Abstract
Purpose
This study aims to analyze the retinal layers and choroidal thickness in a large set of eyes with early age-related macular degeneration (AMD), in order to detect differences by stage suggestive of early neurodegeneration, and to explore biomarkers of different phenotypes.
Methods
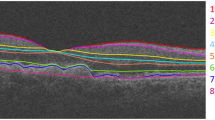
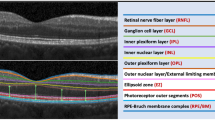
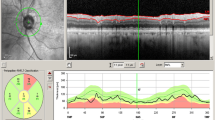
This study is a population-based, cross-sectional study. Patients from the incidence AMD study (NCT02748824) with early AMD (Rotterdam 2a, 2b, 3) were included. All performed spectral-domain optical coherence tomography (SD-OCT) (Spectralis, Heidelberg Engineering, Germany) and automatic segmentation of all retinal layers was obtained with built-in software. Manual correction was performed whenever necessary. The mean thicknesses (ETDRS grid) and volume of each layer were recorded. Subfoveal choroidal thickness was manually measured. Estimates for each layer thickness were calculated with linear mixed models and tested for pairwise differences between stages. Associations between layer thickness and microstructural findings were assessed by multivariate regression analysis.
Results
The final cohort comprised 346 eyes (233 patients): 82.66% (n = 286) in stage 2a, 5.49% (n = 19) in stage 2b, and 11.85% (n = 41) in stage 3. A global tendency for lower/inferior thickness of the neuroretinal layers was found comparing stage 3 to 2a: retinal nerve fiber layer (RNFL), ganglion cell layer (GCL), and inner plexiform layer (IPL) were inferior in the inner/outer ETDRS circles and the outer nuclear layer (ONL) and photoreceptors’ segments layer in the central circle (p ≤ 0.002). The retinal pigment epithelium–Bruch’s membrane (RPE/BrM) layer was thicker in stage 3 (p ≤ 0.001). Subretinal drusenoid deposits (SDD) were associated with thinner neuroretinal layers and choroid (p < 0.05).
Conclusions
Our results showed in a large population-based dataset that several inner and outer neuroretinal layers were thinner with a higher stage in early AMD. These findings support the existence of early and progressive neurodegeneration. Neuronal retinal layer thicknesses might thus be used as quantitative biomarkers of disease progression in AMD. The presence of SDD is possibly associated to more prominent and faster neurodegeneration.





Similar content being viewed by others
References
Coljn JM, Buitendijk GHS, Prokofyeva E et al (2017) Prevalence of age-related macular degeneration in Europe: the past and the future. Ophthalmology 124:1753–1763
Li JQ, Welchowski T, Schmid M, Mauschitz MM, Holz FG, Finger RP (2019) Prevalence and incidence of age-related macular degeneration in Europe: a systematic review and meta-analysis. Br J Ophthalmol 104(8):1077–1084
Wong WL, Su X, Li X, Cheung CMG, Klein R, Cheng CY, Wong TY (2014) Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2(2):e106–e116
Sitnilska V, Kersten E, Altay L, Schick T, Enders P, de Jong EK, Langmann T, Hoyng CB, den Hollander AI, Fauser S (2020) Major predictive factors for progression of early to late age-related macular degeneration. Ophthalmologica 243(6):444–452
Finger RP, Schmitz-Valckenberg S, Schmid M, Rubin GS, Dunbar H, Tufail A, Crabb DP, Binns A, Sánchez CI, Margaron P, Normand G, Durbin MK, Luhmann UFO, Zamiri P, Cunha-Vaz J, Asmus F, Holz FG, on behalf of the MACUSTAR consortium (2019) MACUSTAR: development and clinical validation of functional, structural, and patient-reported endpoints in intermediate age-related macular degeneration. Ophthalmologica 241(2):61–72
