Abstract
Purpose
Probiotics have been reported to be beneficial for inflammatory bowel disease (IBD), but the types, number of strains, dosage, and intervention time of probiotics used remain controversial. Furthermore, the changes of gut microbiota in IBD’s patients are also intriguing. Thus, this meta-analysis was to explore the clinical effects and gut microbiota changes of using probiotics, prebiotics and synbiotics in IBD.
Methods
The search was performed in PubMed, Web of Science and the Cochrane library from inception to April 2020. Qualified randomized controlled trials were included. IBD’s remission rate, disease activity index and recurrence rate were extracted and analyzed. Changes in the gut microbiota of patients with IBD are comprehensively described.
Results
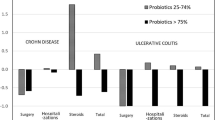
Thirty-eight articles were included. Probiotics, prebiotics and synbiotics can induce/maintain IBD’s remission and reduce ulcerative colitis (UC) disease activity index (RR = 1.13, 95% CI 1.02, 1.26, P < 0.05; SMD = 1.00, 95% CI 0.27, 1.73, P < 0.05). In subgroup analyses of IBD remission rate and UC disease activity index, we obtained some statistically significant results in some subgroup (P < 0.05). To some extent, probiotic supplements can increase the number of beneficial bacteria (especially Bifidobacteria) in the intestinal tract of patients with IBD.
Conclusions
Our results support the treatment of IBD (especially UC) with pro/pre/synbiotics, and synbiotics are more effective. Probiotic supplements that are based on Lactobacillus and Bifidobacterium or more than one strain are more likely to be beneficial for IBD remission. The dose of 1010–1012 CFU/day may be a reference range for using probiotics to relieve IBD.







Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Change history
24 May 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00394-021-02592-2
References
Jairath V, Feagan BG (2020) Global burden of inflammatory bowel disease. Lancet Gastroenterol Hepatol 5(1):2–3. https://doi.org/10.1016/s2468-1253(19)30358-9
Alatab S, Sepanlou SG, Ikuta K, Vahedi H, Bisignano C, Safiri S, Sadeghi A, Nixon MR, Abdoli A, Abolhassani H, Alipour V, Almadi MAH, Almasi-Hashiani A, Anushiravani A, Arabloo J, Atique S, Awasthi A, Badawi A, Baig AAA, Bhala N, Bijani A, Biondi A, Borzì AM, Burke KE, Carvalho F, Daryani A, Dubey M, Eftekhari A, Fernandes E, Fernandes JC, Fischer F, Haj-Mirzaian A, Haj-Mirzaian A, Hasanzadeh A, Hashemian M, Hay SI, Hoang CL, Househ M, Ilesanmi OS, Jafari Balalami N, James SL, Kengne AP, Malekzadeh MM, Merat S, Meretoja TJ, Mestrovic T, Mirrakhimov EM, Mirzaei H, Mohammad KA, Mokdad AH, Monasta L, Negoi I, Nguyen TH, Nguyen CT, Pourshams A, Poustchi H, Rabiee M, Rabiee N, Ramezanzadeh K, Rawaf DL, Rawaf S, Rezaei N, Robinson SR, Ronfani L, Saxena S, Sepehrimanesh M, Shaikh MA, Sharafi Z, Sharif M, Siabani S, Sima AR, Singh JA, Soheili A, Sotoudehmanesh R, Suleria HAR, Tesfay BE, Tran B, Tsoi D, Vacante M, Wondmieneh AB, Zarghi A, Zhang Z-J, Dirac M, Malekzadeh R, Naghavi M (2020) The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 5(1):17–30. https://doi.org/10.1016/s2468-1253(19)30333-4
Kaplan GG (2015) The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol 12(12):720–727. https://doi.org/10.1038/nrgastro.2015.150
