Abstract
Background
Functional gastrointestinal symptoms such as abdominal pain, bloating, distension, constipation, diarrhea and flatulence have been noted in patients with irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD). The diversity of symptoms has meant that finding an effective treatment has been challenging with most treatments alleviating only the primary symptom. A novel treatment option for IBS and IBD currently generating much excitement is the low fermentable, oligo-, di-, mono-saccharides and polyol (FODMAP) diet. The aim of this meta-analysis was to determine the evidence of the efficacy of such a diet in the treatment of functional gastrointestinal symptoms.
Methods
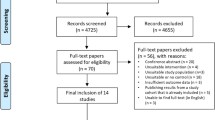
Electronic databases were searched through to March 2015 to identify relevant studies. Pooled odds ratios (ORs) and 95 % confidence intervals were calculated for the effect of a low FODMAP diet on the reduction in IBS [Symptoms Severity Score (SSS)] score and increase in IBS quality of life (QOL) score for both randomized clinical trials (RCTs) and non-randomized interventions using a random-effects model.
Results
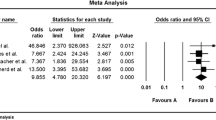
Six RCTs and 16 non-randomized interventions were included in the analysis. There was a significant decrease in IBS SSS scores for those individuals on a low FODMAP diet in both the RCTs (OR 0.44, 95 % CI 0.25–0.76; I 2 = 35.52, p = 0.00) and non-randomized interventions (OR 0.03, 95 % CI 0.01–0.2; I 2 = 69.1, p = 0.02). In addition, there was a significant improvement in the IBS-QOL score for RCTs (OR 1.84, 95 % CI 1.12–3.03; I 2 = 0.00, p = 0.39) and for non-randomized interventions (OR 3.18, 95 % CI 1.60–6.31; I 2 = 0.00, p = 0.89). Further, following a low FODMAP diet was found to significantly reduce symptom severity for abdominal pain (OR 1.81, 95 % CI 1.13–2.88; I 2 = 0.00, p = 0.56), bloating (OR 1.75, 95 % CI 1.07–2.87; I 2 = 0.00, p = 0.45) and overall symptoms (OR 1.81, 95 % CI 1.11–2.95; I 2 = 0.00, p = 0.4) in the RCTs. In the non-randomized interventions similar findings were observed.
Conclusion
The present meta-analysis supports the efficacy of a low FODMAP diet in the treatment of functional gastrointestinal symptoms. Further research should ensure studies include dietary adherence, and more studies looking at greater number of patients and long-term adherence to a low FODMAP diet need to be conducted.





Similar content being viewed by others
References
Russo MW, Gaynes BN, Drossman DA (1999) A national survey of practice patterns of gastroenterologists with comparison to the past two decades. J Clin Gastroenterol 29(339):43
Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, Talley NJ, Quigley EM (2009) An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol 104:S1–S35
Andrews EB, Eaton SC, Hollis KA, Hopkins JS, Ameen V, Hamm LR et al (2005) Prevalence and demographics of irritable bowel syndrome: results from a large web-based survey. Aliment Pharmacol Ther 22(10):935–942
Horwitz BJ, Fisher RS (2001) The irritable bowel syndrome. N Engl J Med 344:1846–1850
Anastasi JK, Capili B, Chang M (2013) Managing irritable bowel syndrome. AJN Am J Nurs 113(7):42–52
Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, Talley NJ, Quigley EM (2009) American college of gastroenterology task force on irritable bowel syndrome—an evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol 104(Suppl 1):S1–S35
Eswaran S, Muir J, Chey WD (2013) Fiber and functional gastrointestinal disorders. Am J Gastroenterol 108:718–727
Eswaran S, Tack J, Chey WD (2011) Food: the forgotten factor in the irritable bowel syndrome. Gastroenterol Clin N Am 40(1):141–162
Shepherd SJ, Halmos E, Glance S (2014) The role of FODMAPs in irritable bowel syndrome. Curr Opin Clin Nutr Metab Care 17(6):605–609
Gibson PR, Shepherd SJ (2005) Personal view: food for thought–western lifestyle and susceptibility to Crohn’s disease—the FODMAP hypothesis. Aliment Pharmacol Ther 21(12):1399–1409
Parker K, Salas M, Nwosu VC (2010) High fructose corn syrup: production, uses and public health concerns. Biotechnol Mol Biol Rev 5(5):71–78
