Abstract
Purpose
Urinary incontinence (UI) is a frequent and complex condition that negatively affects women’s quality of life (QoL). Weight loss and pelvic floor muscle training (PFMT) are first-line treatments of UI. The study aimed to reduce the symptoms of UI on QoL in overweight women by a multidisciplinary intervention including diet, physical exercise, and PFMT.
Methods
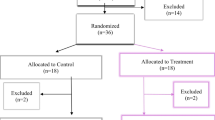
In this non-blinded prospective interventional study, women with stress or mixed UI were included in an intervention combining dietary counseling, physical exercise in groups, and individually planned PFMT. The primary outcome measure was the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF). The Patient Global Impression of Improvement (PGI-I) was used at 12 and 36 weeks. Also, anthropometric measures, pelvic floor muscle strength (PFMS), and physical performance were measured at baseline, 12, and 36 weeks. The primary aim of this study was to reduce the ICIQ-UI SF score by minimum of 2.6 points.
Results
Thirty-three women participated in the study. Nine dropped out during the intervention. The ICIQ-UI SF score was reduced by 6.8 and 4.5 points at 12 and 36 weeks, respectively. PGI-I revealed satisfaction with the results. Furthermore, weight was reduced by 2.6 and 3.6 kg at 12 and 36 weeks, respectively, and PFMS improved significantly.
Conclusion
Despite a limited mean weight loss of 3.6 kg, participants reported a significant decrease in the symptoms and the burden of UI. Using PFMT as an integrated part of the intervention might have contributed to the improvements and could be subject to future research.
Similar content being viewed by others
References
Coyne KS, Kvasz M, Ireland AM et al (2012) Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the UK, and the US. Eur Urol 61:88–95. https://doi.org/10.1016/j.eururo.2011.07.049
Schreiber Pedersen L, Lose G, Høybye MT et al (2017) Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand 96:939–948. https://doi.org/10.1111/aogs.13149
Vissers D, Neels H, Vermandel A et al (2014) The effect of non-surgical weight loss interventions on urinary incontinence in overweight women: a systematic review and meta-analysis. Obes Rev. https://doi.org/10.1111/obr.12170
Subak LL, Wing R, West D et al (2009) Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med 360:481–490. https://doi.org/10.1056/NEJMoa0806375.Weight
National Institute of Diabetes and Digestive and Kidney Diseases (2017) Overweight and Obesity Statistics. In: Heal. Stat. https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity. Accessed 3 Jan 2019
Eurostat - Statistics Explained (2014) Overweight and obesity—BMI statistics. https://ec.europa.eu/eurostat/statistics-explained/index.php/Overweight_and_obesity_-_BMI_statistics. Accessed 3 Jan 2019
Wing RR, Creasman JM, West DS, Richter HE (2010) Improving urinary incontinence in overweight and obese women through modest weight loss. Obstet Gynecol 116:284–292
National Institute for Health and Care Excellence (NICE) (2014) Weight management: lifestyle services for overweight or obese adults. http://www.nice.org.uk/guidance/ph53
Greaves CJ, Sheppard KE, Abraham C et al (2011) Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 11:119. https://doi.org/10.1186/1471-2458-11-119
Nambiar AK, Bosch R, Cruz F et al (2018) EAU guidelines on assessment and nonsurgical management of urinary incontinence. Eur Urol 73:596–609. https://doi.org/10.1016/j.eururo.2017.12.031
Strohacker K, Fazzino D, Breslin WL, Xu X (2015) The use of periodization in exercise prescriptions for inactive adults: a systematic review. Prev Med Rep 2:385–396. https://doi.org/10.1016/j.pmedr.2015.04.023
Avery K, Donovan J, Peters TJ et al (2004) ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 23:322–330. https://doi.org/10.1002/nau.20041
Yalcin I, Bump RC (2003) Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol 189:98–101
Ryhammer AM, Djurhuus JC, Laurberg S (1999) Pad testing in incontinent women: a review. Int Urogynecol J Pelvic Floor Dysfunct 10:111–115
Fletcher GF, Ades PA, Kligfield P et al (2013) Exercise standards for testing and training: a scientific statement from the American heart association. Circulation 128:873–934. https://doi.org/10.1161/CIR.0b013e31829b5b44