Mak WY, Zhao M, Ng SC, Burisch J (2020) The epidemiology of inflammatory bowel disease: east meets west. J Gastroenterol Hepatol 35(3):380–389. https://doi.org/10.1111/jgh.14872
McDowell C, Farooq U, Haseeb M (2020) Inflammatory bowel disease (IBD). In: StatPearls. StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC., Treasure Island (FL)
Guzman-Prado Y, Samson O, Segal JP, Limdi JK, Hayee B (2020) Vitamin D therapy in adults with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis. https://doi.org/10.1093/ibd/izaa087
Peng L, Zhong Y, Wang A, Jiang Z (2019) Probiotics combined with aminosalicylic acid affiliates remission of ulcerative colitis: a meta-analysis of randomized controlled trial. Biosci Rep. https://doi.org/10.1042/BSR20180943
Asto E, Mendez I, Audivert S, Farran-Codina A, Espadaler J (2019) The efficacy of probiotics, prebiotic inulin-type fructans, and synbiotics in human ulcerative colitis: a systematic review and meta-analysis. Nutrients. https://doi.org/10.3390/nu11020293
Rufino MN, Aleixo GFP, Trombine-Batista IE, Giuffrida R, Keller R, Bremer-Neto H (2018) Systematic review and meta-analysis of preclinical trials demonstrate robust beneficial effects of prebiotics in induced inflammatory bowel disease. J Nutr Biochem 62:1–8. https://doi.org/10.1016/j.jnutbio.2018.05.016
Jakubczyk D, Leszczynska K, Gorska S (2020) The effectiveness of probiotics in the treatment of inflammatory bowel disease (IBD)-a critical review. Nutrients. https://doi.org/10.3390/nu12071973
Pandey KR, Naik SR, Vakil BV (2015) Probiotics, prebiotics and synbiotics- a review. J Food Sci Technol 52(12):7577–7587. https://doi.org/10.1007/s13197-015-1921-1
Cruz BCS, Sarandy MM, Messias AC, Goncalves RV, Ferreira C, Peluzio MCG (2020) Preclinical and clinical relevance of probiotics and synbiotics in colorectal carcinogenesis: a systematic review. Nutr Rev. https://doi.org/10.1093/nutrit/nuz087
Plaza-Diaz J, Ruiz-Ojeda FJ, Gil-Campos M, Gil A (2019) Mechanisms of action of probiotics. Adv Nutr 10(suppl_1):S49–S66. https://doi.org/10.1093/advances/nmy063
Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, Scott K, Stanton C, Swanson KS, Cani PD, Verbeke K, Reid G (2017) Expert consensus document: the International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol 14(8):491–502. https://doi.org/10.1038/nrgastro.2017.75
Mohanty D, Misra S, Mohapatra S, Sahu PS (2018) Prebiotics and synbiotics: recent concepts in nutrition. Food Biosci 26:152–160. https://doi.org/10.1016/j.fbio.2018.10.008
Angelino D, Martina A, Rosi A, Veronesi L, Antonini M, Mennella I, Vitaglione P, Grioni S, Brighenti F, Zavaroni I, Fares C, Torriani S, Pellegrini N (2019) Glucose- and lipid-related biomarkers are affected in healthy obese or hyperglycemic adults consuming a whole-grain pasta enriched in prebiotics and probiotics: a 12-week randomized controlled trial. J Nutr 149(10):1714–1723. https://doi.org/10.1093/jn/nxz071
Yoshimatsu Y, Yamada A, Furukawa R, Sono K, Osamura A, Nakamura K, Aoki H, Tsuda Y, Hosoe N, Takada N, Suzuki Y (2015) Effectiveness of probiotic therapy for the prevention of relapse in patients with inactive ulcerative colitis. World J Gastroenterol 21(19):5985–5994. https://doi.org/10.3748/wjg.v21.i19.5985
