Abstract
Purpose
Although previous literature has reported that regular green tea consumption may improve blood pressure, the evidence from these studies is not consistent. The present study systematically reviewed randomised controlled trials and examined the effect of green tea consumption on blood pressure using meta-analysis.
Methods
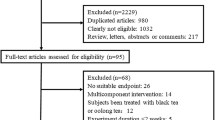
Search of ProQuest, PubMed, Scopus and Cochrane Library (CENTERAL) was conducted, to identify eligible articles. Articles from 1995 to 2013 were included. A random-effect model was chosen to calculate the effect of combined trials.
Result
Thirteen studies were included in the meta-analysis. Green tea consumption significantly changed systolic blood pressure, by −2.08 mm Hg (95 % CI −3.06, −1.05), and diastolic blood pressure, by −1.71 mm Hg (95 % CI −2.86, −0.56), compared to the control. Changes in lipid profile, blood glucose and body mass index were also assessed in the meta-analysis. A significant reduction was found in total cholesterol (−0.15 mmol/L [95 % CI −0.27, −0.02]) and low-density lipoprotein cholesterol (−0.16 mmol/L [95 % CI −0.22, −0.09]). Changes in other parameters did not reach statistical significance. Subgroup analysis suggested a greater reduction in both systolic and diastolic blood pressure in studies that included participants with a baseline mean systolic blood pressure of ≥130 mm Hg, and studies involving consuming green tea as an extract.
Conclusion
The present meta-analysis suggests that green tea and its catechins may improve blood pressure, and the effect may be greater in those with systolic blood pressure ≥130 mm Hg. The meta-analysis also suggests that green tea catechins may improve total and low-density lipoprotein cholesterol.



Similar content being viewed by others
References
WHO (2002) World Health Organization. World Health Report 2002. Reducing risks, promoting healthy life. Geneva, Switzerland. http://wwww.hoint/whr/2002/en
WHO (2008) Global health observatory (GHO). Raised blood pressure. http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/index.html
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS (2012) Heart disease and stroke statistics—2012 update a report from the American Heart Association. Circulation 125(1):e2–e220
Law M, Wald N, Morris J (2005) Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy. Int J Technol Assess Health Care 21(1):145. doi:10.1017/s0266462305220196
Qureshi A, Sapkota B (2011) Blood pressure reduction in secondary stroke prevention. Continuum (Minneapolis, Minn) 17 (6 2ndary Stroke Prevention):1233
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT (2003) Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42(6):1206–1252
Hooper L, Kroon PA, Rimm EB, Cohn JS, Harvey I, Le Cornu KA, Ryder JJ, Hall WL, Cassidy A (2008) Flavonoids, flavonoid-rich foods, and cardiovascular risk: a meta-analysis of randomized controlled trials. Am J Clin Nutr 88(1):38–50
Rains TM, Agarwal S, Maki KC (2011) Antiobesity effects of green tea catechins: a mechanistic review. J Nutr Biochem 22(1):1–7
Balentine DA, Wiseman SA, Bouwens LC (1997) The chemistry of tea flavonoids. Crit Rev Food Sci Nutr 37(8):693–704
Bhardwaj P, Khanna D (2013) Green tea catechins: defensive role in cardiovascular disorders. Chin J Nat Med 11(4):345–353
Erba D, Riso P, Bordoni A, Foti P, Biagi PL, Testolin G (2005) Effectiveness of moderate green tea consumption on antioxidative status and plasma lipid profile in humans. J Nutr Biochem 16(3):144–149. doi:10.1016/j.jnutbio.2004.11.006
Maruyama K, Iso H, Sasaki S, Fukino Y (2009) The association between concentrations of green tea and blood glucose levels. J Clin Biochem Nutr 44(1):41
Mu LN, Lu QY, Yu SZ, Jiang QW, Cao W, You NC, Setiawan VW, Zhou XF, Ding BG, Wang RH (2005) Green tea drinking and multigenetic index on the risk of stomach cancer in a Chinese population. Int J Cancer 116(6):972–983
Sun C-L, Yuan J-M, Koh W-P, Mimi CY (2006) Green tea, black tea and breast cancer risk: a meta-analysis of epidemiological studies. Carcinogenesis 27(7):1310–1315
