Abstract
Background
Myositis-associated antibodies (MAA) and myositis-specific antibodies (MSA) are detected in patients with idiopathic inflammatory myopathies (IIM); their role as diagnostic biomarkers is however still debated. The aim of our study was to assess the utility of MAA/MSA assessed by new line immunoassays in detecting myositis among neuromuscular patients.
Methods
We retrospectively analysed sera samples obtained from patients tested for myositis antibodies with the “Euroline: Autoimmune Inflammatory Myopathies 16Ag” and “myositis profile 3” kits (Mi-2, TIF1γ, MDA5, NXP2, SAE1, Jo-1, SRP, PL-7/12, EJ, OJ, Ro-52, Ku, PM-Scl75/100). First symptom, CK, EMG, muscle biopsy and diagnosis were also analysed. Using logistic regression analysis, two diagnostic models were built to evaluate the diagnostic power of MAA/MSA in distinguishing myositis patients from controls and other myopathies.
Results
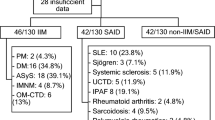
1229 patients were identified. 141 patients had a bioptic confirmed IIM; other diagnoses included: myopathy (n = 357), other neuromuscular diseases (n = 144) and no neuromuscular diseases (n = 587). The specificity was 95% for MSA and 89% for MAA, the sensitivity 20% and 22%, respectively. MAA showed no use in differentiating myositis patients from controls, whereas MSA had limited effect (OR = 5.165), compared to other variables as EMG (OR = 47.755) or CK > 2000 U/L (OR = 45.307). MSA were, however, the most useful parameter differentiating IIM from non-IIM patients (OR = 7.259), better than CK > 2000 U/L (OR = 4.033) and MAA (OR = 2.737).
Conclusions
Line immunoassays for myositis antibodies show high specificity but low sensitivity. Their usefulness as diagnostic biomarkers widely depends on the clinical settings. Our study suggests that MSA/MAA should be used for confirmatory and differential diagnosis rather than for screening purposes in inflammatory myopathies.




Similar content being viewed by others
References
Selva-O’Callaghan A, Pinal-Fernandez I, Trallero-Araguas E et al (2018) Classification and management of adult inflammatory myopathies. Lancet Neurol 17(9):816–828
Amato AA, Griggs RC (2003) Unicorns, dragons, polymyositis, and other mythological beasts. Neurology 61(3):288–289
Betteridge Z, McHugh N (2016) Myositis-specific autoantibodies: an important tool to support diagnosis of myositis. J Intern Med 280(1):8–23
Cavazzana I, Fredi M, Ceribelli A et al (2016) Testing for myositis specific autoantibodies: Comparison between line blot and immunoprecipitation assays in 57 myositis sera. J Immunol Methods 433:1–5
Ghirardello A, Zampieri S, Tarricone E et al (2006) Clinical implications of autoantibody screening in patients with autoimmune myositis. Autoimmunity 39(3):217–221
Zampeli E, Venetsanopoulou A, Argyropoulou OD et al (2018) Myositis autoantibody profiles and their clinical associations in Greek patients with inflammatory myopathies. Clin Rheumatol. https://doi.org/10.1007/s10067-018-4267-z
Palterer B, Vitiello G, Carraresi A et al (2018) Bench to bedside review of myositis autoantibodies. Clin Mol Allergy 16:5. https://doi.org/10.1186/s12948-018-0084-9
Ladislau L, Arouche-Delaperche L, Allenbach Y et al (2018) Potential pathogenic role of anti-signal recognition protein and anti-3-hydroxy-3-methylglutaryl-CoA reductase antibodies in immune-mediated necrotizing myopathies. Curr Rheumatol Rep 20(9):56. https://doi.org/10.1007/s11926-018-0763-z
Vulsteke JB, De Langhe E, Claeys KG et al (2018) Detection of myositis-specific antibodies. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2017-212915
Lundberg IE, Tjarnlund A, Bottai M et al (2017) 2017 European League Against Rheumatism/American College of rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Arthritis Rheumatol (Hoboken, NJ) 69(12):2271–2282
