Abstract
Aim
Exercise training with blood flow restriction (BFR) increases muscle size and strength. However, there is limited investigation into the effects of BFR on cardiovascular health, particularly central hemodynamic load.
Purpose
To determine the effects of BFR exercise on central hemodynamic load (heart rate—HR, central pressures, arterial wave reflection, and aortic stiffness).
Methods
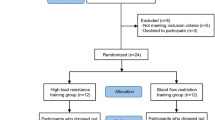
Fifteen males (age = 25 ± 2 years; BMI = 27 ± 2 kg/m2, handgrip max voluntary contraction-MVC = 50 ± 2 kg) underwent 5-min bouts (counter-balanced, 10 min rest between) of rhythmic unilateral handgrip (1 s squeeze, 2 s relax) performed with a moderate-load (60% MVC) with and without BFR (i.e., 71 ± 5% arterial inflow flow reduction, assessed via Doppler ultrasound), and also with a low-load (40% MVC) with BFR. Outcomes included HR, central mean arterial pressure (cMAP), arterial wave reflection (augmentation index, AIx; wave reflection magnitude, RM%), aortic arterial stiffness (pulse wave velocity, aPWV), and peripheral (vastus lateralis) microcirculatory response (tissue saturation index, TSI%).
Results
HR increased above baseline and time control for all handgrip bouts, but was similar between the moderate load with and without BFR conditions (moderate-load with BFR = + 9 ± 2; moderate-load without BFR = + 8 ± 2 bpm, p < 0.001). A similar finding was noted for central pressure (e.g., moderate load with BFR, cMAP = + 14 ± 1 mmHg, p < 0.001). No change occurred for RM% or AIx (p > 0.05) for any testing stage. TSI% increased during the moderate-load conditions (p = 0.01), and aPWV increased above baseline following moderate-load handgrip with BFR only (p = 0.012).
Conclusions
Combined with BFR, moderate load handgrip training with BFR does not significantly augment central hemodynamic load during handgrip exercise in young healthy men.





Similar content being viewed by others
Abbreviations
- Aix:
-
Augmentation Index
- AP:
-
Augmentation pressure
- aPWV:
-
Aortic pulse wave velocity
- BFR:
-
Blood flow restriction exercise
- BP:
-
Blood pressure
- cMAP:
-
Central mean arterial pressure
- H+ :
-
Hydrogen ions
- HF:
-
High-frequency component
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- L1:
-
Distance between sternal notch and carotid pulse site
- L2:
-
Distance between sternal notch and proximal edge of thigh cuff
- LF:
-
Low-frequency component
- LF/HF:
-
Low-frequency-to-high-frequency component ratio
- MHz:
-
Mega-hertz
- MVC:
-
Maximal voluntary contraction
- NIRS:
-
Near-infrared spectroscopy
- Pb:
-
Backward pressure component
- Pf:
-
Forward pressure component
- PP:
-
Pulse pressure
- RM%:
-
Reflection magnitude
- RMSSD:
-
Root mean square of standard deviation of R–R intervals
- RPP:
-
Rate pressure product
- SDNN:
-
Standard deviation of R–R intervals
- TSI%:
-
Tissue Saturation Index
- V mean :
-
Mean blood velocity
References
Abe T, Kearns CF, Sato Y (2006) Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. J Appl Physiol 100:1460–1466
Alam M, Smirk FH (1937) Observations in man upon a blood pressure raising reflex arising from the voluntary muscles. J Physiol 89:372–383
Barstow TJ (2019) Understanding near infrared spectroscopy (NIRS) and its application to skeletal muscle research. J Appl Physiol 126:1360–1376
Butlin M, Qasem A, Avolio AP (2012) Estimation of central aortic pressure waveform features derived from the brachial cuff volume displacement waveform. Conf Proc IEEE Eng Med Biol Soc 2012:2591–2594
Camm AJ et al (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93:1043–1065
Credeur DP, Hollis BC, Welsch MA (2010) Effects of handgrip training with venous restriction on brachial artery vasodilation. Med Sci Sports Exer 42:1296–1302
Credeur DP et al (2014) Characterizing rapid onset vasodilation to single muscle contractions in the human leg. J Appl Physiol 118:455–464
Dankel SJ, Jessee MB, Abe T, Loenneke JP (2016) The effects of blood flow restriction on upper-body musculature located distal and proximal to applied pressure. Sports Med 46:23–33
Delaney EP, Greaney JL, Edwards DG, Rose WC, Fadel PJ, Farquhar WB (2010) Exaggerated sympathetic and pressor responses to handgrip exercise in older hypertensive humans: role of the muscle metaboreflex. Am J Physiol Heart Circ Physiol 299:H1318–1327
Domingos E, Polito MD (2018) Blood pressure response between resistance exercise with and without blood flow restriction: A systematic review and meta-analysis. Life Sci 209:122–131
Dursteine JL, Moore GM (2003) ACSM's exercise management for persons with chronic diseases and disabilities, 2nd edn. Human kinetics
Fadel PJ, Keller DM, Watanabe H, Raven PB, Thomas GD (2004) Noninvasive assessment of sympathetic vasoconstriction in human and rodent skeletal muscle using near-infrared spectroscopy and Doppler ultrasound. J Appl Physiol 96:1323–1330
