy donors (n = 37) and patients hospitalized for either non-severe (n = 25) or severe (n = 32) leptospirosis. Monocyte cell counts and phenotypes were assessed by flow cytometry. We analysed the expression of several cell activation markers: CD14, CD16, HLA-DR, CD69, TLR2, TLR4, CD11b and CD11c. Although monocyte values at admittance were not significantly different from controls, patients experienced significant monocytosis at 1.33 × 109/L (p < 0.0001 compared to controls: 0.56 × 109/L) during their hospital stay. This monocytosis observed during hospital stay was correlated to several surrogate markers of organ injury. Non-classical (CD14−CD16+) and intermediate (CD14+CD16+) monocyte subsets increased compared to controls (p < 0.05). Accordingly, classical monocyte subset (CD14+CD16−) showed decreased percentages (p < 0.0001). Levels of several cell surface activation molecules were decreased: HLA-DR involved in MHC class II antigen presentation, integrins CD11b and CD11c implicated in phagocytosis and cell recruitment (p < 0.0001). None of these parameters had a prognostic value. Results from this study showed that during acute human leptospirosis, patients experienced monocytosis with a switch toward an inflammation-related phenotype contrasted by low expression levels of markers implicated in monocyte function.




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available in the FlowRepository public database, URL: https://flowrepository.org/id/RvFrfom7jwL1SHc4nTFg2epdGcDpHc3qwtsGSOPoDm6ofWkmfjfQTm22c2UcA1At.
References
Costa F, Hagan JE, Calcagno J et al (2015) Global morbidity and mortality of leptospirosis: a systematic review. PLoS Negl Trop Dis 9:e0003898. https://doi.org/10.1371/journal.pntd.0003898
Bharti AR, Nally JE, Ricaldi JN et al (2003) Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis 3:757–771
Hotchkiss RS, Monneret G, Payen D (2013) Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol 13:862–874. https://doi.org/10.1038/nri3552
Werts C (2017) Interaction of Leptospira with the Innate Immune System. Curr Top Microbiol Immunol. https://doi.org/10.1007/82_2017_46
Toma C, Okura N, Takayama C, Suzuki T (2011) Characteristic features of intracellular pathogenic Leptospira in infected murine macrophages. Cell Microbiol 13:1783–1792. https://doi.org/10.1111/j.1462-5822.2011.01660.x
Liu B, Wang Y, Guo X et al (2014) Carboxyfluorescein diacetate succinimidyl ester labeling method to study the interaction between Leptospira and macrophages. J Microbiol Methods 107:205–213. https://doi.org/10.1016/j.mimet.2014.10.005
Davis JM, Haake DA, Ramakrishnan L (2009) Leptospira interrogans stably infects zebrafish embryos, altering phagocyte behavior and homing to specific tissues. PLoS Negl Trop Dis 3:e463. https://doi.org/10.1371/journal.pntd.0000463
Chen X, Li S-J, Ojcius DM et al (2017) Mononuclear-macrophages but not neutrophils act as major infiltrating anti-leptospiral phagocytes during leptospirosis. PLoS One 12:e0181014. https://doi.org/10.1371/journal.pone.0181014
Li S, Ojcius DM, Liao S et al (2010) Replication or death: distinct fates of pathogenic Leptospira strain Lai within macrophages of human or mouse origin. Innate Immun 16:80–92. https://doi.org/10.1177/1753425909105580
Wang B, Sullivan JA, Sullivan GW, Mandell GL (1984) Role of specific antibody in interaction of leptospires with human monocytes and monocyte-derived macrophages. Infect Immun 46:809–813
Zhang L, Zhang C, Ojcius DM et al (2012) The mammalian cell entry (Mce) protein of pathogenic Leptospira species is responsible for RGD motif-dependent infection of cells and animals. Mol Microbiol 83:1006–1023. https://doi.org/10.1111/j.1365-2958.2012.07985.x
Xue F, Zhao X, Yang Y et al (2013) Responses of murine and human macrophages to leptospiral infection: a study using comparative array analysis. PLoS Negl Trop Dis 7:e2477. https://doi.org/10.1371/journal.pntd.0002477
Jongyota W, Wigraipat C, Nontapa S et al (2008) Differential response of cytokines induced by Leptospira interrogans, serogroup Pomona, serovar Pomona, in mouse and human cell lines. Asian Pac J Allergy Immunol 26:229–236
Goris MGA, Wagenaar JFP, Hartskeerl RA et al (2011) Potent innate immune response to pathogenic Leptospira in human whole blood. PLoS One 6:e18279. https://doi.org/10.1371/journal.pone.0018279
