Abstract
Purpose
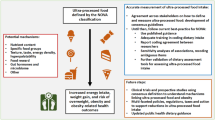
Breast cancer (BC) incidence is increasing worldwide. Higher insulin resistance may potentially lead to an increased risk of BC. Sugar-sweetened beverages (SSB) are an acknowledged dietary factor that increases insulin resistance. However, the association between SSB and BC has not been widely explored. We evaluated the association between baseline consumption of SSB and the incidence of BC among relatively young women in a cohort of Spanish university graduates.
Methods
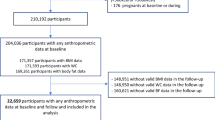
We evaluated 10,713 middle-aged, Spanish female university graduates (median age 33) from the Seguimiento Universidad de Navarra (SUN) cohort, initially free of BC. SSB consumption was collected at baseline using a validated 136-item semi-quantitative food-frequency questionnaire. Incidence of BC was confirmed by a trained oncologist using medical records. We fitted Cox regression models to assess the relationship between baseline categories of SSB consumption and the incidence of BC during follow-up. We stratified the analyses by menopausal status.
Results
During 106,189 person-years follow-up, 100 incident cases of BC were confirmed. Among postmenopausal women, regular consumption of SSB was associated with a significantly higher incidence of BC (HR 2.12; 95% CI 1.02, 4.41) in the fully adjusted model, compared to women who never or seldom consumed SSB. No association was found among premenopausal women (HR 1.16; 95% CI 0.66, 2.07).
Conclusions
Even though the number of cases was small, in this Mediterranean cohort, we observed a direct association between SSB consumption and BC risk among postmenopausal women. Nonetheless further larger longitudinal studies are needed to support this association.


Similar content being viewed by others
Abbreviations
- BC:
-
Breast cancer
- SSB:
-
Sugar-sweetened beverage
- SUN:
-
Seguimiento Universidad de Navarra (University of Navarra Follow-up Study)
- HR:
-
Hazard ratio
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- BMI:
-
Body mass index
- MET:
-
Metabolic equivalent index
- SD:
-
Standard deviation
References
World Health Organization (2012) GLOBOCAN. Cancer fact sheets: breast cancer. http://globocan.iarc.fr/old/FactSheets/cancers/breast-new.asp. Accessed 6 Jun 2018
World Cancer Research Fund, American Institute for Cancer Research (2017) Diet, nutrition, physical activity and breast cancer. http://www.aicr.org/continuous-update-project/reports/breast-cancer-report-2017.pdf. Accessed 6 Jun 2018
Global Burden of Disease Cancer Collaboration C, Fitzmaurice C, Allen C et al (2017) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 3:524–548. https://doi.org/10.1001/jamaoncol.2016.5688
Ligibel JA, Alfano CM, Courneya KS, Demark-Wahnefried W, Burger RA, Chlebowski RT et al (2014) American Society of Clinical Oncology position statement on obesity and cancer. J Clin Oncol 32:3568–3574. https://doi.org/10.1200/JCO.2014.58.4680
Mørch LS, Skovlund CW, Hannaford PC et al (2017) Contemporary hormonal contraception and the risk of breast cancer. N Engl J Med 377:2228–2239. https://doi.org/10.1056/NEJMoa1700732
Gartlehner G, Patel SV, Feltner C et al (2017) Hormone therapy for the primary prevention of chronic conditions in postmenopausal women: evidence report and systematic review for the US preventive services task force. JAMA 318:2234–2249. https://doi.org/10.1001/jama.2017.16952
Kobayashi S, Sugiura H, Ando Y, Shiraki N, Yanagi T, Yamashita H et al (2012) Reproductive history and breast cancer risk. Breast Cancer 19:302–308. https://doi.org/10.1007/s12282-012-0384-8
Collaborative Group on Hormonal Factors in Breast Cancer (2002) Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet 360:187–195
Petri AL, Tjønneland A, Gamborg M et al (2004) Alcohol intake, type of beverage, and risk of breast cancer in pre- and postmenopausal women. Alcohol Clin Exp Res 28:1084–1090
Romieu I, Scoccianti C, Chajès V et al (2015) Alcohol intake and breast cancer in the European prospective investigation into cancer and nutrition. Int J Cancer 137:1921–1930. https://doi.org/10.1002/ijc.29469
Smith-Warner SA, Spiegelman D, Yaun SS et al (1998) Alcohol and breast cancer in women: a pooled analysis of cohort studies. JAMA 279:535–540
Fortner RT, Katzke V, Kúhn T et al (2016) Obesity and breast cancer. Recent Results Cancer Res 208:43–65
Lahmann PH, Friedenreich C, Schuit AJ et al (2007) Physical activity and breast cancer risk: the european prospective investigation into cancer and nutrition. Cancer Epidemiol Biomark Prev 16:36–42
Wu Y, Zhang D, Kang S (2013) Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat 137:869–882. https://doi.org/10.1007/s10549-012-2396-7