Antonello M, Montemurro D, Bolognesi M, Di Pascoli M, Piva A, Grego F, Sticchi D, Giuliani L, Garbisa S, Rossi GP (2007) Prevention of hypertension, cardiovascular damage and endothelial dysfunction with green tea extracts. Am J Hypertens 20(12):1321–1328
Nagao T, Hase T, Tokimitsu I (2007) A green tea extract high in catechins reduces body fat and cardiovascular risks in humans. Obesity 15(6):1473–1483. doi:10.1038/oby.2007.176
Auvichayapat P, Prapochanung M, Tunkamnerdthai O, Sripanidkulchai B-O, Auvichayapat N, Thinkhamrop B, Kunhasura S, Wongpratoom S, Sinawat S, Hongprapas P (2008) Effectiveness of green tea on weight reduction in obese Thais: a randomized, controlled trial. Physiol Behav 93(3):486–491
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269
Liberati A, Moher D, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. doi:10.1371/journal.pmed.1000100
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Commun Health 52(6):377–384
Cohen J (1992) A power primer. Psychol Bull 112(1):155–159. doi:10.1037/0033-2909.112.1.155
Harrison RA, Siminoski K, Vethanayagam D, Majumdar SR (2007) Osteoporosis-related kyphosis and impairments in pulmonary function: a systematic review. J Bone Miner Res 22(3):447–457
Higgins J, Green SP, Wiley I, Cochrane C (2008) Cochrane handbook for systematic reviews of interventions. vol Book, Whole. Wiley-Blackwell, Hoboken
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, Medical Research Council, UK
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188. doi:10.1016/0197-2456(86)90046-2
Kim A, Chiu A, Barone MK, Avino D, Wang F, Coleman CI, Phung OJ (2011) Green tea catechins decrease total and low-density lipoprotein cholesterol: a systematic review and meta-analysis. J Am Diet Assoc 111(11):1720–1729
Dong J-Y, Szeto IM, Makinen K, Gao Q, Wang J, Qin L-Q, Zhao Y (2013) Effect of probiotic fermented milk on blood pressure: a meta-analysis of randomised controlled trials. Br J Nutr 110(07):1188–1194
Sone T, Kuriyama S, Nakaya N, Hozawa A, Shimazu T, Nomura K, Rikimaru S, Tsuji I (2011) Randomized controlled trial for an effect of catechin-enriched green tea consumption on adiponectin and cardiovascular disease risk factors. Food Nutr Res 55:1–10. doi:10.3402/fnr.v55i0.8326
Basu A, Du M, Sanchez K, Leyva MJ, Betts NM, Blevins S, Wu M, Aston CE, Lyons TJ (2011) Green tea minimally affects biomarkers of inflammation in obese subjects with metabolic syndrome. Nutrition 27(2):206–213. doi:10.1016/j.nut.2010.01.015
Fukino Y, Shimbo M, Aoki N, Okubo T, Iso H (2005) Randomized controlled trial for an effect of green tea consumption on insulin resistance and inflammation markers. J Nutr Sci Vitaminol (Tokyo) 51(5):335–342
Bogdanski P, Suliburska J, Szulinska M, Stepien M, Pupek-Musialik D, Jablecka A (2012) Green tea extract reduces blood pressure, inflammatory biomarkers, and oxidative stress and improves parameters associated with insulin resistance in obese, hypertensive patients. Nutr Res 32(6):421–427. doi:10.1016/j.nutres.2012.05.007
Frank J, George TW, Lodge JK, Rodriguez-Mateos AM, Spencer JP, Minihane AM, Rimbach G (2009) Daily consumption of an aqueous green tea extract supplement does not impair liver function or alter cardiovascular disease risk biomarkers in healthy men. J Nutr 139(1):58–62. doi:10.3945/jn.108.096412
Hsu CH, Liao YL, Lin SC, Tsai TH, Huang CJ, Chou P (2011) Does supplementation with green tea extract improve insulin resistance in obese type 2 diabetics? A randomized, double-blind, and placebo-controlled clinical trial. Altern Med Rev 16(2):157–163
Hsu CH, Tsai TH, Kao YH, Hwang KC, Tseng TY, Chou P (2008) Effect of green tea extract on obese women: a randomized, double-blind, placebo-controlled clinical trial. Clin Nutr 27(3):363–370
Nagao T, Hase T, Tokimitsu I (2007) A green tea extract high in catechins reduces body fat and cardiovascular risks in humans. Obesity (Silver Spring) 15(6):1473–1483. doi:10.1038/oby.2007.176
Nantz MP, Rowe CA, Bukowski JF, Percival SS (2009) Standardized capsule of Camellia sinensis lowers cardiovascular risk factors in a randomized, double-blind, placebo-controlled study. Nutrition 25(2):147–154