Nahori M-A, Fournié-Amazouz E, Que-Gewirth NS et al (2005) Differential TLR recognition of leptospiral lipid A and lipopolysaccharide in murine and human cells. J Immunol 175:6022–6031
Gomes-Solecki M, Santecchia I, Werts C (2017) Animal models of Leptospirosis: of mice and hamsters. Front Immunol 8:58. https://doi.org/10.3389/fimmu.2017.00058
Raffray L, Giry C, Vandroux D et al (2016) Major neutrophilia observed in acute phase of human leptospirosis is not associated with increased expression of granulocyte cell activation markers. PLoS One 11:e0165716. https://doi.org/10.1371/journal.pone.0165716
Raffray L, Giry C, Thirapathi Y et al (2017) Increased levels of soluble forms of E-selectin and ICAM-1 adhesion molecules during human leptospirosis. PLoS One 12:e0180474. https://doi.org/10.1371/journal.pone.0180474
Bellomo R, Ronco C, Kellum JA et al (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the acute dialysis quality initiative (ADQI) Group. Crit Care 8:R204–212. https://doi.org/10.1186/cc2872
Bone RC, Balk RA, Cerra FB et al (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. Am Coll Chest Phys Soc Critical Care Med Chest 101:1644–1655
Giry C, Roquebert B, Li-Pat-Yuen G et al (2017) Simultaneous detection of chikungunya virus, dengue virus and human pathogenic Leptospira genomes using a multiplex TaqMan® assay. BMC Microbiol 17:105. https://doi.org/10.1186/s12866-017-1019-1
Levett PN, Morey RE, Galloway RL et al (2005) Detection of pathogenic leptospires by real-time quantitative PCR. J Med Microbiol 54:45–49
Ziegler-Heitbrock L, Ancuta P, Crowe S et al (2010) Nomenclature of monocytes and dendritic cells in blood. Blood 116:e74–e80. https://doi.org/10.1182/blood-2010-02-258558
Pagès F, Polycarpe D, Dehecq J-S et al (2014) Human leptospirosis on Reunion Island: past and current burden. Int J Environ Res Public Health 11:968–982. https://doi.org/10.3390/ijerph110100968
Delmas B, Jabot J, Chanareille P et al (2017) Leptospirosis in ICU: a retrospective study of 134 consecutive admissions. Crit Care Med. https://doi.org/10.1097/CCM.0000000000002825
Guernier V, Lagadec E, Cordonin C et al (2016) Human Leptospirosis on Reunion Island, Indian Ocean: are rodents the (only) ones to blame? PLoS Negl Trop Dis 10:e0004733. https://doi.org/10.1371/journal.pntd.0004733
De Silva NL, Niloofa M, Fernando N et al (2014) Changes in full blood count parameters in leptospirosis: a prospective study. Int Arch Med 7:31. https://doi.org/10.1186/1755-7682-7-31
Craig SB, Graham GC, Burns M-A et al (2009) Haematological and clinical-chemistry markers in patients presenting with leptospirosis: a comparison of the findings from uncomplicated cases with those seen in the severe disease. Ann Trop Med Parasitol 103:333–341. https://doi.org/10.1179/136485909X435058
Wong KL, Yeap WH, Tai JJY et al (2012) The three human monocyte subsets: implications for health and disease. Immunol Res 53:41–57. https://doi.org/10.1007/s12026-012-8297-3
Fingerle G, Pforte A, Passlick B et al (1993) The novel subset of CD14+/CD16+ blood monocytes is expanded in sepsis patients. Blood 82:3170–3176
Skrzeczyñska J, Kobylarz K, Hartwich Z et al (2002) CD14+ CD16+ monocytes in the course of sepsis in neonates and small children: monitoring and functional studies. Scand J Immunol 55:629–638
Mukherjee R, Kanti Barman P, Kumar Thatoi P et al (2015) Non-classical monocytes display inflammatory features: validation in sepsis and systemic lupus erythematous. Sci Rep 5:13886. https://doi.org/10.1038/srep13886
Poehlmann H, Schefold JC, Zuckermann-Becker H et al (2009) Phenotype changes and impaired function of dendritic cell subsets in patients with sepsis: a prospective observational analysis. Crit Care 13:R119. https://doi.org/10.1186/cc7969
Monneret G, Finck M-E, Venet F et al (2004) The anti-inflammatory response dominates after septic shock: association of low monocyte HLA-DR expression and high interleukin-10 concentration. Immunol Lett 95:193–198. https://doi.org/10.1016/j.imlet.2004.07.009
Landelle C, Lepape A, Voirin N et al (2010) Low monocyte human leukocyte antigen-DR is independently associated with nosocomial infections after septic shock. Intensive Care Med 36:1859–1866. https://doi.org/10.1007/s00134-010-1962-x
