Abstract
Purpose
Current data show that maternal mental conditions affect about 10% of pregnant women worldwide. Assessing timing and patterns of mental health illness, therefore, is critical to ensure the wellbeing of the mother, the new-born and the whole family. The aim of this review is to summarize the latest evidence linking maternal mental disorders and adverse reproductive outcomes.
Methods
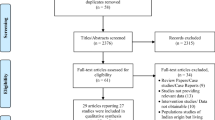
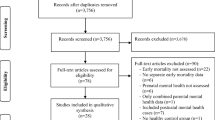
Following the PRISMA guidelines for systematic reviews, a literature search was conducted to ascertain the possible impact of mental health conditions on reproductive outcomes before and during pregnancy. The comprehensive strategy included cohort studies, randomised controlled trials and literature reviews on women with Primary Maternal Mental Illness (PMMI) and Secondary Maternal Mental Illness (SMMI) considering periconceptional, obstetric and foetal-neonatal outcomes. PubMed, WoS, CINAHL and Google scholar were used for the search. Cross-referencing in bibliographies of the selected papers ensured wider study capture.
Results
Evidence linking depressive disorders and infertility among PMMI is weak. Given this, women with prior mental conditions experience additional distress when undergoing fertility treatments. Primary mental disorders may also increase the risk of miscarriage and other pregnancy complications (e.g., gestational diabetes). For SMMI, there is more robust evidence correlating Preterm Birth (PTB) and Low Birth Weight (LBW) with common mental disorders which develop during pregnancy.
Conclusion
Prevention and management of maternal mental health diseases and minor mental conditions within the first 1000 days’ timeframe, should have a place in the holistic approach to women going through reproductive decisions, infertility treatment and pregnancy.

Similar content being viewed by others
References
Vigo D, Thornicroft G, Atun R (2016) Estimating the true global burden of mental illness. Lancet Psychiatry 3:171–178. https://doi.org/10.1016/S2215-0366(15)00505-2
Hay SI, Abajobir AA, Abate KH et al (2017) Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study. Lancet 390:1260–1344
World Health Organization (2018) Management of physical health conditions in adults with severe mental disorders: WHO guidelines. World Health Organization. Licence: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/bitstream/handle/10665/275718/9789241550383-eng.pdf
World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization. https://apps.who.int/iris/handle/10665/37958
Hendrick V (1998) Evaluation of mental health and depression during pregnancy. Psychopharmacol Bull 34:297–299
Rahman A, Fisher J, Bower P et al (2013) Interventions for common perinatal mental disorders in women in low-and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ 91:593–601. https://doi.org/10.2471/BLT.12.10981
Fisher J, Mello MC, Patel V et al (2012) Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bull World Health Organ 90:139–149G. https://doi.org/10.2471/BLT.11.09185
O'Hara MW, Wisner KL (2014) Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol 28:3–12. https://doi.org/10.1016/j.bpobgyn.2013.09.002
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1371/journal.pmed1000097
Hayden JA, Côté P, Bombardier C (2006) Evaluation of the quality of prognosis studies in systematic reviews. Ann Int Med 144:427–437. https://doi.org/10.7326/0003-4819-144-6-200603210-00010
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C (2013) Assessing bias in studies of prognostic factors. Ann Int Med. 158:280–286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
Prasad A, Schisterman EF, Schliep KC et al (2014) Depressive symptoms and their relationship with endogenous reproductive hormones and sporadic anovulation in premenopausal women. Ann Epidemiol 24:920–924. https://doi.org/10.1016/j.annepidem.2014.10.005
Baldur-Felskov B, Kjaer SK, Albieri V et al (2013) Psychiatric disorders in women with fertility problems: results from a large Danish register-based cohort study. Hum Reprod 28:683–690. https://doi.org/10.1093/humrep/des422
Pasch LA, Gregorich SE, Katz PK et al (2012) Psychological distress and in vitro fertilization outcome. Fertil Steril 98:459–464. https://doi.org/10.1016/j.fertnstert.2012.05.023
Gold KJ, Dalton VK, Schwenk TL et al (2007) What causes pregnancy loss? Preexisting mental illness as an independent risk factor. Gen Hosp Psychiatry 29:207–213. https://doi.org/10.1016/j.genhosppsych.2007.02.002
