Abstract
Introduction
Dynasilan is a fluoroalkylsilan that is able to interact with surface active centres on intraocular lenses (IOL), offering a new way for surface modification of different IOL materials. The purpose of this in vitro study was to investigate the influence of this new surface modification on the adherence of two typical endophthalmitis causing bacteria (Staphylococcus epidermidis, Propionibacterium acnes).
Materials and methods
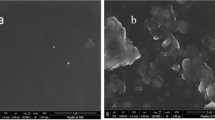
In a pilot experiment, the effect of Dynasilan coating on the adherence of S. epidermidis was tested on glass slides. Forty-two Dynasilan-modified and 42 unmodified IOL (14 PMMA, 14 silicone and 14 hydrogel) were incubated at 37°C in brain heart infusion broth (108 CFU/ml) with either S. epidermidis for 24 h or with P. acnes for 1 h. Subsequently, the adherent bacteria were resuspended using ultrasonification at 35 kHz for 3×45 s. After dilution series and incubation at 37°C on Petri dishes for 24 h and 3 days, respectively, the colonies were counted.
Results
In the pilot experiment, a markedly lower number of adherent S. epidermidis was observed on Dynasilan-modified glass slides. Of all IOL materials incubated with S. epidermidis, those modified with Dynasilan showed a lower mean number of adherent bacteria (mean 1.37×107; SD 2.37×107) than those untreated (2.43×107; SD 3.04×107).
IOLs incubated with P. acnes showed a significantly lower mean number of adherent bacteria of 2.51×104 (SD 2.71×104) on Dynasilan-modified IOLs versus 6.27×104 (SD 7.70×104) on untreated IOLs.
Conclusion
The presented in vitro results indicate that Dynasilan surface modification is able to reduce the adherence of S. epidermidis and P. acnes on all IOL materials tested.
Further studies regarding the stability of this modification and its biocompatibility must be performed.





Similar content being viewed by others
References
Basti S, Aasuri MK, Reddy MK, Preetam P, Reddy S, Gupa S, Naduvilath TJ (1999) Heparin-surface- modified intraocular lenses in pediatric cataract surgery: prospective randomized study. J Cataract Refract Surg 25:782–787
Cusumano A, Busin M, Spitznas M (1991) Is chronic intraocular inflammation after lens implantation of bacterial origin? Ophthalmology 98:1703–1710
Eloy R, Parrat D, Duc TM, Legeay G, Bechetoille A (1993) In vitro evaluation of inflammatory cell response after CF4 plasma surface modification of poly(methyl methacrylate) intraocular lenses. J Cataract Refract Surg 19:364–370
Fox GM, Joondeph BC, Flynn HW, Pflugfelder SC, Roussel TJ (1991) Delayed-onset pseudophakic endophthalmitis. Am J Ophthalmol 111:163–173
Gabriel MM, Ahearn DG, Chan KY, Patel AS (1998) In vitro adherence of Pseudomonas aeruginosa to four intraocular lenses. J Cataract Refract Surg 24:124–129
Garcia-Saenz MC, Arias-Puente A, Fresnadillo-Martinez MJ, Matilla-Rodriguez A (2000) In vitro adhesion of Staphylococcus epidermidis to intraocular lenses. J Cataract Refract Surg 26:1673–1679
Hoerauf H, Menz DH, Dresp J, Böse O, Laqua H (2000) Neue Wege zur Vermeidung von Silikonöladhäsionen auf Intraokularlinsen. In: Kohnen T, Ohrloff C, Wenzel M (eds) 13. Kongreβ der DGII. Springer, Berlin Heidelberg New York, pp 96–104
Kodjikian L, Burillon C, Roques C, Pellon G, Freney J, Renaud FN (2003) Bacterial adherence of Staphylococcus epidermidis to intraocular lenses: a bioluminescence and scanning electron microscopy study. Invest Ophthalmol Vis Sci 44:4388–4394
Lawin-Brüssel CA, Refojo MF, Kenyon KR (1992) In vitro adhesion of Pseudomonas aeruginosa and Staphylococcus epidermidis to surface passivated poly(methyl methacrylate) intraocular lenses. J Cataract Refract Surg 18:598–601
Legeais JM, Werner LP, Legeay G, Briat B, Renard G (1998) In vivo study of a fluorocarbon polymer-coated intraocular lens in a rabbit model. J Cataract Refract Surg 24:371–379
Lundberg F, Gouda I, Larm O, Galin MA, Ljungh A (1998) A new model to assess staphylococcal adhesion to intraocular lenses under in vitro flow conditions. Biomaterials 19:1727–1733
Miño de Kaspar H, Kollmann M, Klauß V (1993) Endophthalmitis. Bedeutung mikrobiologischer Untersuchungen für Therapie und Prognose. Ophthalmologe 90:726–736
Pinna A, Sechi LA, Zanetti S, Delogu D, Carta F (2000) Adherence of ocular isolates of Staphylococcus epidermidis to Acrysof intraocular lenses. A scanning electron microscopy and molecular biology study. Ophthalmology 107:2162–2166
Portolés M, Refojo MF, Leong FL (1993) Reduced bacterial adhesion to heparin-surface-modified intraocular lenses. J Cataract Refract Surg 19:755–759
Schlöricke E, Schmidt H, Schulze HA, Beck R, Guthoff R, Falkenhagen U (1997) Adhärenz von Staphylokokken unterschiedlicher Hydrophobizität. Untersuchung an verschiedenen Intraokularlinsen. Ophthalmologe 94:785–790
Speaker MG, Milch FA, Shah MK, Eisner W, Kreiswirth BN (1991) Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology 98:639–650
Sutherland IW (2001) The biofilm matrix—an immobilized but dynamic microbial environment. Trends Microbiol 9:222–227
Trocme SD, Li H (2000) Effect of heparin-surface-modified intraocular lenses on postoperative inflammation after phacoemulsification: a randomized trial in a United States patient population. Ophthalmology 107:1031–1037
Versura P, Torreggiani A, Cellini M, Caramazza R (1999) Adhesion mechanisms of human lens epithelial cells on 4 intraocular lens materials. J Cataract Refract Surg 25:527–533
Werner LP, Legeais JM, Durand J, Savoldelli M, Legeay G, Renard G (1997) Endothelial damage caused by uncoated and fluorocarbon-coated poly(methyl methacrylate) intraocular lenses. J Cataract Refract Surg 23:1013–1019
Werner L, Legeais JM, Nagel MD, Renard G (1999) Neutral red assay of the cytotoxicity of fluorocarbon-coated polymethylmethacrylate intraocular lenses in vitro. J Biomedical Mat Res 48:814–819
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kienast, A., Kämmerer, R., Weiss, C. et al. Influence of a new surface modification of intraocular lenses with fluoroalkylsilan on the adherence of endophthalmitis-causing bacteria in vitro. Graefe's Arch Clin Exp Ophthalmo 244, 1171–1177 (2006). https://doi.org/10.1007/s00417-005-0242-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0242-x