Amiriani T, Rajabli N, Faghani M, Besharat S, Roshandel G, Akhavan Tabib A, Joshaghani H (2020) Effect of Lactocare(R) synbiotic on disease severity in ulcerative colitis: a randomized placebo-controlled double-blind clinical trial. Middle East J Dig Dis 12(1):27–33. https://doi.org/10.15171/mejdd.2020.160
Tamaki H, Nakase H, Inoue S, Kawanami C, Itani T, Ohana M, Kusaka T, Uose S, Hisatsune H, Tojo M, Noda T, Arasawa S, Izuta M, Kubo A, Ogawa C, Matsunaka T, Shibatouge M (2016) Efficacy of probiotic treatment with Bifidobacterium longum 536 for induction of remission in active ulcerative colitis: a randomized, double-blinded, placebo-controlled multicenter trial. Dig Endosc 28(1):67–74. https://doi.org/10.1111/den.12553
Kato K, Mizuno S, Umesaki Y, Ishii Y, Sugitani M, Imaoka A, Otsuka M, Hasunuma O, Kurihara R, Iwasaki A, Arakawa Y (2004) Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment Pharmacol Ther 20(10):1133–1141. https://doi.org/10.1111/j.1365-2036.2004.02268.x
Matsuoka K, Uemura Y, Kanai T, Kunisaki R, Suzuki Y, Yokoyama K, Yoshimura N, Hibi T (2018) Efficacy of Bifidobacterium breve fermented milk in maintaining remission of ulcerative colitis. Dig Dis Sci 63(7):1910–1919. https://doi.org/10.1007/s10620-018-4946-2
Wildt S, Nordgaard I, Hansen U, Brockmann E, Rumessen JJ (2011) A randomised double-blind placebo-controlled trial with Lactobacillus acidophilus La-5 and Bifidobacterium animalis subsp. lactis BB-12 for maintenance of remission in ulcerative colitis. J Crohn’s Colitis 5(2):115–121. https://doi.org/10.1016/j.crohns.2010.11.004
Jiang Y, Zhang ZG, Qi FX, Zhang Y, Han T (2016) Comparison of maintenance effect of probiotics and aminosalicylates on ulcerative colitis: a meta-analysis of randomized controlled trials. Chronic Dis Transl Med 2(1):34–41. https://doi.org/10.1016/j.cdtm.2016.07.002
Mardini HE, Grigorian AY (2014) Probiotic mix VSL#3 is effective adjunctive therapy for mild to moderately active ulcerative colitis: a meta-analysis. Inflamm Bowel Dis 20(9):1562–1567. https://doi.org/10.1097/MIB.0000000000000084
Derwa Y, Gracie DJ, Hamlin PJ, Ford AC (2017) Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease. Aliment Pharmacol Ther 46(4):389–400. https://doi.org/10.1111/apt.14203
Ganji-Arjenaki M, Rafieian-Kopaei M (2018) Probiotics are a good choice in remission of inflammatory bowel diseases: a meta analysis and systematic review. J Cell Physiol 233(3):2091–2103. https://doi.org/10.1002/jcp.25911
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration. https://training.cochrane.org/handbook. Accessed 21 July 2020
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Hu Y, Amoah AN, Zhang H, Fu R, Qiu Y, Cao Y, Sun Y, Chen H, Liu Y, Lyu Q (2020) Effect of ginger in the treatment of nausea and vomiting compared with vitamin B6 and placebo during pregnancy: a meta-analysis. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2020.1712714
Fan H, Du J, Liu X, Zheng WW, Zhuang ZH, Wang CD, Gao R (2019) Effects of pentasa-combined probiotics on the microflora structure and prognosis of patients with inflammatory bowel disease. Turk J Gastroenterol 30(8):680–685. https://doi.org/10.5152/tjg.2019.18426
