Abstract
Objectives
Maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) could be useful clinical parameters in monitoring many conditions including cystic fibrosis (CF). However, current protocols for undertaking the measurements lack standardization including the number of repeated attempts to achieve best values. We aimed to (a) determine the optimum number of attempts to achieve best MIP/MEP values, and (b) evaluate if the number of attempts is consistent across two different test days.
Methods
We analyzed data of a previous randomized controlled trial involving the effect of singing on respiratory muscle strength in 35 children with CF. On two different days (T1, T2) children performed MIP/MEP with at least ten attempts each to achieve < 10% repeatability.
Results
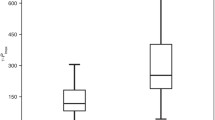
All children achieved repeatable MIP/MEP values within 10–11 attempts with 24 (68.6%) and 26 (74.3%) of these achieving best values of MIP and MEP, respectively, at attempts 6–11. Median values of the pressures by three, five, eight and all attempts significantly increased with more attempts (all p < 0.05). At T2, 56% required fewer attempts to achieve best values, but 32% required more attempts, indicating that the number of attempts required was inconsistent between test days.
Conclusion
It is likely that at least ten attempts (best two within < 10% variability) is required to achieve best and reliable MIP/MEP in children with CF. A larger sample size in children with CF and various conditions is required to consolidate these findings.


Similar content being viewed by others
Data Availability
All data and materials support this study claims and comply with field standards.
References
American Thoracic Society/European Respiratory Society (2002) ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med 166(4):518–624. https://doi.org/10.1164/rccm.166.4.518
Verma R, Chiang J, Qian H, Amin R (2019) Maximal static respiratory and sniff pressures in healthy children. A systematic review and meta-analysis. Ann Am Thorac Soc 16(4):478–487. https://doi.org/10.1513/AnnalsATS.201808-506OC
Heinzmann-Filho JP, Marostica PJC, Donadio M (2012) Ventilatory muscle strength in cystic fibrosis patients: a literature review. Monaldi Arch Chest Dis 77:134–138. https://doi.org/10.4081/monaldi.2012.147
Szeinberg A, England S, Mindorff C, Fraser IM, Levison H (1985) Maximal inspiratory and expiratory pressures are reduced in hyperinflated, malnourished, young adult male patients with cystic fibrosis. Am Rev Respir Dis 132(4):766–769. https://doi.org/10.1164/arrd.1985.132.4.766
Dekerlegand RL, Hadjiliadis D, Swisher AK, Parrott JS, Heuer AJ, Myslinski MJ (2015) Inspiratory muscle strength relative to disease severity in adults with stable cystic fibrosis. J Cyst Fibros 14(5):639–645. https://doi.org/10.1016/j.jcf.2015.05.003
Dassios T, Katelari A, Doudounakis S, Mantagos S, Dimitriou G (2013) Respiratory muscle function in patients with cystic fibrosis. Pediatr Pulmonol 48(9):865–873. https://doi.org/10.1002/ppul.22709
Laveneziana P, Albuquerque A, Aliverti A et al (2019) ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. https://doi.org/10.1183/13993003.01214-2018
Combret Y, Medrinal C, Bonnevie T, Gravier F-E, Le Roux P, Lamia B, Prieur G, Reychler G (2020) Clinimetric evaluation of muscle function tests for individuals with cystic fibrosis: a systematic review. J Cyst Fibros. https://doi.org/10.1016/j.jcf.2020.05.014
Fauroux B, Aubertin G (2007) Measurement of maximal pressures and the sniff manoeuvre in children. Paediatr Respir Rev 8(1):90–93. https://doi.org/10.1016/j.prrv.2007.02.006
Leech JA, Ghezzo H, Stevens D, Becklake MR (1983) Respiratory pressures and function in young adults. Am Rev Respir Dis 128(1):17–23. https://doi.org/10.1164/arrd.1983.128.1.17
