Abstract
Background
Depression is common in patients after acute coronary syndromes (ACS) and with stable coronary artery disease (CAD) and has been associated with increased mortality and morbidity. However, it is unclear whether selective serotonin receptor inhibitors (SSRIs) reduce mortality or cardiac events in patients with CAD and depression.
Objective
We conducted a systematic review and meta-analysis to assess the effects of SSRIs on cardiovascular events in depressed CAD patients.
Methods
The CENTRAL, MEDLINE, and PsycINFO databases were searched (April 2020) for randomized controlled trials (RCTs) and extended follow-up analyses of RCTs that compared SSRIs with placebo or no intervention in patients with CAD and depression. The primary outcomes were all-cause mortality, cardiovascular mortality, and myocardial infarction incidence. The results were calculated through random-effect meta-analyses and reported in terms of risk ratio (RR) with 95% confidence intervals (CI).
Results
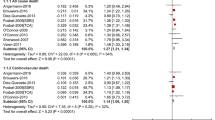
We retrieved 8 RCTs (2 of which with extended follow-up analyses), comprising a total of 1148 patients. 7 studies only included post-ACS patients. SSRIs were associated with a significantly lower risk of myocardial infarction in patients with CAD and depression (RR 0.54, 95% CI 0.34–0.86), and in post-ACS patients with depression (RR 0.56, 95% CI 0.35–0.90). We found no statistically significant difference in all-cause mortality, cardiovascular mortality, hospitalizations, angina, congestive heart failure, or stroke incidence.
Conclusion
The use of SSRIs in post-ACS patients with depression was associated with a 44% relative risk reduction of myocardial infarction. No difference in mortality was found. Given that the quality of the evidence was low, further research is warranted.


Similar content being viewed by others
Availability of data and material (data transparency)
Any missing dada or material used in this article will be made available to readers upon reasonable request.
Abbreviations
- 95% CI:
-
95% Confidence interval
- ACS:
-
Acute coronary syndrome
- AD:
-
Antidepressant
- BDI:
-
Beck's depression inventory
- CAD:
-
Coronary artery disease
- CHF:
-
Congestive heart failure
- DSM-III-R:
-
Diagnostic and Statistical Manual of Mental Disorders III R
- DSM-IV:
-
Diagnostic and Statistical Manual of Mental Disorders IV
- F:
-
Female
- FU:
-
Extended follow-up analysis of an RCT
- GRADE:
-
Grading of recommendations, assessment and evaluation
- HAMD-17:
-
17 Item Hamilton rating scale for depression
- HAM-D-24:
-
24 Item Hamilton rating scale for depression
- HDRS:
-
Hamilton depression rating scale
- HF:
-
Heart failure
- HR:
-
Heart rate
- IDD:
-
Inventory to diagnose depression
- IPT:
-
Interpersonal psychotherapy
- LVEF:
-
Left ventricle ejection fraction
- M:
-
Male
- MDD:
-
Major depressive disorder
- mDD:
-
Minor depressive disorder
- MI:
-
Myocardial infarction
- NSTEMI:
-
Non-ST elevation myocardial infarction
- P:
-
Placebo
- PCI:
-
Percutaneous coronary intervention
- RCT:
-
Randomized controlled trial
- RoB2:
-
Cochrane revised tool for risk of bias in randomized trials
- RR:
-
Risk ratio
- RRR:
-
Risk ratio reduction
- SCL-90 DS:
-
90-Item symptom check list depression scale
- SCL-90-R DS:
-
90-Item symptom check list revised depression subscale
- SDS:
-
Self-rating depression scale
- SSRI:
-
Selective serotonin reuptake inhibitor
- STEMI:
-
ST elevation myocardial infarction
- UA:
-
Unstable angina
References
Thombs BD, Bass EB, Ford DE et al (2006) Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med 21(1):30–38. https://doi.org/10.1111/j.1525-1497.2005.00269.x
Kang H-J, Stewart R, Bae K-Y et al (2015) Predictors of depressive disorder following acute coronary syndrome: Results from K-DEPACS and EsDEPACS. J Affect Disord 181:1–8. https://doi.org/10.1016/j.jad.2015.04.004
Amin AA, Jones AMH, Nugent K, Rumsfeld JS, Spertus JA (2006) The prevalence of unrecognized depression in patients with acute coronary syndrome. Am Heart J 152(5):928–934. https://doi.org/10.1016/j.ahj.2006.05.006
Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P (2011) Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry 33(3):203–216. https://doi.org/10.1016/j.genhosppsych.2011.02.007