Heesterbeek TJ, Lorés-Motta L, Hoyng CB, Lechanteur YTE, den Hollander AI (2020) Risk factors for progression of age-related macular degeneration. Ophthalmic Physiol Opt 40:140–170
Kersten E, Paun CC, Schellevis RL, Hoyng CB, Delcourt C, Lengyel I, Peto T, Ueffing M, Klaver CCW, Dammeier S, den Hollander AI, de Jong EK (2018) Systemic and ocular fluid compounds as potential biomarkers in age-related macular degeneration. Surv Ophthalmol 63:9–39
Strunz T, Lauwen S, Kiel C et al (2020) A transcriptome-wide association study based on 27 tissues identifies 106 genes potentially relevant for disease pathology in age-related macular degeneration. Sci Rep 10:1–16
Holz FG, Sadda SVR, Staurenghi G et al (2017) Imaging protocols in clinical studies in advanced age-related macular degeneration: recommendations from classification of atrophy consensus meetings. Ophthalmology 124:464–478
Sadda SR, Guymer R, Holz FG et al (2018) Consensus definition for atrophy associated with age-related macular degeneration on OCT. Classification of Atrophy Report 3. Ophthalmology 125:537–548
Guymer RH, Rosenfeld PJ, Curcio CA et al (2020) Incomplete retinal pigment epithelial and outer retinal atrophy in age-related macular degeneration: classification of atrophy meeting report 4. Ophthalmology 127:394–409
Farinha C, Cachulo ML, Coimbra R, Alves D, Nunes S, Pires I, Marques JP, Costa J, Martins A, Sobral I, Barreto P, Laíns I, Figueira J, Ribeiro L, Cunha-Vaz J, Silva R (2020) Age-related macular degeneration staging by color fundus photography vs. multimodal imaging—epidemiological implications (The Coimbra Eye Study—Report 6). J Clin Med 9:1329
Nittala MG, Hogg RE, Luo Y, Velaga SB, Silva R, Alves D, Staurenghi G, Chakravarthy U, Sadda SR (2018) Changes in retinal layer thickness in the contralateral eye of patients with unilateral neovascular age-related macular degeneration. Ophthalmol Retin 3:112–121
Brandl C, Brücklmayer C, Günther F, Zimmermann ME, Küchenhoff H, Helbig H, Weber BHF, Heid IM, Stark KJ (2019) Retinal layer thicknesses in early age-related macular degeneration: results from the German AugUR study. Invest Ophthalmol Vis Sci 60:1581–1594
Abdelfattah NS, Zhang H, Boyer DS, Rosenfeld PJ, Feuer WJ, Gregori G, Sadda SR (2016) Drusen volume as a predictor of disease progression in patients with late age-related macular degeneration in the fellow eye. Investig Ophthalmol Vis Sci 57:1839–1846
Lee MW, Kim JM, Lim HB, Shin YI, Lee YH, Kim JY (2020) Longitudinal changes in ganglion cell–inner plexiform layer of fellow eyes in unilateral neovascular age-related macular degeneration. Am J Ophthalmol 212:17–25
Lamin A, Oakley JD, Dubis AM, Russakoff DB, Sivaprasad S (2019) Changes in volume of various retinal layers over time in early and intermediate age-related macular degeneration. Eye 33:428–434
Lee EK, Yu HG (2015) Ganglion cell–inner plexiform layer and peripapillary retinal nerve fiber layer thicknesses in age-related macular degeneration. Investig Ophthalmol Vis Sci 56:3976–3983
Muftuoglu IK, Ramkumar HL, Bartsch DU, Meshi A, Gaber R, Freeman WR (2017) Quantitative analysis of the inner retinal layer thicknesses in age related macular degeneration using corrected optical coherence tomography segmentation. Retina 38:1478–1484
Yenice E, Şengün A, Soyugelen Demirok G, Turaçli E (2015) Ganglion cell complex thickness in nonexudative age-related macular degeneration. Eye 29:1076–1080
Savastano MC, Minnella AM, Tamburrino A, Giovinco G, Ventre S, Falsini B (2014) Differential vulnerability of retinal layers to early age-related macular degeneration: Evidence by SD-OCT segmentation analysis. Investig Ophthalmol Vis Sci 55:560–566