Gaultier C, Zinman R (1983) Maximal static pressures in healthy children. Respir Physiol 51(1):45–61. https://doi.org/10.1016/0034-5687(83)90101-9
Wilson SH, Cooke NT, Edwards RH, Spiro SG (1984) Predicted normal values for maximal respiratory pressures in Caucasian adults and children. Thorax 39(7):535–538. https://doi.org/10.1136/thx.39.7.535
Wagener JS, Hibbert ME, Landau LI (1984) Maximal respiratory pressures in children. Am Rev Respir Dis 129(5):873–875. https://doi.org/10.1164/arrd.1984.129.5.873
Smyth RJ, Chapman KR, Rebuck AS (1984) Maximal inspiratory and expiratory pressures in adolescents. Norm Values Chest 86(4):568–572. https://doi.org/10.1378/chest.86.4.568
Szeinberg A, Marcotte JE, Roizin H, Mindorff C, England S, Tabachnik E, Levison H (1987) Normal values of maximal inspiratory and expiratory pressures with a portable apparatus in children, adolescents, and young adults. Pediatr Pulmonol 3(4):255–258. https://doi.org/10.1002/ppul.1950030411
Wen AS, Woo MS, Keens TG (1997) How many maneuvers are required to measure maximal inspiratory pressure accurately. Chest 111(3):802–807. https://doi.org/10.1378/chest.111.3.802
Stefanutti D, Fitting JW (1999) Sniff nasal inspiratory pressure. Reference values in Caucasian children. Am J Respir Crit Care Med 159(1):107–111. https://doi.org/10.1164/ajrccm.159.1.9804052
Rafferty GF, Leech S, Knight L, Moxham J, Greenough A (2000) Sniff nasal inspiratory pressure in children. Pediatr Pulmonol 29(6):468–475. https://doi.org/10.1002/(sici)1099-0496(200006)29:6%3c468::aid-ppul9%3e3.0.co;2-2
Tomalak W, Pogorzelski A, Prusak J (2002) Normal values for maximal static inspiratory and expiratory pressures in healthy children. Pediatr Pulmonol 34(1):42–46. https://doi.org/10.1002/ppul.10130
Windisch W, Hennings E, Sorichter S, Hamm H, Criee CP (2004) Peak or plateau maximal inspiratory mouth pressure: which is best? Eur Respir J 23(5):708–713. https://doi.org/10.1183/09031936.04.00136104
Heinzmann-Filho JP, Vasconcellos Vidal PC, Jones MH, Donadio MV (2012) Normal values for respiratory muscle strength in healthy preschoolers and school children. Respir Med 106(12):1639–1646. https://doi.org/10.1016/j.rmed.2012.08.015
Cox DW, Verheggen MM, Stick SM, Hall GL (2012) Characterization of maximal respiratory pressures in healthy children. Respiration 84(6):485–491. https://doi.org/10.1159/000342298
Mendes RE, Campos TF, Macedo TM, Borja RO, Parreira VF, Mendonca KM (2013) Prediction equations for maximal respiratory pressures of Brazilian adolescents. Braz J Phys Ther 17(3):218–226. https://doi.org/10.1590/s1413-35552012005000086
Arnall DA, Nelson AG, Owens B, Cebriai Iranzo MA, Sokell GA, Kanuho V, Interpreter C, Coast JR (2013) Maximal respiratory pressure reference values for Navajo children ages 6–14. Pediatr Pulmonol 48(8):804–808. https://doi.org/10.1002/ppul.22645
Gochicoa-Rangel LG, Moreno-Chavarria T, Rodriguez-Moreno L, Fernandez-Plata R, Martinez Briseno D, Torre-Bouscoulet L (2014) Maximal inspiratory and expiratory pressure in children: reference values. In: B54 respiratory function in early childhood American Thoracic Society International Conference Abstracts, New York, p. A3239
Gomes E, Peixoto-Souza F, Carvalho E, Nascimento E, Sampaio L, Eloi J, Magalhães A, Costa D (2014) Maximum respiratory pressures: values found and predicted in children. J Lung Pulm Respir Res. https://doi.org/10.15406/jlprr.2014.01.00014
Delgado RN, Campos TF, Borja Rde O, de Freitas DA, Chaves GS, de Mendonca KM (2015) Maximal respiratory pressures of healthy children: comparison between obtained and predicted values. Pediatr Phys Ther 27(1):31–37. https://doi.org/10.1097/pep.0000000000000100
da Rosa GJ, Morcillo AM, de Assumpcao MS, Schivinski CIS (2017) Predictive equations for maximal respiratory pressures of children aged 7–10. Braz J Phys Ther 21(1):30–36. https://doi.org/10.1016/j.bjpt.2016.04.002