Barrett JS, Gearry RB, Muir JG, Irving PM, Rose R, Rosella O, Haines ML, Shepherd SJ, Gibson PR (2010) Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther 31(8):874
Ong DK, Mitchell SB, Barrett JS, Shepherd SJ, Irving PM, Biesiekierski JR et al (2010) Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol 25(8):1366
Halmos E, Chrstopherrsen CT, Bird AR, Shepard SJ, Gibson PR, Muir JG (2015) Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut 64(1):93–100
Huamán JW, Felip A, Guedea E, Jansana M, Videla S, Saperas E (2014) The diet low in fermentable carbohydrates short chain and polyols improves symptoms in patients with functional gastrointestinal disorders in Spain. Gastroenterol Hepatol 6(14):00245
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ Br Med J 327(7414):557–560
Egger M, Davey S, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 1(315):629–634
Orwin R (1983) A fail-safe N for effect size in meta-analysis. J Educ Stat 8:157–159
Staudacher HM, Lomer MCE, Anderson JL, Barrett JS, Muir JG, Irving PM, Whelan K (2012) Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr 142(8):1510
Pedersen N, Ankersen DV, Felding M, Vegh Z, Burisch J, Munkholm P (2014) Mo1210 low FODMAP diet reduces irritable bowel symptoms and improves quality of life in patients with inflammatory bowel disease in a randomized controlled trial. Gastroenterology 146(5):S-587
Pedersen N, Andersen NN, Végh Z, Jensen L, Ankersen DV, Felding M, Simonsen M, Burisch J, Munkholm (2014) Ehealth: low FODMAP diet vs Lactobacillus rhamnosus GG in irritable bowel syndrome. World J Gastroenterol WJG 20(43):16215
Harvie R, Schultz M, Chisholm A (2013) A reduction in FODMAP intake correlates strongly with a reduction in IBS symptoms–the FIBS study. J Gastroenterol Hepatol 28(Suppl. 3):23–693
Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG (2013) A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology 146(1):67
Staudacher HM, Whelan K, Irving PM, Lomer MCE (2011) Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet 24(5):487–495
Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, Gibson PR (2013) No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 145(2):320
Chumpitazi BP, Tsai CM, McMeans AR, Shulman RJ (2014) A low fodmaps diet ameliorates symptoms in children with irritable bowel syndrome: a double blind, randomized crossover trial. Gastroenterology 146(5):S-144
Pedersen N, Vegh Z, Burisch J, Jensen L, Ankersen DV, Felding M, Simonsen M, Burisch J, Munkholm P (2014) Ehealth monitoring in irritable bowel syndrome patients treated with low fermentable oligo-, di-, mono-saccharides and polyols diet. World J Gastroenterol 20(21):6680–6684
Roest RH, Dobbs BR, Chapman BA, Batman B, O’Brien LA, Leeper JA, Hebblethwaite CR, Gearry RB (2013) The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study. Int J Clin Pract 67(9):895–903
Zubek J, White R (2012) An audit investigating the efficacy of the low FODMAP diet in improving symptoms in patients with functional gastro-intestinal symptoms. Gut 61:A86–A86
Mcgeoch V, Blackwell V, Wigham L, Hoare JM (2014) PWE-170: an audit of clinical response in patients with Ibs treated with the low Fodmap diet at St Mary’s Hospital. Gut 63(Supp 1):A199–A200
O’Meara C, Craig OF, Mahmud N, McKiernan S, Maccarthy F (2013) A pilot study on the introduction of a low FODMAP diet in a subgroup of symptomatic IBS patients referred by the gastroenterology service in an Irish Tertiary Referral Centre. Gut 62(Suppl 2):A3–A4
Ones M, Morken MH, Hatlebakk JG (2014) PP112-MON: effects of a Fodmap-restricted diet in a Scandinavian population with irritable bowel syndrome. Clin Nutr 33:S171
Van Megen F, Kahrs GE (2014) Effects of a FODMAP-restricted diet on irritable bowel symptoms in patients with inflammatory bowel disease. United Eur Gastroenterol J 2(Suppl 1):P0342
Chevillat D, Neff S, Maghdessian R, Kiss C, Maissen S (2014) P091: L’approche FODMAP améliore la symptomatologie gastro-intestinale chez les patients adultes souffrant d’un syndrome de l’intestin irritable: une étude pilote. Nutrition Clinique et Métabolisme. UEG Week 28: S116