Osler M, Mårtensson S, Wium-Andersen IK et al (2016) Depression after first hospital admission for acute coronary syndrome: a study of time of onset and impact on survival. Am J Epidemiol 183(3):218–226. https://doi.org/10.1093/aje/kwv227
Lichtman JH, Froelicher ES, Blumenthal JA et al (2014) Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation 129(12):1350–1369. https://doi.org/10.1161/CIR.0000000000000019
Vaccarino V, Badimon L, Bremner JD et al (2019) Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur Heart J. https://doi.org/10.1093/eurheartj/ehy913
Albus C, Waller C, Fritzsche K, Gunold H, Haass M, Hamann B, Kindermann I, Köllner V, Leithäuser B, Marx N, Meesmann M, Michal M, Ronel J, Scherer M, Schrader V, Schwaab B, Weber CS, Herrmann-Lingen C (2019) Significance of psychosocial factors in cardiology: update 2018. Clin Res Cardiol 108(11):1175–1196
Bush DE, Ziegelstein RC, Tayback M et al (2001) Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol 88(4):337–341. https://doi.org/10.1016/S0002-9149(01)01675-7
Frasure-Smith N, Lespérance F (2008) Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry 65(1):62. https://doi.org/10.1001/archgenpsychiatry.2007.4
Celano CM, Huffman JC (2011) Depression and cardiac disease. Cardiol Rev 19(3):130–142. https://doi.org/10.1097/CRD.0b013e31820e8106
Barth J, Schumacher M, Herrmann-Lingen C (2004) Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med 66(6):802–813. https://doi.org/10.1097/01.psy.0000146332.53619.b2
van Melle JP, de Jonge P, Spijkerman TA et al (2004) Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med 66(6):814–822. https://doi.org/10.1097/01.psy.0000146294.82810.9c
Kim J-MJ-WH, Stewart R, Lee Y-S et al (2018) Effect of escitalopram vs placebo treatment for depression on long-term cardiac outcomes in patients with acute coronary syndrome. JAMA 320(4):350. https://doi.org/10.1001/jama.2018.9422
Glassman AH, Bigger JT, Gaffney M (2009) Psychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression. Arch Gen Psychiatry 66(9):1022. https://doi.org/10.1001/archgenpsychiatry.2009.121
Smolderen KG, Buchanan DM, Gosch K et al (2017) Depression treatment and 1-year mortality after acute myocardial infarction. Circulation 135(18):1681–1689. https://doi.org/10.1161/CIRCULATIONAHA.116.025140
National Institute for Health and Clinical Excellence (2009) Depression: the treatment and management of depression in adults (update). (Clinical guideline 90). https://www.nice.org.uk/guidance/CG90. Accessed 21 May 2020
Lichtman JH, Bigger JT, Blumenthal JA et al (2008) Depression and coronary heart disease. Circulation 118(17):1768–1775. https://doi.org/10.1161/CIRCULATIONAHA.108.190769
Post-Myocardial Infarction Depression Clinical Practice Guideline Panel (2009) AAFP guideline for the detection and management of post-myocardial infarction depression. Ann Fam Med 7(1):71–79. https://doi.org/10.1370/afm.918
Thombs BD, de Jonge P, Coyne JC et al (2008) Depression screening and patient outcomes in cardiovascular care. JAMA 300(18):2161. https://doi.org/10.1001/jama.2008.667
Pizzi C, Rutjes AWS, Costa GM, Fontana F, Mezzetti A, Manzoli L (2011) Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am J Cardiol 107(7):972–979. https://doi.org/10.1016/j.amjcard.2010.11.017
Kim Y, Lee YS, Kim MG et al (2018) The effect of selective serotonin reuptake inhibitors on major adverse cardiovascular events. Int Clin Psychopharmacol. https://doi.org/10.1097/YIC.0000000000000238
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339(1):b2535–b2535. https://doi.org/10.1136/bmj.b2535
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. https://doi.org/10.1136/bmj.l4898
Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH (2012) Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. https://doi.org/10.18637/jss.v049.i05
Schünemann H, Brożek J, Guyatt G, Oxman A (eds) (2013) GRADE handbook for grading the quality of evidence and strength of recommendations. The GRADE Working Group. https://gdt.gradepro.org/app/handbook/handbook.html. Accessed 21 May 2020
GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2015 (developed by Evidence Prime, Inc.). Available from gradepro.org. Accessed 21 May 2020
Strik JJMH, Honig A, Lousberg R et al (2000) Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 62(6):783–789. https://doi.org/10.1097/00006842-200011000-00007