Gavin AR, Chae DH, Mustillo S et al (2009) Prepregnancy depressive mood and preterm birth in black and white women: findings from the CARDIA study. J Womens Health 18:803–811
Thornton D, Guendelman S, Hosang N (2010) Obstetric complications in women with diagnosed mental illness: the relative success of California’s county mental health system. Health Serv Res 45:246–264. https://doi.org/10.1111/j.1475-6773.2009.01058.x
Hizkiyahu R, Levy A, Sheiner E (2010) Pregnancy outcome of patients with schizophrenia. Am J Perinat 27:019–23
Wangel AM, Molin J, Moghaddassi M et al (2011) Prior psychiatric inpatient care and risk of cesarean sections: a registry study. J Psychosom Obstet Gynecol 32:189–197. https://doi.org/10.3109/0167482X.2011.626940
Witt WP, Wisk LE, Cheng ER et al (2012) Preconception mental health predicts pregnancy complications and adverse birth outcomes: a national population-based study. Matern Child Health J 16:1525–1541. https://doi.org/10.1007/s10995-011-0916-4
Sydsjö G, Möller L, Lilliecreutz C et al (2015) Psychiatric illness in women requesting caesarean section. BJOG 122:351–358. https://doi.org/10.1111/1471-0528.12714
Lassi ZS, Imam AM, Dean SV et al (2014) Preconception care: screening and management of chronic disease and promoting psychological health. Reprod Health 11:S5. https://doi.org/10.1186/1742-4755-11-S3-S5
Pare-Miron V, Czuzoj-Shulman N, Oddy L et al (2016) Effect of borderline personality disorder on obstetrical and neonatal outcomes. Womens Health Issues 26:190–195
Nilsson E, Hultman CM, Cnattingius S et al (2008) Schizophrenia and offspring’s risk for adverse pregnancy outcomes and infant death. Br J Psychiatry 193:311–315. https://doi.org/10.1192/bjp.bp.107.045146
Dayan J, Creveuil C, Marks MN et al (2006) Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med 68:938–946. https://doi.org/10.1097/01.psy.0000244025.20549.bd
Goedhart G, Snijders AC, Hesselink AE et al (2010) Maternal depressive symptoms in relation to perinatal mortality and morbidity: results from a large multiethnic cohort study. Psychosom Med 72:769–776
Szegda K, Markenson G, Bertone-Johnson ER et al (2014) Depression during pregnancy: a risk factor for adverse neonatal outcomes? A critical review of the literature. J Matern Fetal Neonatal Med 27:960–967. https://doi.org/10.3109/14767058.2013.845157
Niemi M, Falkenberg T, Petzold M et al (2013) Symptoms of antenatal common mental disorders, preterm birth and low birthweight: a prospective cohort study in a semi-rural district of Vietnam. Trop Med Int Health 18:687–695. https://doi.org/10.1111/tmi.12101
Grote NK, Bridge JA, Gavin AR et al (2010) A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 67:1012–1024. https://doi.org/10.1001/archgenpsychiatry.2010.111
Ding XX, Wu YL, Xu SJ et al (2014) Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord 20:103–110. https://doi.org/10.1016/j.jad.2014.02.027
Staneva A, Bogossian F, Pritchard M et al (2015) The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: a systematic review. Women Birth 28:179–193. https://doi.org/10.1016/j.wombi.2015.02.003
Brittain K, Myer L, Koen N et al (2015) Risk factors for antenatal depression and associations with infant birth outcomes: results from a South african birth cohort study. Paediatr Perinat Epidemiol 29:505–514. https://doi.org/10.1111/ppe.12216
Smith KF, Huber LR, Issel LM et al (2015) The association between maternal depression during pregnancy and adverse birth outcomes: a retrospective cohort study of PRAMS participants. J Community Health 40:984–992. https://doi.org/10.1007/s10900-015-0022-4
Liu C, Cnattingius S, Bergström M et al (2016) Prenatal parental depression and preterm birth: a national cohort study. BJOG 123:1973–1982. https://doi.org/10.1111/1471-0528.13891
Jarde A, Morais M, Kingston D et al (2016) Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry 73:826–837. https://doi.org/10.1001/jamapsychiatry.2016.0934
Szegda K, Bertone-Johnson ER, Pekow P et al (2017) Depression during pregnancy and adverse birth outcomes among predominantly Puerto Rican women. Matern Child Health J 21:942–952. https://doi.org/10.1007/s10995-016-2195-6
Van Ngo T, Gammeltoft T, Nguyen HT et al (2018) Antenatal depressive symptoms and adverse birth outcomes in Hanoi Vietnam. PLoS ONE 13:e0206650. https://doi.org/10.1371/journal.pone.0206650
Weobong B, ten Asbroek AH, Soremekun S et al (2014) Association of antenatal depression with adverse consequences for the mother and newborn in Rural Ghana: findings from the DON population-based cohort study. PLoS ONE 9:e116333. https://doi.org/10.1371/journal.pone.0116333