Zanini B, Marullo M, Ricci C, Lanzarotto F, Lanzini A (2014) Sa1989 non celiac gluten sensitivity (NCGS) is outnumbered by FODMAPs sensitivity in patients spontaneously adhering to gluten free diet (GFD): a two stage double blind prospective study. Gastroenterology 146(5):S-348
Joyce T, Staudacher H, Whelan K, Irving P, Lomer M (2014) PWE-092 symptom response following advice on a diet low in short-chain fermentable carbohydrates (fodmaps) for functional bowel symptoms in patients with Ibd. Gut 63(Suppl 1):A164
Mazzawi T, Hausken T, Gundersen D, El-Salhy M (2013) Effects of dietary guidance on the symptoms, quality of life and habitual dietary intake of patients with irritable bowel syndrome. Mol Med Rep 8(3):845–852
Gearry RB, Irving PM, Barrett JS, Nathan DM, Shepherd SJ, Gibson PR (2009) Reduction of dietary poorly absorbed short-chain carbohydrates (FODMAPs) improves abdominal symptoms in patients with inflammatory bowel disease—a pilot study. J Crohn’s Colitis 3(1):8–14
Azpiroz F, Guyonnet D, Donazzolo Y, Gendre D, Tanguy J, Guarner F (2014) Digestive symptoms in healthy people and subjects with irritable bowel syndrome: validation of symptom frequency questionnaire. J Clin Gastroenterol 1
Francis CY, Morris J, Whorwell PJ (1997) The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 11(2):395–402
Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL (1998) Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci 43(2):400
Drossman D, Morris CB, Hu Y, Toner BB, Diamant N, Whitehead WE et al (2007) Characterization of health related quality of life (HRQOL) for patients with functional bowel disorder (FBD) and its response to treatment. Am J Gastroenterol 102(7):1442–1453
Christodoulides S (2014) PWE-184 the effect of fibre on chronic constipation in adults: a systematic review. Gut 63(suppl 1):A206–A207
James SL et al (2009) FODMAP but not fibre intake is associated with IBS-like symptoms in patients with IBD. J Gastroenterol Hepatol 24:A313–A314
Rome F (2006) Guidelines-Rome III diagnostic criteria for functional gastrointestinal disorders. J Gastrointest Liver Dis 15(3):307–312
Buono JL, Tourkodimitris S, Sarocco P, Johnston JM, Carson RT (2014) Impact of linaclotide treatment on work productivity and activity impairment in adults with irritable bowel syndrome with constipation: results from 2 randomized, double-blind, placebo-controlled phase 3 trials. Am Health Drug Benefits 7(5):289
Muir JG, Rose R, Rosella O, Liels K, Barrett JS, Shepherd SJ et al (2009) Measurement of short-chain carbohydrates in common australian vegetables and fruits by high-performance liquid chromatography (HPLC). J Agric Food Chem 57(2):554–565
Staudacher HM, Lomer MCE, Anderson JL, Barrett JS, Muir JG, Irving PM et al (2010) Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr 142(8):1510
Tuck CJ (2014) Fermentable oligosaccharides, disaccharides, monosaccharides and polyols: role in irritable bowel syndrome. Expert Rev Gastroenterol Hepatol 8(7):819–834
Azpiroz F, Malagelada J (2005) Abdominal bloating. Gastroenterology 129(3):1060–1078
Spiegel BMR, Bolus R, Harris LA, Lucak S, Chey WD, Sayuk G et al (2010) Characterizing abdominal pain in IBS: guidance for study inclusion criteria, outcome measurement and clinical practice. Aliment Pharmacol Ther 32(9):1192
Houghton LA, Lea R, Agrawal A, Agrawal A, Reilly B, Whorwell PJ (2006) Relationship of abdominal bloating to distention in irritable bowel syndrome and effect of bowel habit. Gastroenterology 131(4):1003
Böhn L, Störsrud S, LiIjebo T, Collin L, Törnblom H, Simrén M (2014) A Multi-center, randomized, controlled, single-blind, comparative trial: low-FODMAP diet versus traditional dietary advice in IBS. United Eur Gastroenterol J 2(1S):A1–A131
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marsh, A., Eslick, E.M. & Eslick, G.D. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr 55, 897–906 (2016). https://doi.org/10.1007/s00394-015-0922-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-0922-1