McFarlane A, Kamath MV, Fallen EL, Malcolm V, Cherian F, Norman G (2001) Effect of sertraline on the recovery rate of cardiac autonomic function in depressed patients after acute myocardial infarction. Am Heart J 142(4):617–623. https://doi.org/10.1067/mhj.2001.116766
Glassman AH (2002) Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 288(6):701. https://doi.org/10.1001/jama.288.6.701
Mohapatra PK, Kar N, Kar GC, Behera M (2005) Effectiveness of sertraline in treatment of depression in a consecutive sample of patients with acute myocardial infarction: six month prospective study on outcome. Clin Pract Epidemiol Ment Health 1:26. https://doi.org/10.1186/1745-0179-1-26
Kennedy S (University of TOC) (2006) Synopsis-study 10413: a double-blind, multicentre, randomised, parallel-group, placebo-controlled study assessing the efficacy and safety of escitalopram in post-myocardial infarction patients suffering from depressive symptoms. https://www.clinicaltrialsregister.eu/ctr-search/trial/2004-000990-78/results. Accessed 21 May 2020
Lespérance F, Frasure-Smith N, Koszycki D et al (2007) Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease. JAMA 297(4):367. https://doi.org/10.1001/jama.297.4.367
Kim J-M, Bae K-Y, Stewart R et al (2015) Escitalopram treatment for depressive disorder following acute coronary syndrome. J Clin Psychiatry 76(01):62–68. https://doi.org/10.4088/JCP.14m09281
Tian X, Wang Q, Guo R, Xu L, Chen QM, Hou Y (2016) Effects of paroxetine-mediated inhibition of GRK2 expression on depression and cardiovascular function in patients with myocardial infarction. Neuropsychiatr Dis Treat 12:2333–2341. https://doi.org/10.2147/NDT.S109880
Chittaranjan A, Chethan KB, Sandarsh S (2013) Cardiovascular mechanisms of SSRI drugs and their benefits and risks in ischemic heart disease and heart failure. Int Clin Psychopharmacol 28(3):145–155. https://doi.org/10.1097/YIC.0b013e32835d735d
Pizzi C, Santarella L, Bugiardini R (2014) Epidemiology and the physiopathological link between depression and cardiovascular disease. IJC Metab Endocr 5:52–55. https://doi.org/10.1016/j.ijcme.2014.10.004
Carvalho AF, Sharma MS, Brunoni AR, Vieta E, Fava GA (2016) The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: a critical review of the literature. Psychother Psychosom 85(5):270–288. https://doi.org/10.1159/000447034
Taylor CB (2005) Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry 62(7):792. https://doi.org/10.1001/archpsyc.62.7.792
Fang XY, Spieler D, Albarqouni L, Ronel J, Ladwig KH (2018) Impact of generalized anxiety disorder (GAD) on prehospital delay of acute myocardial infarction patients. Findings from the multicenter MEDEA study. Clin Res Cardiol 107(6):471–478. https://doi.org/10.1007/s00392-018-1208-4
Peikert A, Kaier K, Merz J, Manhart L, Schäfer I, Hilgendorf I, Hehn P, Wolf D, Willecke F, Sheng X, Clemens A, Zehender M, von Zur MC, Bode C, Zirlik A, Stachon P (2020) Residual inflammatory risk in coronary heart disease: incidence of elevated high-sensitive CRP in a real-world cohort. Clin Res Cardiol 109(3):315–323. https://doi.org/10.1007/s00392-019-01511-0
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JJF had speaker and consultant fees with Grünenthal, Fundação MSD (Portugal), TEVA, MSD, Allergan, Medtronic, GlaxoSmithKline, Novartis, Lundbeck, Solvay, BIAL, Merck-Serono, Merz, Ipsen, Biogen, Acadia, Allergan, Abbvie, Sunovion-Pharmaceuticals. FJP had consultant and speaker fees with Astra Zeneca, Bayer, BMS, Boehringer Ingelheim, and Daiichi Sankyo. DC has participated in educational meetings and/or attended conferences or symposia (including travel, accommodation, and/or hospitality) with Bristol-Myers Squibb, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Merck Serono, Ferrer, Pfizer, Novartis, and Roche. The remaining authors do not have interests to disclose.
Code availability
Not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fernandes, N., Prada, L., Rosa, M.M. et al. The impact of SSRIs on mortality and cardiovascular events in patients with coronary artery disease and depression: systematic review and meta-analysis. Clin Res Cardiol 110, 183–193 (2021). https://doi.org/10.1007/s00392-020-01697-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01697-8