Abstract
Purpose
Our aim is to develop a new generation of suprachoroidal–transretinal stimulation (STS) retinal prosthesis using a dual-stimulating electrode array to enlarge the visual field. In the present study, we aimed to examine how position and size of the visual field—created by a retinal prosthesis simulator—influenced mobility.
Methods
Twelve healthy subjects wore retinal prosthesis simulators. Images captured by a web camera attached to a head-mounted display (HMD) were processed by a computer and displayed on the HMD. Three types of artificial visual fields—designed to imitate phosphenes—obtained by a single (5 × 5 electrodes; visual angle, 15°) or dual (5 × 5 electrodes ×2; visual angle, 30°) electrode array were created. Visual field (VF)1 is an inferior visual field, which corresponds to a dual-electrode array implanted in the superior hemisphere. VF2 is a superior visual field, which corresponds to a single-electrode array implanted in the inferior hemisphere. VF3 is a superior visual field, which corresponds to a dual-electrode array implanted in the inferior hemisphere. In each type of artificial visual field, a natural circular visual field (visual angle, 5°) which imitated the vision of patients with advanced retinitis pigmentosa existed at the center. Subjects were instructed to walk along a black carpet (6 m long × 2.2 m wide) without stepping on attached white circular obstacles. Each obstacle was 20 cm in diameter, and obstacles were installed at 40-cm intervals. We measured the number of footsteps on the obstacles, the time taken to complete the obstacle course, and the extent of head movement to scan the area (head-scanning). We then compared the results recorded from these 3 types of artificial visual field.
Results
The number of footsteps on obstacles was lowest in VF3 (One-way ANOVA; P = 0.028, Fisher’s LSD; VF 1 versus 3 P = 0.039, 2 versus 3 P = 0.012). No significant difference was observed for the time to complete the obstacle course or the extent of head movement between the 3 visual fields.
Conclusion
The superior and wide visual field (VF3) obtained by the retinal prosthesis simulator resulted in better mobility performance than the other visual fields.



Similar content being viewed by others
References
Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H, Kitazawa Y, Tajimi Study G (2006) Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology 113:1354–1362. https://doi.org/10.1016/j.ophtha.2006.04.022
Kocur I, Resnikoff S (2002) Visual impairment and blindness in Europe and their prevention. Br J Ophthalmol 86:716–722
Humayun MS, Weiland JD, Fujii GY, Greenberg R, Williamson R, Little J, Mech B, Cimmarusti V, Van Boemel G, Dagnelie G, de Juan E (2003) Visual perception in a blind subject with a chronic microelectronic retinal prosthesis. Vis Res 43:2573–2581
Rizzo JF 3rd, Wyatt J, Loewenstein J, Kelly S, Shire D (2003) Perceptual efficacy of electrical stimulation of human retina with a microelectrode array during short-term surgical trials. Invest Ophthalmol Vis Sci 44:5362–5369
Zrenner E (2002) Will retinal implants restore vision? Science 295:1022–1025. https://doi.org/10.1126/science.1067996
Chow AY, Chow VY, Packo KH, Pollack JS, Peyman GA, Schuchard R (2004) The artificial silicon retina microchip for the treatment of vision loss from retinitis pigmentosa. Arch Ophthalmol 122:460–469. https://doi.org/10.1001/archopht.122.4.460
Lorach H, Goetz G, Mandel Y, Lei X, Galambos L, Kamins TI, Mathieson K, Huie P, Dalal R, Harris JS, Palanker D (2015) Performance of photovoltaic arrays in-vivo and characteristics of prosthetic vision in animals with retinal degeneration. Vis Res 111:142–148. https://doi.org/10.1016/j.visres.2014.09.007
Wong YT, Chen SC, Seo JM, Morley JW, Lovell NH, Suaning GJ (2009) Focal activation of the feline retina via a suprachoroidal electrode array. Vis Res 49:825–833. https://doi.org/10.1016/j.visres.2009.02.018