Doll R, Peto R (1981) The causes of cancer: quantitative estimates of avoidable risks of cancer in the united states today. J Natl Cancer Inst 66:1192–1308
World Cancer Research Fund/American Institute for Cancer Research. Diet, nutrition, physical activity and cancer: a global perspective. Continuous update project expert report 2018. Available at https://www.wcrf.org/dietandcancer. Accessed 6 June 2018
Eccles S, Aboagye EO, Ali S, Anderson a S, Armes J, Berditchevski F et al (2013) Critical research gaps and translational priorities for the successful prevention and treatment of breast cancer. Breast Cancer Res 15:92. https://doi.org/10.1186/bcr3493
Hodge AM, Bassett JK, Milne RL, English DR, Giles GG (2018) Consumption of sugar-sweetened and artificially sweetened soft drinks and risk of obesity-related cancers. Public Health Nutr 21:1618–1626
Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB (2010) Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 33:2477–2481. https://doi.org/10.2337/dc10-1079
Hu FB, Malik VS (2010) Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav 100:47–54. https://doi.org/10.1016/j.physbeh.2010.01.036
Barrio-Lopez MT, Martinez-Gonzalez M, Fernandez-Montero A, Beunza JJ, Zazpe I, Bes-Rastrollo M (2013) Prospective study of changes in sugar-sweetened beverage consumption and the incidence of the metabolic syndrome and its components: the SUN cohort. Br J Nutr 110:1722–1731. https://doi.org/10.1017/S0007114513000822
Carwile JL, Willett WC, Spiegelman D, Hertzmark E, Rich-Edwards J, Frazier a L et al (2015) Sugar-sweetened beverage consumption and age at menarche in a prospective study of US girls. Hum Reprod 30:675–683. https://doi.org/10.1093/humrep/deu349
Duchaine CS, Dumas I, Diorio C (2014) Consumption of sweet foods and mammographic breast density: a cross-sectional study. BMC Public Health 14:554. https://doi.org/10.1186/1471-2458-14-554
Seguí-Gómez M, de la Fuente C, Vázquez Z, de Irala J, Martínez-González MA (2006) Cohort profile: the “Seguimiento Universidad de Navarra” (SUN) study. Int J Epidemiol 35:1417–1422. https://doi.org/10.1186/1475-2891-10-121
Willett WC (2013) Issues in analysis and presentation of dietary data. In: Willett WC (ed) Nutritional epidemiology, 3rd edn. Oxford University Press, New York, pp 305–333
Martin-Moreno JM, Boyle P, Gorgojo L et al (1993) Development and validation of a food frequency questionnaire in Spain. Int J Epidemiol 22:512–519
De la Fuente-Arrillaga C, Vázquez Ruiz Z, Bes-Rastrollo M, Sampson L, Martinez-González MA (2010) Reproducibility of an FFQ validated in Spain. Public Health Nutr 13:1364–1372. https://doi.org/10.1017/S1368980009993065
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348:2599–2608
Bes-Rastrollo M, Pérez Valdivieso JR, Sánchez-Villegas A, Alonso Á, Martínez-González M (2005) Validación del peso e índice de masa corporal auto-declarados de los participantes de una cohorte de graduados universitarios. Rev Esp Obes 3:352–358. https://doi.org/10.3305/nh.2013.28.5.6671
Martínez-González MA, López-Fontana C, Varo JJ et al (2005) Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr 8:920–927
Shivappa N, Sandin S, Löf M et al (2015) Prospective study of dietary inflammatory index and risk of breast cancer in Swedish women. Br J Cancer 113:1099–1103. https://doi.org/10.1038/bjc.2015.304
Augustin LS, Dal Maso L, La Vecchia C, Parpinel M, Negri E, Vaccarella S et al (2001) Dietary glycemic index and glycemic load, and breast cancer risk: a case–control study. Ann Oncol 12:1533–1538
Potischman N, Coates RJ, Swanson CA, Carroll RJ, Daling JR, Brogan DR et al (2002) Increased risk of early-stage breast cancer related to consumption of sweet foods among women less than age 45 in the United States. Cancer Causes Control 13:937–946. https://doi.org/10.1023/A:1021919416101
Bradshaw PT, Sagiv SK, Kabat GC, Satia JA, Britton JA, Teitelbaum SL et al (2009) Consumption of sweet foods and breast cancer risk: a case–control study of women on Long Island, New York. Cancer Causes Control 20:1509–1515. https://doi.org/10.1007/s10552-009-9343-x
Chandran U, McCann SE, Zirpoli G, Gong Z, Lin Y, Hong CC et al (2014) Intake of energy-dense foods, fast foods, sugary drinks, and breast cancer risk in African American and European American women. Nutr Cancer 66:1187–1199. https://doi.org/10.1080/01635581
Witte JS, Ursin G, Siemiatycki J, Thompson WD, Paganini-Hill A, Haile RW (1997) Diet and premenopausal bilateral breast cancer: a case–control study. Breast Cancer Res Treat 42:243–251. https://doi.org/10.1023/A:1005710211184