Andersson D (2004) The Åstrand–Ryhming test/method under the magnifying glass. A review of research articles. http://docplayer.net/32831104-The-astrand-ryhming-test-method-under-the-magnifying-glass.html
Rathleff CR, Baird WN, Olesen JL et al (2013) Hip and knee strength is not affected in 12–16 year old adolescents with patellofemoral pain—a cross-sectional population-based study. PLoS ONE 8:1–8. https://doi.org/10.1371/journal.pone.0079153
Bohannon RW, Magasi SR, Bubela DJ et al (2012) Grip and knee extension muscle strength reflect a common construct among adults. Muscle Nerve 46:555–558. https://doi.org/10.1002/mus.23350
Laycock J, Jerwood D (2001) Pelvic floor muscle assessment: The PERFECT scheme. Physiotherapy 87:631–642. https://doi.org/10.1016/S0031-9406(05)61108-X
Due U, Tibæk S, Valbjørn S, Colstrup V (2013) KNGF Guideline on Stress Urinary Incontinence, Danish Version. https://www.fysio.dk/globalassets/documents/fafo/kliniske-retningslinjer/gyn-obs-urologi/kr_stress-urininkontinens_2013.pdf
Andersen L (2010) Construct validity of a revised Physical Activity Scale and testing by cognitive interviewing. Scand J Public Health 38:707–714
Nyström E, Sjöström M, Stenlund H, Samuelsson E (2014) ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol Urodyn 34:747–751. https://doi.org/10.1002/nau.22657
Sirls LT, Tennstedt S, Brubaker L et al (2015) The minimum important difference for the INternational Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form in women with stress urinary incontinence. Neurourol Urodyn. https://doi.org/10.1002/nau
Karmakar D, Mostafa A, Abdel-Fattah M (2017) A new validated score for detecting patient-reported success on postoperative ICIQ-SF: a novel two-stage analysis from two large RCT cohorts. Int Urogynecol J 28:95–100. https://doi.org/10.1007/s00192-016-3070-0
Sand PK, Richardson DA, Staskin DR et al (1995) Pelvic floor electrical stimulation in the treatment of genuine stress incontinence: a multicenter, placebo-controlled trial. Am J Obstet Gynecol 173:72–79. https://doi.org/10.1016/0002-9378(95)90172-8
Pereira VS, Correia GN, Driusso P (2011) Individual and group pelvic floor muscle training versus no treatment in female stress urinary incontinence: a randomized controlled pilot study. Eur J Obstet Gynecol Reprod Biol 159:465–471. https://doi.org/10.1016/j.ejogrb.2011.09.003
Chevalier F, Fernandez-Lao C, Cuesta-Vargas AI (2014) Normal reference values of strength in pelvic floor muscle of women: a descriptive and inferential study. BMC Womens Health 14:143. https://doi.org/10.1186/s12905-014-0143-4
Alkharaiji M, Anyanwagu U, Donnelly R, Idris I (2018) Tier 3 specialist weight management service and pre-bariatric multicomponent weight management programmes for adults with obesity living in the UK: a systematic review. Endocrinol Diabetes Metab 2:e00042. https://doi.org/10.1002/edm2.42
Dursun M, Otunctemur A, Ozbek E et al (2014) Stress urinary incontinence and visceral adipose index: a new risk parameter. Int Urol Nephrol 46:2297–2300. https://doi.org/10.1007/s11255-014-0832-9
Brown TJ, O’Malley C, Blackshaw J et al (2017) Exploring the evidence base for Tier 3 weight management interventions for adults: a systematic review. Clin Obes 7:260–272. https://doi.org/10.1111/cob.12204
Funding
The study was undertaken with financial support from the Department of Health Promotion, Aalborg University Hospital, Denmark.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. AF: protocol/project development, data collection, data analysis, manuscript writing. LS protocol/project development, data collection, data analysis, manuscript writing. JA: project development, data analysis, manuscript editing. KG: project development, data analysis, manuscript editing. The first draft of the manuscript was written by Annette Fjerbæk and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study received all required approvals from the Danish Data Protection Agency (2008-58-0028) and the Scientific Ethical Committee (N-20150029) for the Region of North Denmark.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fjerbæk, A., Søndergaard, L., Andreasen, J. et al. Treatment of urinary incontinence in overweight women by a multidisciplinary lifestyle intervention. Arch Gynecol Obstet 301, 525–532 (2020). https://doi.org/10.1007/s00404-019-05371-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05371-x