Hulzebos E, Takken T, Reijneveld EA, Mulder MMG, Bongers BC (2018) Reference values for respiratory muscle strength in children and adolescents. Respiration 95(4):235–243. https://doi.org/10.1159/000485464
Irons JY, Kenny DT, McElrea M, Chang AB (2012) Singing therapy for young people with cystic fibrosis: a randomized controlled pilot study. Music Med 4(3):136–145. https://doi.org/10.1177/1943862112452150
Miller MR, Crapo R, Hankinson J et al (2005) General considerations for lung function testing. Eur Respir J 26(1):153–161. https://doi.org/10.1183/09031936.05.00034505
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343. https://doi.org/10.1183/09031936.00080312
Domenech-Clar R, Lopez-Andreu JA, Compte-Torrero L, De Diego-Damia A, Macian-Gisbert V, Perpina-Tordera M, Roques-Serradilla JM (2003) Maximal static respiratory pressures in children and adolescents. Pediatr Pulmonol 35(2):126–132. https://doi.org/10.1002/ppul.10217
Pellegrino R, Viegi G, Brusasco V et al (2005) Interpretative strategies for lung function tests. Eur Respir J 26(5):948–968. https://doi.org/10.1183/09031936.05.00035205
Volianitis S, McConnell AK, Jones DA (2001) Assessment of maximum inspiratory pressure. Respiration 68(1):22–27. https://doi.org/10.1159/000050458
Fiz J, Montserrat J, Picado C, Plaza V, Agusti-Vidal A (1989) How many manoeuvres should be done to measure maximal inspiratory mouth pressure in patients with chronic airflow obstruction? Thorax 44(5):419–421. https://doi.org/10.1136/thx.44.5.419
Aldrich TK, Spiro P (1995) Maximal inspiratory pressure: does reproducibility indicate full effort? Thorax 50(1):40–43. https://doi.org/10.1136/thx.50.1.40
Enright S, Unnithan VB, Davies D (2006) Reproducibility of measurements of inspiratory work capacity in cystic fibrosis patients. Respir Physiol Neurobiol 150(1):35–43. https://doi.org/10.1016/j.resp.2005.02.012
Trojan DA, Arnold DL, Shapiro S et al (2009) Fatigue in post-poliomyelitis syndrome: association with disease-related, behavioral, and psychosocial factors. PM&R 1(5):442–449. https://doi.org/10.1016/j.pmrj.2009.03.003
Funding
This study was not funded. WB is supported by an Asia–Pacific Society of Respirology short-term research/training scholarship (ID 2959) and a Charles Darwin University PhD scholarship. AC is supported by an Australian National Health and Medical Research Council (NHMRC) Practitioner Fellowship (APP1058213) and a top-up fellowship from the Children’s Hospital Foundation (Grant 50286). JM is supported by an Early Career Fellowship Grant from Queensland Children’s Hospital Foundation (RPC0772019).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by WB and MM. The children in the original RCT were recruited by JYI. The first draft of the manuscript was written by WB. MM, AC and JM were involved in preparation of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that they have no conflict of interest to disclose.
Ethical Approval
The questionnaire and methodology for this study was approved by the Human Research Ethics committee of Children’s Health Queensland (CHQ HREC 2007/104) for the original RCT and this current study.
Informed Consent
Written informed consent was obtained from the parents or legal guardians, and assent was obtained from children aged over 12 years. No identifiable information of participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boonjindasup, W., Chang, A.B., Marchant, J.M. et al. How Many Maneuvers Should We Do for Maximal Inspiratory and Expiratory Muscle Pressure Testing in Children: A Retrospective Review in Children with Cystic Fibrosis. Lung 199, 213–222 (2021). https://doi.org/10.1007/s00408-021-00422-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-021-00422-0