Tjärnlund A, Rönnelid J, Bottai M et al (2018) Response to: ‘Detection of myositis-specific antibodies’ by Vulsteke et al. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2018-212948
Mahler M, Fritzler MJ (2018) Detection of myositis-specific antibodies: additional notes. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2018-213153
Tjärnlund A, Lundberg IE, Rönnelid J (2018) Response to: ‘Detection of myositis-specific antibodies: additional notes’ by Infantino et al. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2018-213341
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (second of two parts). N Engl J Med 292(8):403–407
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292(7):344–347
Mariampillai K, Granger B, Amelin D et al (2018) Development of a new classification system for idiopathic inflammatory myopathies based on clinical manifestations and myositis-specific autoantibodies. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2018.2598
Lecouffe-Desprets M, Hémont C, Néel A et al (2018) Clinical contribution of myositis-related antibodies detected by immunoblot to idiopathic inflammatory myositis: a one-year retrospective study. Autoimmunity 51(2):89–95. https://doi.org/10.1080/08916934.2018.1441830
Dobloug C, Garen T, Bitter H et al (2015) Prevalence and clinical characteristics of adult polymyositis and dermatomyositis; data from a large and unselected Norwegian cohort. Ann Rheum Dis 74(8):1551–1556. https://doi.org/10.1136/annrheumdis-2013-205127
Gofrit SG, Yonath H, Lidar M et al (2018) The clinical phenotype of patients positive for antibodies to myositis and myositis-related disorders. Clin Rheumatol 37(5):1257–1263. https://doi.org/10.1007/s10067-018-4032-3
Cruellas MG, Viana Vdos S, Levy-Neto M et al (2013) Myositis-specific and myositis-associated autoantibody profiles and their clinical associations in a large series of patients with polymyositis and dermatomyositis. Clinics (Sao Paulo) 68(7):909–914. https://doi.org/10.6061/clinics/2013(07)04
Benveniste O, Drouot L, Jouen F et al (2011) Correlation of anti-signal recognition particle autoantibody levels with creatine kinase activity in patients with necrotizing myopathy. Arthritis Rheum 63(7):1961–1971. https://doi.org/10.1002/art.30344
Stone KB, Oddis CV, Fertig N et al (2007) Anti-Jo-1 antibody levels correlate with disease activity in idiopathic inflammatory myopathy. Arthritis Rheum 56(9):3125–3131
Hengstman GJ, van Brenk L, Vree Egberts WT et al (2005) High specificity of myositis specific autoantibodies for myositis compared with other neuromuscular disorders. J Neurol 252(5):534–537
Mammen AL, Casciola-Rosen L, Christopher-Stine L et al (2015) Myositis-specific autoantibodies are specific for myositis compared to genetic muscle disease. Neurol Neuroimmunol Neuroinflamm 2(6):e172. https://doi.org/10.1212/NXI.0000000000000172
Sener U, Martinez-Thompson J, Laughlin RS, Dimberg EL, Rubin DI (2018) Needle electromyography and histopathologic correlation in myopathies. Muscle Nerve. https://doi.org/10.1002/mus.26381
Naddaf E, Milone M, Mauermann ML, Mandrekar J, Litchy WJ (2018) Muscle biopsy and electromyography correlation. Front Neurol 9:839. https://doi.org/10.3389/fneur.2018.00839
Lundberg IE, de Visser M, Werth VP (2018) Classification of myositis. Nat Rev Rheumatol 14(5):269–278. https://doi.org/10.1038/nrrheum.2018.41
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare they have no conflict of interest to disclose.
Ethical standards
The study has been conducted in compliance with the principles of the declaration of Helsinki and with the local German laws and regulations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Montagnese, F., Babačić, H., Eichhorn, P. et al. Evaluating the diagnostic utility of new line immunoassays for myositis antibodies in clinical practice: a retrospective study. J Neurol 266, 1358–1366 (2019). https://doi.org/10.1007/s00415-019-09266-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09266-4