Cachulo MDL, Lobo C, Figueira J, Ribeiro L, Laíns I, Vieira A, Nunes S, Costa M, Simão S, Rodrigues V, Vilhena N, Cunha-Vaz J, Silva R (2015) Prevalence of age-related macular degeneration in Portugal: the Coimbra eye study - Report 1. Ophthalmologica 233:119–127
Cachulo M d L, Laíns I, Lobo C, Figueira J, Ribeiro L, Marques JP, Costa J, Vieira A, Rodrigues J, Alves D, Nunes S, Costa M, Rodrigues V, Cunha-Vaz J, Delcourt C, Silva R, Age-related macular degeneration in Portugal (2016) prevalence and risk factors in a coastal and an inland town. The Coimbra Eye Study – Report 2. Acta Ophthalmol 94:e442–e453
Farinha CVL, Cachulo ML, Alves D, Pires I, Marques JP, Barreto P, Nunes S, Costa J, Martins A, Sobral I, Laíns I, Figueira J, Ribeiro L, Cunha-Vaz J, Silva R (2019) Incidence of age-related macular degeneration in the central region of Portugal: the coimbra eye study-report 5. Ophthalmic Res 61(4):226–235
Klaver CC, Assink JJ, van Leeuwen R, Wolfs RC, Vingerling JR, Stijnen T, Hofman A, de Jong PT (2001) Incidence and progression rates of age-related maculopathy: the Rotterdam Study. Invest Ophthalmol Vis Sci 42(10):2237–2241
Gattoussi S, Buitendijk GHS, Peto T et al (2019) The European eye epidemiology spectral-domain optical coherence tomography classification of macular diseases for epidemiological studies. Acta Ophthalmol 97:364–371
Nassisi M, Fan W, Shi Y, Lei J, Borrelli E, Ip M, Sadda SR (2018) Quantity of intraretinal hyperreflective foci in patients with intermediate age-related macular degeneration correlates with 1-year progression. Investig Ophthalmol Vis Sci 59:3431–3439
Won JY, Kim SE, Park YH (2016) Effect of age and sex on retinal layer thickness and volume in normal eyes. Medicine (United States) 95:1–6
Margolis R, Spaide RF (2009) A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol 147:811–815
Borrelli E, Abdelfattah NS, Uji A, Nittala MG, Boyer DS, Sadda SVR (2017) Postreceptor neuronal loss in intermediate age-related macular degeneration. Am J Ophthalmol 181:1–11
Garg A, Oll M, Yzer S, Chang S, Barile GR, Merriam JC, Tsang SH, Bearelly S (2013) Reticular pseudodrusen in early age-related macular degeneration are associated with choroidal thinning. Invest Ophthalmol Vis Sci 54:7075–7081
Echols BS, Clark ME, Swain TA, Chen L, Kar D, Zhang Y, Sloan KR, McGwin G, Singireddy R, Mays C, Kilpatrick D, Crosson JN, Owsley C, Curcio CA (2020) Hyperreflective foci and specks are associated with delayed rod-mediated dark adaptation in nonneovascular age-related macular degeneration. Ophthalmol Retin 4(11):1059–1068
Acknowledgements
The authors thank Patricia Barreto and Maria Helena Madeira for their contribution in the development of the Coimbra Eye Study and in the epidemiological characterization of AMD in Portugal.
Funding
This study was an investigator-initiated study financially supported by Novartis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All human-related procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all included participants
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Table 1
(DOCX 14 kb)
Supplementary Table 2
(DOCX 18 kb)
Supplementary Table 3
(DOCX 14 kb)
Supplementary Table 4
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Farinha, C., Silva, A.L., Coimbra, R. et al. Retinal layer thicknesses and neurodegeneration in early age-related macular degeneration: insights from the Coimbra Eye Study. Graefes Arch Clin Exp Ophthalmol 259, 2545–2557 (2021). https://doi.org/10.1007/s00417-021-05140-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05140-0