Sanchez-Morales A, Perez-Ayala MF, Cruz-Martinez M, Arenas-Osuna J, Ramirez-Mendoza P, Ceniceros RA, Mora-Canas EM, Cruz-Dominguez P, Saavedra-Salinas MA (2019) Probiotics’ effectiveness on symptoms, histological features and feeding tolerance in ulcerative colitis. Revista medica del Instituto Mexicano del Seguro Social 57(1):9–14
Bjarnason I, Sission G, Hayee B (2019) A randomised, double-blind, placebo-controlled trial of a multi-strain probiotic in patients with asymptomatic ulcerative colitis and Crohn’s disease. Inflammopharmacology 27(3):465–473. https://doi.org/10.1007/s10787-019-00595-4
Kamarli Altun H, Akal Yildiz E, Akin M (2019) Effects of synbiotic therapy in mild-to-moderately active ulcerative colitis: a randomized placebo-controlled study. Turk J Gastroenterol 30(4):313–320. https://doi.org/10.5152/tjg.2019.18356
Huang M, Chen Z, Lang C, Chen J, Yang B, Xue L, Zhang Y (2018) Efficacy of mesalazine in combination with bifid triple viable capsules on ulcerative colitis and the resultant effect on the inflammatory factors. Pak J Pharm Sci 31(6(Special)):2891–2895
Su H, Kang Q, Wang H, Yin H, Duan L, Liu Y, Fan R (2018) Effects of glucocorticoids combined with probiotics in treating Crohn’s disease on inflammatory factors and intestinal microflora. Exp Ther Med 16(4):2999–3003. https://doi.org/10.3892/etm.2018.6559
Petersen AM, Mirsepasi H, Halkjaer SI, Mortensen EM, Nordgaard-Lassen I, Krogfelt KA (2014) Ciprofloxacin and probiotic Escherichia coli Nissle add-on treatment in active ulcerative colitis: a double-blind randomized placebo controlled clinical trial. J Crohns Colitis 8(11):1498–1505. https://doi.org/10.1016/j.crohns.2014.06.001
Bourreille A, Cadiot G, Le Dreau G, Laharie D, Beaugerie L, Dupas JL, Marteau P, Rampal P, Moyse D, Saleh A, Le Guern ME, Galmiche JP, Group FS (2013) Saccharomyces boulardii does not prevent relapse of Crohn’s disease. Clin Gastroenterol Hepatol 11(8):982–987. https://doi.org/10.1016/j.cgh.2013.02.021
Li G, Zeng S, Liao W, Lv N (2012) The effect of bifid triple viable on immune function of patients with ulcerative colitis. Gastroenterol Res Pract. https://doi.org/10.1155/2012/404752
Benjamin JL, Hedin CR, Koutsoumpas A, Ng SC, McCarthy NE, Hart AL, Kamm MA, Sanderson JD, Knight SC, Forbes A, Stagg AJ, Whelan K, Lindsay JO (2011) Randomised, double-blind, placebo-controlled trial of fructo-oligosaccharides in active Crohn’s disease. Gut 60(7):923–929. https://doi.org/10.1136/gut.2010.232025
Steed H, Macfarlane GT, Blackett KL, Bahrami B, Reynolds N, Walsh SV, Cummings JH, Macfarlane S (2010) Clinical trial: the microbiological and immunological effects of synbiotic consumption - a randomized double-blind placebo-controlled study in active Crohn’s disease. Aliment Pharmacol Ther 32(7):872–883. https://doi.org/10.1111/j.1365-2036.2010.04417.x
Tursi A, Brandimarte G, Papa A, Giglio A, Elisei W, Giorgetti GM, Forti G, Morini S, Hassan C, Pistoia MA, Modeo ME, Rodino S, D’Amico T, Sebkova L, Sacca N, Di Giulio E, Luzza F, Imeneo M, Larussa T, Di Rosa S, Annese V, Danese S, Gasbarrini A (2010) Treatment of relapsing mild-to-moderate ulcerative colitis with the probiotic VSL#3 as adjunctive to a standard pharmaceutical treatment: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol 105(10):2218–2227. https://doi.org/10.1038/ajg.2010.218
