Abstract
Introduction
The reliability of joint line tenderness was previously investigated among other clinical tests for the diagnosis of meniscal pathology with variable results. The aim of this study was to evaluate and compare the accuracy of joint line tenderness as a clinical diagnosing test for arthroscopically confirmed meniscal tears between males and females.
Materials and methods
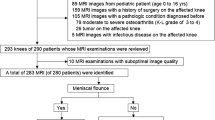
For the purpose of preoperative joint line tenderness accuracy calculations, this study included male and female groups of patients who have had knee arthroscopy following preoperative diagnosis of meniscal tear. Overall, 195 patients were included in the study, 134 males and 61 females. The mean age was 43.4 (13–76) years.
Results
In the male group, the diagnosis of meniscal tear by joint line tenderness was correct in 84 (62.7 %) of 134 knees for the medial side and in 115 (85.8 %) for the lateral side. In the female group, the diagnosis was correct in 35 (57.4 %) of 61 knees for the medial side and in 57 (93.4 %) for the lateral side. In order to refine the accuracy of medial joint line tenderness, the data were recalculated for patients with medial meniscal tears and no chondral lesion or cruciate ligament tears; however, the accuracy remained low.
Conclusions
The physical finding of joint line tenderness of the knee as a test for lateral meniscal tear was found reliable in both males and females. For medial meniscal tears, the test had low reliability and thus less useful if used alone, in both genders.
Similar content being viewed by others
References
Galli M, Ciriello V, Menghi A, Aulisa AG, Rabini A, Marzetti E (2013) Joint line tenderness and McMurray tests for the detection of meniscal lesions: what is their real diagnostic value? Arch Phys Med Rehabil 94(6):1126–1131
Malanga GA, Andrus S, Nadler SF, McLean J (2003) Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil 84(4):592–603
Scholten RJ, Deville WL, Opstelten W, Bijl D, van der Plas CG, Bouter LM (2001) The accuracy of physical diagnostic tests for assessing meniscal lesions of the knee: a meta-analysis. J FamPract 50:938–944
Fowler PJ, Lubliner JA (1989) The predictive value of five clinical signs in the evaluation of meniscal pathology. Arthroscopy 5:184–186
Akseki D, Ozcan O, Boya H, Pinar H (2004) A new weight-bearing meniscal test and a comparison with McMurray’s test and joint line tenderness. Arthroscopy 20(9):951–958
Karachalios T, Hantes M, Zibis AH, Zachos V, Karantanas AH, Malizos KN (2005) Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Joint Surg Am 87(5):955–962
Eren OT (2003) The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy 19:850–854
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85(Suppl 2):58–69
Oberlander MA, Shalvoy RM, Hughston JC (1993) The accuracy of the clinical knee examination documented by arthroscopy. A prospective study. Am J Sports Med 21:773–778
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no financial relationships.
Rights and permissions
About this article
Cite this article
Haviv, B., Bronak, S., Kosashvili, Y. et al. Gender differences in the accuracy of joint line tenderness for arthroscopically confirmed meniscal tears. Arch Orthop Trauma Surg 135, 1567–1570 (2015). https://doi.org/10.1007/s00402-015-2305-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2305-8