Shivdasani MN, Luu CD, Cicione R, Fallon JB, Allen PJ, Leuenberger J, Suaning GJ, Lovell NH, Shepherd RK, Williams CE (2010) Evaluation of stimulus parameters and electrode geometry for an effective suprachoroidal retinal prosthesis. J Neural Eng 7:036008. https://doi.org/10.1088/1741-2560/7/3/036008
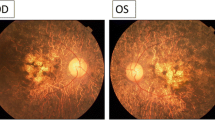
Fujikado T, Kamei M, Sakaguchi H, Kanda H, Endo T, Hirota M, Morimoto T, Nishida K, Kishima H, Terasawa Y, Oosawa K, Ozawa M, Nishida K (2016) One-year outcome of 49-channel suprachoroidal-transretinal stimulation prosthesis in patients with advanced retinitis pigmentosa. Invest Ophthalmol Vis Sci 57:6147–6157. https://doi.org/10.1167/iovs.16-20367
Stingl K, Schippert R, Bartz-Schmidt KU, Besch D, Cottriall CL, Edwards TL, Gekeler F, Greppmaier U, Kiel K, Koitschev A, Kühlewein L, MacLaren RE, Ramsden JD, Roider J, Rothermel A, Sachs H, Schröder GS, Tode J, Troelenberg N, Zrenner E (2017) Interim results of a multicenter trial with the new electronic subretinal implant alpha AMS in 15 patients blind from inherited retinal degenerations. Front Neurosci 11:445–445. https://doi.org/10.3389/fnins.2017.00445
Marigold DS, Patla AE (2008) Visual information from the lower visual field is important for walking across multi-surface terrain. Exp Brain Res 188:23–31. https://doi.org/10.1007/s00221-008-1335-7
Black AA, Wood JM, Lovie-Kitchin JE (2011) Inferior visual field reductions are associated with poorer functional status among older adults with glaucoma. Ophthalmic Physiol Opt 31:283–291. https://doi.org/10.1111/j.1475-1313.2010.00811.x
Abe RY, Diniz-Filho A, Costa VP, Gracitelli CP, Baig S, Medeiros FA (2016) The impact of location of progressive visual field loss on longitudinal changes in quality of life of patients with glaucoma. Ophthalmology 123:552–557. https://doi.org/10.1016/j.ophtha.2015.10.046
de Haan GA, Melis-Dankers BJ, Brouwer WH, Tucha O, Heutink J (2015) The effects of compensatory scanning training on mobility in patients with homonymous visual field defects: a randomized controlled trial. PLoS One 10:e0134459. https://doi.org/10.1371/journal.pone.0134459
de Haan GA, Melis-Dankers BJ, Brouwer WH, Tucha O, Heutink J (2016) The effects of compensatory scanning training on mobility in patients with homonymous visual field defects: further support, predictive variables and follow-up. PLoS One 11:e0166310. https://doi.org/10.1371/journal.pone.0166310
Sabbah N, Authie CN, Sanda N, Mohand-Said S, Sahel JA, Safran AB (2014) Importance of eye position on spatial localization in blind subjects wearing an Argus II retinal prosthesis. Invest Ophthalmol Vis Sci 55:8259–8266. https://doi.org/10.1167/iovs.14-15392
Caspi A, Roy A, Wuyyuru V, Rosendall PE, Harper JW, Katyal KD, Barry MP, Dagnelie G, Greenberg RJ (2018) Eye movement control in the Argus II retinal-prosthesis enables reduced head movement and better localization precision. Invest Ophthalmol Vis Sci 59:792–802. https://doi.org/10.1167/iovs.17-22377
Titchener SA, Shivdasani MN, Fallon JB, Petoe MA (2018) Gaze compensation as a technique for improving hand-eye coordination in prosthetic vision. Transl Vis Sci Technol 7:2. https://doi.org/10.1167/tvst.7.1.2
Glen FC, Smith ND, Crabb DP (2015) Impact of superior and inferior visual field loss on hazard detection in a computer-based driving test. Br J Ophthalmol 99:613–617. https://doi.org/10.1136/bjophthalmol-2014-305932
Dive S, Rouland JF, Lenoble Q, Szaffarczyk S, McKendrick AM, Boucart M (2016) Impact of peripheral field loss on the execution of natural actions: a study with glaucomatous patients and normally sighted people. J Glaucoma 25:e889–e896. https://doi.org/10.1097/IJG.0000000000000402
Funding
This study was supported by KAKENHI (Grants-in-Aid for Scientific Research B 16H05487).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of Osaka University Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Endo, T., Hozumi, K., Hirota, M. et al. The influence of visual field position induced by a retinal prosthesis simulator on mobility. Graefes Arch Clin Exp Ophthalmol 257, 1765–1770 (2019). https://doi.org/10.1007/s00417-019-04375-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04375-2