Ferri CP, Mitsuhiro SS, Barros MC et al (2007) The impact of maternal experience of violence and common mental disorders on neonatal outcomes: a survey of adolescent mothers in Sao Paulo Brazil. BMC Public Health 7:209. https://doi.org/10.1186/1471-2458-7-209
Nasreen HE, Kabir ZN, Forsell Y et al (2010) Low birth weight in offspring of women with depressive and anxiety symptoms during pregnancy: results from a population-based study in Bangladesh. BMC Public Health 10:515. https://doi.org/10.1186/1471-2458-10-515
Lewis AJ, Austin E, Galbally M (2016) Prenatal maternal mental health and fetal growth restriction: a systematic review. J Devel Orig Health Dis 7:416–428. https://doi.org/10.1017/S2040174416000076
Deave T, Heron J, Evans J et al (2008) The impact of maternal depression in pregnancy on early child development. BJOG 115:1043–1051. https://doi.org/10.1111/j.1471-0528.2008.01752.x
Muglia LJ, Katz M (2010) The enigma of spontaneous preterm birth. N Eng J Med 362:529–535
Gelenberg AJ, Dunner DL, Rothschild AJ et al (2013) Sexual functioning in patients with recurrent major depressive disorder enrolled in the PREVENT study. J Nerv Ment Dis 201:266–273. https://doi.org/10.1097/NMD.0b013e318288d298
Sujan AC, Rickert ME, Öberg AS et al (2017) Associations of maternal antidepressant use during the first trimester of pregnancy with preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/hyperactivity disorder in offspring. JAMA 317:1553–1562. https://doi.org/10.1001/jama.2017.3413
Prady SL, Hanlon I, Fraser LK et al (2018) A systematic review of maternal antidepressant use in pregnancy and short-and long-term offspring’s outcomes. Arch Womens Ment Health 21:127–140. https://doi.org/10.1007/s00737-017-0780-3
Vesga-Lopez O, Blanco C, Keyes K et al (2008) Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry 65:805–815. https://doi.org/10.1001/archpsyc.65.7.805
Schenker S, Yang Y, Mattiuz E et al (1999) Olanzapine transfer by human placenta. Clin Exp Pharmacol Physiol 26:691–697. https://doi.org/10.1046/j.1440-1681.1999.03111.x
Ewing G, Tatarchuk Y, Appleby D et al (2015) Placental transfer of antidepressant medications: implications for postnatal adaptation syndrome. Clin Pharmacokinet 54:359–370. https://doi.org/10.1007/s40262-014-0233-3
Vitale SG, Laganà AS, Muscatello MR et al (2016) Psychopharmacotherapy in pregnancy and breastfeeding. Obstet Gynecol Surv 71:721–733. https://doi.org/10.1097/OGX.0000000000000369
Bruno A, Laganà AS, Leonardi V et al (2018) Inside-out: the role of anger experience and expression in the development of postpartum mood disorders. J Matern Fetal Neonatal Med 31:3033–3038. https://doi.org/10.1080/14767058.2017.1362554
Singla D, Lazarus A, Atif N et al (2014) “Someone like us”: Delivering maternal mental health through peers in two South Asian contexts. J Affect Disord 168:452–458. https://doi.org/10.1016/j.jad.2014.07.017
Mehrotra A, Huskamp HA, Souza J et al (2017) Rapid growth in mental health telemedicine use among rural medicare beneficiaries, wide variation across states. Health Aff (Millwood) 36:909–917. https://doi.org/10.1377/hlthaff.2016.1461
Funding
The current literature review was developed in the frame of the project “Implementazione di un percorso formativo e informativo finalizzato ad un approccio integrato epigenetico per la prevenzione nei primi 1000 giorni di vita” funded by the Italian Ministry of Health—CCM aimed to update the current guidelines on parental preventive lifestyles before and during the first 1000 days of life. This funding was supported by the Italian Ministry of Health—CCM, CUP J59I17000320001.
Data availabilityNot applicable.
Code availabilityNot applicable.
Author information
Authors and Affiliations
Contributions
CM data collection, data management, data analysis and manuscript writing, GZ conceptualization, methodology, supervision, manuscript writing, manuscript editing, GC supervision, manuscript editing, AET supervision, manuscript editing, CB supervision, RB: supervision, SR project administration, supervision, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflicts of interest. Renata Bortolus is part of the Funding Board and has a role of supervision.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
About this article
Cite this article
Montagnoli, C., Zanconato, G., Cinelli, G. et al. Maternal mental health and reproductive outcomes: a scoping review of the current literature. Arch Gynecol Obstet 302, 801–819 (2020). https://doi.org/10.1007/s00404-020-05685-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05685-1