Suliburska J, Bogdanski P, Szulinska M, Stepien M, Pupek-Musialik D, Jablecka A (2012) Effects of green tea supplementation on elements, total antioxidants, lipids, and glucose values in the serum of obese patients. Biol Trace Elem Res 149(3):315–322. doi:10.1007/s12011-012-9448-z
Vieira Senger AE, Schwanke CHA, Gomes I, Valle Gottlieb MG (2012) Effect of green tea (Camellia sinensis) consumption on the components of metabolic syndrome in elderly. J Nutr Health Aging 16(9):738–742. doi:10.1007/s12603-012-0081-5
Diepvens K, Kovacs EM, Nijs IM, Vogels N, Westerterp-Plantenga MS (2005) Effect of green tea on resting energy expenditure and substrate oxidation during weight loss in overweight females. Br J Nutr 94(6):1026–1034
Chantre P, Lairon D (2002) Recent findings of green tea extract AR25 (exolise) and its activity for the treatment of obesity. Phytomedicine 9(1):3–8
Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH (1995) Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med 155(7):701–709. doi:10.1001/archinte.1995.00430070053006
Islam MA (2012) Cardiovascular effects of green tea catechins: progress and promise. Recent Pat Cardiovasc Drug Discov 7(2):88–99
Rastaldo R, Pagliaro P, Cappello S, Penna C, Mancardi D, Westerhof N, Losano G (2007) Nitric oxide and cardiac function. Life Sci 81(10):779–793
Gössl M, Lerman A (2006) Endothelin beyond a vasoconstrictor. Circulation 113(9):1156–1158
Collins QF, Liu H-Y, Pi J, Liu Z, Quon MJ, Cao W (2007) Epigallocatechin-3-gallate (EGCG), a green tea polyphenol, suppresses hepatic gluconeogenesis through 5′-AMP-activated protein kinase. J Biol Chem 282(41):30143–30149
Pon Anandh B, Dongmin L (2008) Green tea catechins and cardiovascular health: an update. Curr Med Chem 15(18):1840–1850. doi:10.2174/092986708785132979
Maron DJ, Lu GP, Cai NS, Wu ZG, Li YH, Chen H, Zhu JQ, Jin XJ, Wouters BC, Zhao J (2003) Cholesterol-lowering effect of a theaflavin-enriched green tea extract: a randomized controlled trial. Arch Intern Med 163(12):1448–1453
Koo SI, Noh SK (2007) Green tea as inhibitor of the intestinal absorption of lipids: potential mechanism for its lipid-lowering effect. J Nutr Biochem 18(3):179–183
Bursill CA, Abbey M, Roach PD (2007) A green tea extract lowers plasma cholesterol by inhibiting cholesterol synthesis and upregulating the LDL receptor in the cholesterol-fed rabbit. Atherosclerosis 193(1):86–93
Ikeda I, Kobayashi M, Hamada T, Tsuda K, Goto H, Imaizumi K, Nozawa A, Sugimoto A, Kakuda T (2003) Heat-epimerized tea catechins rich in gallocatechin gallate and catechin gallate are more effective to inhibit cholesterol absorption than tea catechins rich in epigallocatechin gallate and epicatechin gallate. J Agric Food Chem 51(25):7303–7307
Hsu T, Kusumoto A, Abe K, Hosoda K, Kiso Y, Wang M, Yamamoto S (2006) Polyphenol-enriched oolong tea increases fecal lipid excretion. Eur J Clin Nutr 60(11):1330–1336
Westerterp-Plantenga MS (2010) Green tea catechins, caffeine and body-weight regulation. Physiol Behav 100(1):42–46
Rains TM, Agarwal S, Maki KC (2011) Antiobesity effects of green tea catechins: a mechanistic review. J Nutr Biochem 22(1):1–7
Henning SM, Fajardo-Lira C, Lee HW, Youssefian AA, Go VL, Heber D (2003) Catechin content of 18 teas and a green tea extract supplement correlates with the antioxidant capacity. Nutr Cancer 45(2):226–235
Noordzij M, Uiterwaal CS, Arends LR, Kok FJ, Grobbee DE, Geleijnse JM (2005) Blood pressure response to chronic intake of coffee and caffeine: a meta-analysis of randomized controlled trials. J Hypertens 23(5):921–928
Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, Kastelein JJP, Bittner V, Fruchart J-C, Treating New Targets I, Treating to New Targets I (2007) HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med 357(13):1301–1310. doi:10.1056/NEJMoa064278
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Khalesi, S., Sun, J., Buys, N. et al. Green tea catechins and blood pressure: a systematic review and meta-analysis of randomised controlled trials. Eur J Nutr 53, 1299–1311 (2014). https://doi.org/10.1007/s00394-014-0720-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-014-0720-1