Monneret G, Lepape A, Voirin N et al (2006) Persisting low monocyte human leukocyte antigen-DR expression predicts mortality in septic shock. Intensive Care Med 32:1175–1183. https://doi.org/10.1007/s00134-006-0204-8
Diament D, Brunialti MKC, Romero EC et al (2002) Peripheral blood mononuclear cell activation induced by Leptospira interrogans glycolipoprotein. Infect Immun 70:1677–1683
Salomao R, Brunialti MKC, Rapozo MM et al (2012) Bacterial sensing, cell signaling, and modulation of the immune response during sepsis. Shock 38:227–242. https://doi.org/10.1097/SHK.0b013e318262c4b0
Brunialti MKC, Martins PS, Barbosa de Carvalho H et al (2006) TLR2, TLR4, CD14, CD11B, and CD11C expressions on monocytes surface and cytokine production in patients with sepsis, severe sepsis, and septic shock. Shock 25:351–357. https://doi.org/10.1097/01.shk.0000217815.57727.29
Cinco M, Vecile E, Murgia R et al (1996) Leptospira interrogans and Leptospira peptidoglycans induce the release of tumor necrosis factor alpha from human monocytes. FEMS Microbiol Lett 138:211–214
Russwurm S, Vickers J, Meier-Hellmann A et al (2002) Platelet and leukocyte activation correlate with the severity of septic organ dysfunction. Shock 17:263–268
Jämsä J, Huotari V, Savolainen E-R et al (2015) Kinetics of leukocyte CD11b and CD64 expression in severe sepsis and non-infectious critical care patients. Acta Anaesthesiol Scand 59:881–891. https://doi.org/10.1111/aas.12515
Vieira ML, Naudin C, Mörgelin M et al (2016) Modulation of hemostatic and inflammatory responses by Leptospira Spp. PLoS Negl Trop Dis 10:e0004713. https://doi.org/10.1371/journal.pntd.0004713
Dorigatti F, Brunialti MKC, Romero EC et al (2005) Leptospira interrogans activation of peripheral blood monocyte glycolipoprotein demonstrated in whole blood by the release of IL-6. Braz J Med Biol Res 38:909–914
Acknowledgements
The authors thank the practitioners implicated in the patients’ care as well as the members of the microbiology laboratory of St Denis, La Réunion, for their help in patients’ recruitment. We also thank Alexander Greenshields for critical appraisal of the manuscript.
Funding
The authors work is funded by the research unit PIMIT (processus infectieux en milieu insulaire tropical) and the CHU (centre hospitalo-universaire) de la Réunion. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interest to declare.
Ethical approval
This study was approved by the local human ethic committee of tertiary teaching Hospital ‘CHU de La Réunion’ (protocol number R15018) and conducted according to the principles expressed in the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Additional information
Edited by: C.Bogdan.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1: Evolution of monocyte cell counts during hospitalization and convalescent phase for 10 leptospirosis patients. Caption
: Paired values of monocytes for leptospirosis cases during hospitalization (admittance and maximal value) and 1 month after discharge (M1). Comparisons with non-parametric Wilcoxon paired test. ** indicates P value inferior to 0.01, respectively. (TIFF 315 KB)
Supplementary Fig. 2: Higher
bacteraemia in severe leptospirosis cases. Caption: Plasmatic Leptospira load is established from the 50 patients with positive RT-qPCR in blood and using the log-transformed standard curve. Horizontal bars indicate the median and IQR ranges. Comparison with non-parametric Mann-Whitney test. ** indicates P value inferior to 0.01. (TIFF 289 KB)
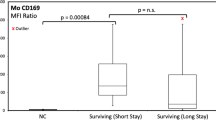
Supplementary Fig. 3: Higher levels of cell surface expression of CD69 on monocytes in severe cases of leptospirosis Caption
: comparison of selected cell surface markers among healthy donors and leptospirosis patients according to disease severity. Horizontal bars indicate the median and IQR ranges for mean fluorescence intensity (MFI). Comparison with non-parametric Mann-Whitney test. **, **** indicate P values inferior to 0.01 and 0.0001, respectively. (TIFF 667 KB)
Rights and permissions
About this article
Cite this article
Raffray, L., Giry, C., Vandroux, D. et al. The monocytosis during human leptospirosis is associated with modest immune cell activation states. Med Microbiol Immunol 208, 667–678 (2019). https://doi.org/10.1007/s00430-018-0575-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-018-0575-9