Gebber GL, Zhong S, Lewis C, Barman SM (2000) Defenselike patterns of spinal sympathetic outflow involving the 10-Hz and cardiac-related rhythms. Am J Physiol Regul Integr Comp Physiol 278:R1616–1626
Gorgey AS, Timmons MK, Dolbow DR, Bengel J, Fugate-Laus KC, Michener LA, Gater DR (2016) Electrical stimulation and blood flow restriction increase wrist extensor cross-sectional area and flow meditated dilatation following spinal cord injury. Eur J Appl Physiol 116:1231–1244
Holwerda SW, Restaino RM, Manrique C, Lastra G, Fisher JP, Fadel PJ (2016) Augmented pressor and sympathetic responses to skeletal muscle metaboreflex activation in type 2 diabetes patients. Am J Physiol Heart Circ Physiol 310:H300–309
Horiuchi M, Fadel PJ, Ogoh S (2014) Differential effect of sympathetic activation on tissue oxygenation in gastrocnemius and soleus muscles during exercise in humans. Exp Physiol 99:348–358
Hunt JE, Walton LA, Ferguson RA (2012) Brachial artery modifications to blood flow-restricted handgrip training and detraining. J Appl Physiol 112:956–961
Kaur J et al (2015) Muscle metaboreflex activation during dynamic exercise vasoconstricts ischemic active skeletal muscle. Am J Physiol Heart Circ Physiol 309:H2145–2151
American College of Sports Medicine (2018) ACSM's guidelines for exercise testing and prescription, 10th edn. Wolters Kluwer, Alphen aan den Rijn
Loenneke JP, Wilson GJ, Wilson JM (2010) A mechanistic approach to blood flow occlusion. Int J Sports Med 31:1–4
Lucero AA et al (2018) Reliability of muscle blood flow and oxygen consumption response from exercise using near-infrared spectroscopy. Exp Physiol 103:90–100
Morrison SF (2001) Differential control of sympathetic outflow. Am J Physiol Regul Integr Comp Physiol 281:R683–698
Morrison SF (2001) Differential regulation of brown adipose and splanchnic sympathetic outflows in rat: roles of raphe and rostral ventrolateral medulla neurons. Clin Exp Pharmacol Physiol 28:138–143
Morrison SF (2001) Differential regulation of sympathetic outflows to vasoconstrictor and thermoregulatory effectors. Ann N Y Acad Sci 940:286–298
Mouser JG, Dankel SJ, Jessee MB, Mattocks KT, Buckner SL, Counts BR, Loenneke JP (2017) A tale of three cuffs: the hemodynamics of blood flow restriction. Eur J Appl Physiol 117:1493–1499
Qasem A, Avolio A (2008) Determination of aortic pulse wave velocity from waveform decomposition of the central aortic pressure pulse. Hypertension 51:188–195
Smith SA, Mitchell JH, Garry MG (2006) The mammalian exercise pressor reflex in health and disease. Exp Physiol 91:89–102
Smith SA, Leal AK, Young CN, Fadel PJ (2010) Neural mechanisms of cardiovascular control during exercise in health and disease. Recent advances in cardiovascular research: from sleep to exercise. Transworld research network, pp 179–209. http://www.ressign.com/UserBookDetail.aspx?bkid=1029&catid=236#
Spranger MD, Krishnan AC, Levy PD, O'Leary DS, Smith SA (2015) Blood flow restriction training and the exercise pressor reflex: a call for concern. Am J Physiol Heart Circ Physiol 309:H1440–1452
Sprick JD, Rickards CA (2017) Combining remote ischemic preconditioning and aerobic exercise: a novel adaptation of blood flow restriction exercise. Am J Physiol Regul Integr Comp Physiol 313:R497–R506
Sugaya M, Yasuda T, Suga T, Okita K, Abe T (2011) Change in intramuscular inorganic phosphate during multiple sets of blood flow-restricted low-intensity exercise. Clin Physiol Funct Imaging 31:411–413
Thavasothy M, Broadhead M, Elwell C, Peters M, Smith M (2002) A comparison of cerebral oxygenation as measured by the NIRO 300 and the INVOS 5100 Near-Infrared Spectrophotometers. Anaesthesia 57:999–1006
Acknowledgements
The authors would like to thank the participants for their time and dedication towards the study. The authors would also like to thank the students (graduate and undergraduate) from the School of Kinesiology and Nutrition at the University of Southern Mississippi for their support and assistance throughout the various stages of this project.
Author information
Authors and Affiliations
Contributions
DC, LS, and SM conceived, and designed research; DC, RJ, and SM conducted experiments; DC, RJ, DS, LS, and MJ analyzed data; DC and RJ drafted the manuscript. All authors read, edited, and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to report for this study.
Additional information
Communicated by Philip D Chilibeck.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Credeur, D.P., Jones, R., Stanford, D. et al. Central cardiovascular hemodynamic response to unilateral handgrip exercise with blood flow restriction. Eur J Appl Physiol 119, 2255–2263 (2019). https://doi.org/10.1007/s00421-019-04209-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-019-04209-3