Sood A, Midha V, Makharia GK, Ahuja V, Singal D, Goswami P, Tandon RK (2009) The probiotic preparation, VSL#3 induces remission in patients with mild-to-moderately active ulcerative colitis. Clin Gastroenterol Hepatol 7(11):1202–1209. https://doi.org/10.1016/j.cgh.2009.07.016
Miele E, Pascarella F, Giannetti E, Quaglietta L, Baldassano RN, Staiano A (2009) Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am J Gastroenterol 104(2):437–443. https://doi.org/10.1038/ajg.2008.118
Hafer A, Kramer S, Duncker S, Kruger M, Manns MP, Bischoff SC (2007) Effect of oral lactulose on clinical and immunohistochemical parameters in patients with inflammatory bowel disease: a pilot study. BMC Gastroenterol 7:36. https://doi.org/10.1186/1471-230x-7-36
Casellas F, Borruel N, Torrejon A, Varela E, Antolin M, Guarner F, Malagelada JR (2007) Oral oligofructose-enriched inulin supplementation in acute ulcerative colitis is well tolerated and associated with lowered faecal calprotectin. Aliment Pharmacol Ther 25(9):1061–1067. https://doi.org/10.1111/j.1365-2036.2007.03288.x
Zocco MA, dal Verme LZ, Cremonini F, Piscaglia AC, Nista EC, Candelli M, Novi M, Rigante D, Cazzato IA, Ojetti V, Armuzzi A, Gasbarrini G, Gasbarrini A (2006) Efficacy of Lactobacillus GG in maintaining remission of ulcerative colitis. Aliment Pharmacol Ther 23(11):1567–1574. https://doi.org/10.1111/j.1365-2036.2006.02927.x
Bousvaros A, Guandalini S, Baldassano RN, Botelho C, Evans J, Ferry GD, Goldin B, Hartigan L, Kugathasan S, Levy J, Murray KF, Oliva-Hemker M, Rosh JR, Tolia V, Zholudev A, Vanderhoof JA, Hibberd PL (2005) A randomized, double-blind trial of Lactobacillus GG versus placebo in addition to standard maintenance therapy for children with Crohn’s disease. Inflamm Bowel Dis 11(9):833–839. https://doi.org/10.1097/01.mib.0000175905.00212.2c
Furrie E, Macfarlane S, Kennedy A, Cummings JH, Walsh SV, O’Neil DA, Macfarlane GT (2005) Synbiotic therapy (Bifidobacterium longum/Synergy 1) initiates resolution of inflammation in patients with active ulcerative colitis: a randomised controlled pilot trial. Gut 54(2):242–249. https://doi.org/10.1136/gut.2004.044834
Tursi A, Brandimarte G, Giorgetti GM, Forti G, Modeo ME, Gigliobianco A (2004) Low-dose balsalazide plus a high-potency probiotic preparation is more effective than balsalazide alone or mesalazine in the treatment of acute mild-to-moderate ulcerative colitis. Med Sci Monit 10(11):Pi126-131
Kruis W, Fric P, Pokrotnieks J, Lukas M, Fixa B, Kascak M, Kamm MA, Weismueller J, Beglinger C, Stolte M, Wolff C, Schulze J (2004) Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 53(11):1617–1623. https://doi.org/10.1136/gut.2003.037747
Cui HH, Chen CL, Wang JD, Yang YJ, Cun Y, Wu JB, Liu YH, Dan HL, Jian YT, Chen XQ (2004) Effects of probiotic on intestinal mucosa of patients with ulcerative colitis. World J Gastroenterol 10(10):1521–1525. https://doi.org/10.3748/wjg.v10.i10.1521
Schultz M, Timmer A, Herfarth HH, Sartor RB, Vanderhoof JA, Rath HC (2004) Lactobacillus GG in inducing and maintaining remission of Crohn’s disease. BMC Gastroenterol 4:5. https://doi.org/10.1186/1471-230x-4-5
Guslandi M, Mezzi G, Sorghi M, Testoni PA (2000) Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Dig Dis Sci 45(7):1462–1464. https://doi.org/10.1023/a:1005588911207