Monzavi-Karbassi B, Hine RJ, Stanley JS, Ramani VP, Carcel-Trullols J, Whitehead TL et al (2010) Fructose as a carbon source induces an aggressive phenotype in MDA-MB-468 breast tumor cells. Int J Oncol 37:615–622
Liu H, Heaney AP (2011) Refined fructose and cancer. Expert Opin Ther Targets 15:1049–1059. https://doi.org/10.1517/14728222.2011
Ludwig DS (2003) Diet and development of the insulin resistance syndrome. Asia Pac J Clin Nutr 12:4
Kaaks R (1996) Nutrition, hormones, and breast cancer: is insulin the missing link? Cancer Causes Control 7:605–625
Kaaks R (2001) Plasma insulin, IGF-I and breast cancer. Gynecol Obstet Fertil 29:185–191. https://doi.org/10.1016/S1297-9589(00)00047-3
Christopoulos PF, Msaouel P, Koutsilieris M (2015) The role of the insulin-like growth factor-1 system in breast cancer. Mol Cancer 14:43. https://doi.org/10.1186/s12943-015-0291-7
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE, Manson JE et al (2009) Insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 101:48–60. https://doi.org/10.1093/jnci/djn415
Iyengar NM, Hudis CA, Dannenberg AJ (2015) Obesity and cancer: local and systemic mechanisms. Annu Rev Med 66:297–309. https://doi.org/10.1146/annurev-med-050913-022228
Bhandari R, Kelley G, Hartley T, Rockett I (2014) Metabolic syndrome is associated with increased breast cancer risk: a systematic review with meta-analysis. Int J Breast Cancer 2014:1–13. https://doi.org/10.1155/2014/189384
Shapira N (2017) The potential contribution of dietary factors to breast cancer prevention. Eur J Cancer Prev 26:385–395. https://doi.org/10.1097/CEJ.0000000000000406
Fernández-Ballart JD, Piñol JL, Zazpe I, Corella D, Carrasco P, Toledo E et al (2010) Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr 103:1808–1816. https://doi.org/10.1017/S0007114509993837
U.S. Department of Health and Human Services and U.S. Department of Agriculture (2015) 2015–2020 dietary guidelines for Americans, 8th edn. https://health.gov/dietaryguidelines/2015/guidelines/. Accessed 6 Jun 2018
Acknowledgements
The authors thank the implication and collaboration of the participants in the SUN Project. ARN was supported by the Fundación Científica Asociación Española Contra el Cáncer (AECC) (Scientific Foundation of the Spanish Association Against Cancer). We thank the other members of the SUN Group: Alonso A, Barrio López MT, Basterra-Gortari FJ, Benito Corchón S, Bes-Rastrollo M, Beunza JJ, Carlos Chillerón S, Carmona L, Cervantes S, de Irala Estévez J, de la Fuente Arrillaga C, de la Rosa PA, Delgado Rodríguez M, Dominguz LJ, Donat Vargas CL, Donázar M, Eguaras S, Fernández Montero A, Galbete Ciáurriz C, García López M, Goñi Ochandorena E, Guillén Grima F, Hernández-Hernandez A, Llorca J, López del Burgo C, Marí Sanchís A, Martí del Moral A, Martín Calvo N, Martínez JA, Molero P, Núñez-Córdoba JM, Pimenta AM, Rico A, Ruiz-Canela M, Ruiz Zambrana A, Sánchez Adán D, Sayón Orea C, Vázquez Ruiz Z. All authors revised the manuscript and read and approved the final version of it.
Funding
The SUN Project has received funding from the Spanish Government-Instituto de Salud Carlos III, and the European Regional Development Fund (FEDER) (RD 06/0045, CIBER-OBN, Grants PI10/02658, PI10/02293, PI13/00615, PI14/01668, PI14/01798, PI14/01764, PI17/01795, and G03/140), the Navarra Regional Government (45/2011, 122/2014, 41/2016), and the University of Navarra.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving participants were approved by the Institutional Review Board of the University of Navarra. All potential participants were duly informed of their right to refuse to participate in the SUN study or to withdraw their consent to participate at any time without reprisal. Special attention was given to the specific information needs of individual potential candidates as well as to the methods used to deliver their information and the feedback that may receive in the future from the research team. After ensuring that the candidate had understood the information, we sought their potential freely given informed consent through their voluntary completion of the baseline questionnaire. These methods were accepted by our Institutional Review Board as to imply an appropriately-obtained informed consent.
Conflict of interest
On behalf of all authors, the corresponding author declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Romanos-Nanclares, A., Toledo, E., Gardeazabal, I. et al. Sugar-sweetened beverage consumption and incidence of breast cancer: the Seguimiento Universidad de Navarra (SUN) Project. Eur J Nutr 58, 2875–2886 (2019). https://doi.org/10.1007/s00394-018-1839-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1839-2