Rembacken BJ, Snelling AM, Hawkey PM, Chalmers DM, Axon AT (1999) Non-pathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: a randomised trial. Lancet 354(9179):635–639. https://doi.org/10.1016/s0140-6736(98)06343-0
Kruis W, Schutz E, Fric P, Fixa B, Judmaier G, Stolte M (1997) Double-blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Aliment Pharmacol Ther 11(5):853–858. https://doi.org/10.1046/j.1365-2036.1997.00225.x
Yilmaz I, Dolar ME, Ozpinar H (2019) Effect of administering kefir on the changes in fecal microbiota and symptoms of inflammatory bowel disease: a randomized controlled trial. Turk J Gastroenterol 30(3):242–253. https://doi.org/10.5152/tjg.2018.18227
Shadnoush M, Hosseini RS, Khalilnezhad A, Navai L, Goudarzi H, Vaezjalali M (2015) Effects of probiotics on gut microbiota in patients with inflammatory bowel disease: a double-blind, placebo-controlled clinical trial. Korean J Gastroenterol 65(4):215–221. https://doi.org/10.4166/kjg.2015.65.4.215
De Preter V, Joossens M, Ballet V, Shkedy Z, Rutgeerts P, Vermeire S, Verbeke Phd K (2013) Metabolic profiling of the impact of oligofructose-enriched inulin in Crohn’s disease patients: a double-blinded randomized controlled trial. Clin Transl Gastroenterol 4:e30. https://doi.org/10.1038/ctg.2012.24
Joossens M, De Preter V, Ballet V, Verbeke K, Rutgeerts P, Vermeire S (2012) Effect of oligofructose-enriched inulin (OF-IN) on bacterial composition and disease activity of patients with Crohn’s disease: results from a double-blinded randomised controlled trial. Gut 61(6):958. https://doi.org/10.1136/gutjnl-2011-300413
Ishikawa H, Matsumoto S, Ohashi Y, Imaoka A, Setoyama H, Umesaki Y, Tanaka R, Otani T (2011) Beneficial effects of probiotic bifidobacterium and galacto-oligosaccharide in patients with ulcerative colitis: a randomized controlled study. Digestion 84(2):128–133. https://doi.org/10.1159/000322977
Ishikawa H, Akedo I, Umesaki Y, Tanaka R, Imaoka A, Otani T (2003) Randomized controlled trial of the effect of bifidobacteria-fermented milk on ulcerative colitis. J Am Coll Nutr 22(1):56–63. https://doi.org/10.1080/07315724.2003.10719276
Shinde T, Perera AP, Vemuri R, Gondalia SV, Karpe AV, Beale DJ, Shastri S, Southam B, Eri R, Stanley R (2019) Synbiotic supplementation containing whole plant sugar cane fibre and probiotic spores potentiates protective synergistic effects in mouse model of IBD. Nutrients. https://doi.org/10.3390/nu11040818
Shen J, Zuo ZX, Mao AP (2014) Effect of probiotics on inducing remission and maintaining therapy in ulcerative colitis, Crohn’s disease, and pouchitis: meta-analysis of randomized controlled trials. Inflamm Bowel Dis 20(1):21–35. https://doi.org/10.1097/01.MIB.0000437495.30052.be
Chen MY, Qiu ZW, Tang HM, Zhuang KH, Cai QQ, Chen XL, Li HB (2019) Efficacy and safety of bifid triple viable plus aminosalicylic acid for the treatment of ulcerative colitis: a systematic review and meta-analysis. Medicine 98(47):e17955. https://doi.org/10.1097/MD.0000000000017955
Fujiya M, Ueno N, Kohgo Y (2014) Probiotic treatments for induction and maintenance of remission in inflammatory bowel diseases: a meta-analysis of randomized controlled trials. Clin J Gastroenterol 7(1):1–13. https://doi.org/10.1007/s12328-013-0440-8
Ghouri YA, Richards DM, Rahimi EF, Krill JT, Jelinek KA, DuPont AW (2014) Systematic review of randomized controlled trials of probiotics, prebiotics, and synbiotics in inflammatory bowel disease. Clin Exp Gastroenterol 7:473–487. https://doi.org/10.2147/CEG.S27530
Zheng HJ, Guo J, Wang Q, Wang L, Wang Y, Zhang F, Huang WJ, Zhang W, Liu WJ, Wang Y (2020) Probiotics, prebiotics, and synbiotics for the improvement of metabolic profiles in patients with chronic kidney disease: a systematic review and meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. https://doi.org/10.1080/10408398.2020.1740645
Coqueiro AY, Raizel R, Bonvini A, Tirapegui J, Rogero MM (2019) Probiotics for inflammatory bowel diseases: a promising adjuvant treatment. Int J Food Sci Nutr 70(1):20–29. https://doi.org/10.1080/09637486.2018.1477123
Celiberto LS, Bedani R, Rossi EA, Cavallini DC (2017) Probiotics: the scientific evidence in the context of inflammatory bowel disease. Crit Rev Food Sci Nutr 57(9):1759–1768. https://doi.org/10.1080/10408398.2014.941457
Aggeletopoulou I, Konstantakis C, Assimakopoulos SF, Triantos C (2019) The role of the gut microbiota in the treatment of inflammatory bowel diseases. Microb Pathog 137:103774. https://doi.org/10.1016/j.micpath.2019.103774
Darb Emamie A, Rajabpour M, Ghanavati R, Asadolahi P, Farzi S, Sobouti B, Darbandi A (2020) The effects of probiotics, prebiotics and synbiotics on the reduction of IBD complications, a periodic review during 2009–2020. J Appl Microbiol. https://doi.org/10.1111/jam.14907
Glassner KL, Abraham BP, Quigley EMM (2020) The microbiome and inflammatory bowel disease. J Allergy Clin Immunol 145(1):16–27. https://doi.org/10.1016/j.jaci.2019.11.003
Abraham BP, Quigley EMM (2017) Probiotics in inflammatory bowel disease. Gastroenterol Clin N Am 46(4):769–782. https://doi.org/10.1016/j.gtc.2017.08.003
Celiberto LS, Pinto RA, Rossi EA, Vallance BA, Cavallini DCU (2018) Isolation and characterization of potentially probiotic bacterial strains from mice: proof of concept for personalized probiotics. Nutrients. https://doi.org/10.3390/nu10111684
Acknowledgements
This research was financially supported by the National Natural Science Foundation of China (31372453) and Henan Institute of Science and Technology (152102310260). The assistance of the staff is gratefully acknowledged.
Funding
This research was financially supported by the National Natural Science Foundation of China (31372453) and Henan Institute of Science and Technology (152102310260).
Author information
Authors and Affiliations
Contributions
XFZ and XXG participated in the study design. XFZ, XXG, YJT and JFS searched the literature and selected studies. XKW and WDW extracted data and assessed quality. XFZ and XXG drafted the manuscript. JMF revised the draft and all authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do have not any conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
For this type of study, formal consent is not required.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, XF., Guan, XX., Tang, YJ. et al. Clinical effects and gut microbiota changes of using probiotics, prebiotics or synbiotics in inflammatory bowel disease: a systematic review and meta-analysis. Eur J Nutr 60, 2855–2875 (2021). https://doi.org/10.1007/s00394-021-02503-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02503-5